Issue Archive
Table of Contents
BLOOD COMMENTARIES
REVIEW ARTICLE
Novel insights into Hodgkin lymphoma biology by single-cell analysis
Aoki and Steidl review the impact of single-cell technologies on the understanding of the heterogeneity of malignant cells and their microenvironment. Using classic Hodgkin lymphoma as a paradigm, the pair describe how single-cell sequencing and multiplexed imaging allows elucidation of the biology of a disease where a small number of tumor cells are embedded in a complex collection of nonmalignant cells in the tumor microenvironment.
CLINICAL TRIALS AND OBSERVATIONS
Central nervous system status is prognostic in T-cell acute lymphoblastic leukemia: a Children’s Oncology Group report
Clinical Trials & Observations
Gossai et al report on the prognostic implications of central nervous system (CNS) involvement in newly diagnosed T-cell acute lymphoblastic leukemia. Pooling data from 2 large trials with different regimens and divergent uses of CNS prophylaxis, the authors analyzed the impact of CNS-1 (no blasts), CNS-2 (0-5% blasts), and CNS-3 (>5% blasts) on outcomes. CNS-1 and CNS-2 have similar event-free survival (EFS) and overall survival (OS), whereas CNS-3 has inferior EFS and OS. Nelarabine improves survival in patients with CNS-3 in a regimen including CNS radioprophylaxis.
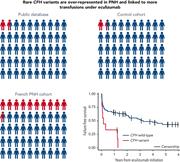
Rare germline complement factor H variants in patients with paroxysmal nocturnal hemoglobinuria
Clinical Trials & Observations
Brief Report
Paroxysmal nocturnal hemoglobinuria (PNH) is caused by somatic mutation of the PIGA gene, leading to a loss of erythrocyte complement inhibitory proteins and complement-mediated hemolysis. Prata and colleagues report on the surprising finding that patients with PNH also have a markedly increased prevalence of associated germline mutations in complement factor H (CFH), affecting both their clinical course and response to eculizumab. Patients with CFH variants had higher rates of transfusion, thrombosis, and poor response to eculizumab.
PNH and complement gene variants
Clinical Trials & Observations
IMMUNOBIOLOGY AND IMMUNOTHERAPY
Mechanisms of response and resistance to combined decitabine and ipilimumab for advanced myeloid disease
Clinical Trials & Observations
Two articles in this week’s issue focus on the use of ipilimumab and decitabine for patients with myelodysplasia (MDS) and acute myeloid leukemia (AML) before and after hematopoietic stem cell transplantation (HSCT) for high-risk disease. In the first article, Garcia et al report on the results of a phase 1 trial of the combination in 54 patients, demonstrating overall response rate of 52% in patients who are HSCT-naïve and 20% in patients post-HSCT; responses are usually short-lived. In the second article, Penter and colleagues characterize gene expression responses to therapy and conclude that decitabine acts directly to clear leukemic cells while ipilimumab acts on infiltrating lymphocytes in marrow and extramedullary sites. Responses are determined by leukemic cell burden and by the frequency and phenotype of infiltrating lymphocytes. Increasing bone marrow regulatory T cells is identified as a potential contributor to checkpoint inhibitor escape.
LYMPHOID NEOPLASIA
SBNO2 is a critical mediator of STAT3-driven hematological malignancies
MYELOID NEOPLASIA
Overlapping features of therapy-related and de novo NPM1-mutated AML
Clinical Trials & Observations
Therapy-related acute myeloid leukemia (t-AML) is viewed as carrying a poor prognosis; however, Othman et al demonstrate that prognosis for t-AML is actually quite heterogeneous, with isolated NPM1 mutation portending a good prognosis in both de novo AML and t-AML. NPM-mutated t-AML nearly always has a normal karyotype and is associated with DNMT3A and TET2 mutations, similar to the signature of de novo NPM-mutated AML. These data suggest that, unlike most t-AML, NPM-mutated t-AML should be viewed as comparable to de novo disease and should not be considered for early stem cell transplant.
RED CELLS, IRON, AND ERYTHROPOIESIS
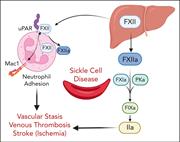
Factor XII contributes to thrombotic complications and vaso-occlusion in sickle cell disease
Sparkenbaugh and colleagues investigated the role of factor XII (FXII) in sickle cell disease (SCD)-related thrombo-inflammation. Patients with SCD have increased markers of activation of FXII and the contact pathway of coagulation. In the Townes mouse model of SCD, FXII contributes to thrombin generation and inflammation after challenge with TNFα, and FXII inhibition reduces venous thrombosis, congestion, and microvascular stasis. FXII inhibition may offer a novel approach to reducing thrombo-inflammation in SCD without incurring increased bleeding risk.
LETTERS TO BLOOD
Ipilimumab plus decitabine for patients with MDS or AML in posttransplant or transplant-naïve settings
Clinical Trials & Observations
Two articles in this week’s issue focus on the use of ipilimumab and decitabine for patients with myelodysplasia (MDS) and acute myeloid leukemia (AML) before and after hematopoietic stem cell transplantation (HSCT) for high-risk disease. In the first article, Garcia et al report on the results of a phase 1 trial of the combination in 54 patients, demonstrating overall response rate of 52% in patients who are HSCT-naïve and 20% in patients post-HSCT; responses are usually short-lived. In the second article, Penter and colleagues characterize gene expression responses to therapy and conclude that decitabine acts directly to clear leukemic cells while ipilimumab acts on infiltrating lymphocytes in marrow and extramedullary sites. Responses are determined by leukemic cell burden and by the frequency and phenotype of infiltrating lymphocytes. Increasing bone marrow regulatory T cells is identified as a potential contributor to checkpoint inhibitor escape.
Predictive value of staging PET/CT to detect bone marrow involvement and early outcomes in marginal zone lymphoma
Clinical Trials & Observations
BLOOD WORK
ERRATA
-
Cover Image
Cover Image
![issue cover]()
Visualization of increased platelet (green) and fibrin (red) deposition within a thrombus formed in the femoral vein of mice with sickle cell disease after electrolytic injury. Yellow indicates the overlay between the 2 colors. See the article by Sparkenbaugh et al on page 1871.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Back MatterBack Matter
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals









T-ALL in CNS-3 status needs improvement
Clinical Trials & Observations