Issue Archive
Table of Contents
EDITORIAL
BLOOD COMMENTARIES
PLENARY PAPER
The role of CD8+ T-cell clones in immune thrombocytopenia
CME
The importance of cytotoxic T cells has been recognized in chronic immune thrombocytopenia (ITP), yet how CD8+ T cells evolve and perpetuate chronic ITP is a mystery. This month’s CME article, a Plenary Paper by Malik and colleagues, demonstrates that in chronic ITP, there is clonal expansion of a particular subset of CD8+ T cells, known as terminally differentiated effector memory T cells, which persist over years, are more evident in refractory ITP, and are more prevalent when the platelet count is low. Furthermore, CD8+ T cells induce platelet activation and apoptosis in an antibody-independent mechanism for refractory thrombocytopenia that may be amenable to therapeutic targeting.
HOW I TREAT SERIES
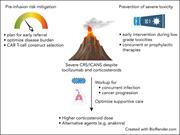
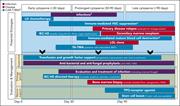
How I treat refractory CRS and ICANS after CAR T-cell therapy
Clinical Trials & Observations
With 6 chimeric antigen receptor (CAR) T-cell products approved by the US Food and Drug Administration and many more showing promise in clinical trials, the need for hematologists to be aware of challenging complications and know how to manage them in routine practice is paramount. Introduced by Associate Editor Helen E. Heslop, this How I Treat series highlights several key complications, reviews current understanding of their etiologies, and provides guidance on therapies through discussion of illustrative cases.
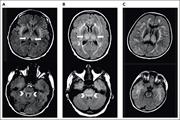
How I treat unique and difficult-to-manage cases of CAR T-cell therapy–associated neurotoxicity
Clinical Trials & Observations
With 6 chimeric antigen receptor (CAR) T-cell products approved by the US Food and Drug Administration and many more showing promise in clinical trials, the need for hematologists to be aware of challenging complications and know how to manage them in routine practice is paramount. Introduced by Associate Editor Helen E. Heslop, this How I Treat series highlights several key complications, reviews current understanding of their etiologies, and provides guidance on therapies through discussion of illustrative cases.
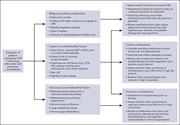
How I approach optimization of patients at risk of cardiac and pulmonary complications after CAR T-cell therapy
With 6 chimeric antigen receptor (CAR) T-cell products approved by the US Food and Drug Administration and many more showing promise in clinical trials, the need for hematologists to be aware of challenging complications and know how to manage them in routine practice is paramount. Introduced by Associate Editor Helen E. Heslop, this How I Treat series highlights several key complications, reviews current understanding of their etiologies, and provides guidance on therapies through discussion of illustrative cases.
How I treat cytopenias after CAR T-cell therapy
With 6 chimeric antigen receptor (CAR) T-cell products approved by the US Food and Drug Administration and many more showing promise in clinical trials, the need for hematologists to be aware of challenging complications and know how to manage them in routine practice is paramount. Introduced by Associate Editor Helen E. Heslop, this How I Treat series highlights several key complications, reviews current understanding of their etiologies, and provides guidance on therapies through discussion of illustrative cases.
CLINICAL TRIALS AND OBSERVATIONS
Dual targeting of CD19 and CD22 with bicistronic CAR-T cells in patients with relapsed/refractory large B-cell lymphoma
Clinical Trials & Observations
When targeting 1 cell surface antigen with chimeric antigen receptor (CAR) T cells results in durable efficacy in only a minority of patients with relapsed large B-cell lymphoma (LBCL), efforts to enhance antitumor responses are needed. Roddie and colleagues report on the results from a phase 1 trial designed to reduce failure by using a novel bicistronic anti-CD19 and CD22 dual-targeted autologous CAR T-cell product in combination with pembrolizumab. The data from 52 heavily pretreated patients with relapsed/refractory LBCL indicate durable remissions but only in a minority of patients, indicating that further technical advances in CAR T-cell design are necessary.
A new CAR takes a test drive in DLBCL
Clinical Trials & Observations
HEMATOPOIESIS AND STEM CELLS
Regeneration after blood loss and acute inflammation proceeds without contribution of primitive HSCs
How important are hematopoietic stem cells (HSCs) to the production of new blood cells in the face of acute emergencies? Using a murine reporter system that enables quantitation of HSC output in vivo without transplantation, Munz and colleagues show that regeneration following blood loss and acute inflammation proceeds without contribution of primitive HSCs, in contrast to situations where stresses are more prolonged, eg, cytotoxic chemotherapy. These data suggest that HSCs are a reserve population required for maintenance of long-term hematopoiesis and for restoration following severe myelosuppression.
LYMPHOID NEOPLASIA
Molecular determinants of clinical outcomes in a real-world diffuse large B-cell lymphoma population
Clinical Trials & Observations
Aggressive B-cell lymphomas are both molecularly and clinically heterogeneous, creating challenges for systems that attempt to classify them into clinically relevant entities. Alduaij et al advance the field by reporting on the utility of a dark zone signature (DZsig), originally identified in double-hit lymphoma in the diagnosis of aggressive B-cell lymphomas with diffuse large B-cell morphology. The authors show that DZsig has a strong negative prognostic value, and these analyses provide a direction for further refinement of current classifications of aggressive B-cell lymphomas.
MYELOID NEOPLASIA
CXCL8/CXCR2 signaling mediates bone marrow fibrosis and is a therapeutic target in myelofibrosis
Cytokines are known to be proinflammatory messengers in myeloproliferative neoplasms (MPNs) and are suspected to be important in the late stages of these diseases. Using primary human samples, single-cell cytokine profiling, and murine models, Dunbar and colleagues reveal that the CXCL8/CXCR2 cytokine-signaling axis is a key mediator of bone marrow fibrosis in MPN, providing a therapeutically tractable avenue to prevent, or treat, this lethal complication of MPN
RED CELLS, IRON, AND ERYTHROPOIESIS
Arginine metabolism regulates human erythroid differentiation through hypusination of eIF5A
LETTER TO BLOOD
BLOOD WORK
ERRATUM
CONTINUING MEDICAL EDUCATION (CME) QUESTIONS
-
Cover Image
Cover Image
![issue cover]()
Bone marrow reticulin staining from the hMPLW515L adoptive transfer mouse model of bone marrow fibrosis treated with ruxolitinib. See the article by Dunbar et al on page 2508.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals









TEMRA: the CD8 subset in chronic ITP?