Issue Archive
Table of Contents
BLOOD COMMENTARIES
REVIEW ARTICLE
Hot under the clot: venous thrombogenesis is an inflammatory process
Rayes and Brill provide an updated review of the interaction between inflammation and venous thrombosis (VT). The authors review preclinical models elucidating the role of inflammation in VT and discuss the potential of anti-inflammatory therapies as an adjunct to anticoagulation in treating VT.
CLINICAL TRIALS AND OBSERVATIONS
Human herpesvirus 6 reactivation and disease are infrequent in chimeric antigen receptor T-cell therapy recipients
Clinical Trials & Observations
Brief Report
Kampouri and colleagues report on human herpesvirus 6B (HHV-6B) reactivation and disease following chimeric antigen receptor (CAR) T-cell therapy. A prospective study of 89 patients tested weekly revealed reactivation in 6%, with low-level detection requiring no therapy. In a retrospective study of 626 patients, 24 had symptom-driven plasma testing, with 1 patient testing positive; in 34 patients receiving symptom-driven cerebrospinal fluid testing, 1 patient had HHV-6 that resolved without therapy, with a cumulative incidence of 0.17%. HHV-6B reactivation is infrequent following CAR T-cell therapy, suggesting routine testing is not indicated.
HEMATOPOIESIS AND STEM CELLS
Integrative single-cell chromatin and transcriptome analysis of human plasma cell differentiation
Alaterre and colleagues used single-cell RNA sequencing and assay for transposase-accessible chromatin with high throughput sequencing to elucidate the regulatory pathways governing plasma cell (PC) differentiation. The authors define a subset of preplasmablasts that are epigenetically committed to PC differentiation and provide a unique resource to probe further molecular pathways critical for PC biology.
LYMPHOID NEOPLASIA
T-bet suppresses proliferation of malignant B cells in chronic lymphocytic leukemia
The T-box transcription factor T-bet is an important regulator of T-cell development, but it is also expressed in B cells. Roessner et al describe a single-cell analysis of the role of T-bet in chronic lymphocytic leukemia (CLL) cells. The authors demonstrate that T-bet acts as a tumor suppressor in CLL cells through upregulation of interferon signaling, and elevated T-bet expression predicts a better prognosis in patients with CLL, suggesting it might be a novel target for CLL therapy.
Motive and opportunity: MYC rearrangements in high-grade B-cell lymphoma with MYC and BCL2 rearrangements (an LLMPP study)
“Double-hit” lymphomas (DHL) with both MYC and BCL2 rearrangements are aggressive and have a poor prognosis. MYC rearrangements in Burkitt lymphoma involve the immunoglobulin gene locus, but the rearrangements in lymphomas with concomitant BCL2 rearrangements are less well-defined. Hilton et al performed sequence analysis of rearrangements and demonstrated that the MYC rearrangements in DHL are distinct, selected for rearrangements that do not interrupt B-cell receptor (BCR) expression so that expression of both BCL2 and BCR is preserved.
MYELOID NEOPLASIA
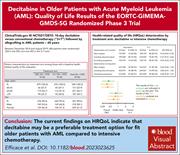
Decitabine in older patients with AML: quality of life results of the EORTC-GIMEMA-GMDS-SG randomized phase 3 trial
Clinical Trials & Observations
Efficace et al report health-related quality of life (HRQoL) in older patients with acute myeloid leukemia (AML) in a randomized trial of 606 patients, comparing decitabine (DEC) with intensive chemotherapy (IC) with consideration of subsequent allogeneic hematopoietic stem cell transplantation (HSCT). At 2 months, the risk of HRQoL deterioration was lower in the DEC arm than in the IC arm. These changes were not seen at 6 and 12 months. Before and after transplant, HRQoL deteriorated in both arms, with the deteriorations in the IC arm being more clinically meaningful. Since the trial outcomes reported no difference in survival or HSCT rates between the 2 arms, this suggests that DEC may be preferable to IC in fit older patients with AML.
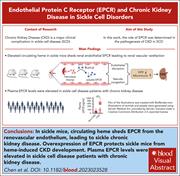
RED CELLS, IRON, AND ERYTHROPOIESIS
Heme-induced loss of renovascular endothelial protein C receptor promotes chronic kidney disease in sickle mice
Chronic kidney disease (CKD) is a leading cause of morbidity and mortality in sickle cell disease (SCD). Chen and colleagues delineate a novel pathophysiologic mechanism for SCD-CKD induced by hemolysis and free heme. Hemolysis leads to shedding of the vascular endothelial protein C receptor (EPCR) from the kidney, raising plasma soluble EPCR (sEPCR). Overexpression of EPCR in SCD mice protected from heme-induced CKD, while in patients with SCD, plasma sEPCR was higher in those with CKD. Restoration of EPCR may be a novel therapeutic target, and sEPCR may be a prognostic marker of CKD in SCD.
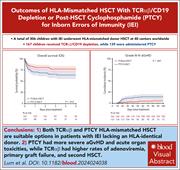
TRANSPLANTATION
Outcomes of HLA-mismatched HSCT with TCRαβ/CD19 depletion or post-HSCT cyclophosphamide for inborn errors of immunity
Clinical Trials & Observations
Lum et al performed a retrospective review of mismatched hematopoietic stem cell transplant (HSCT) for 306 children with inborn errors of immunity (IEIs), comparing posttransplant cyclophosphamide (PTCY) vs in vitro depletion of CD3+ T-cell receptor αβ/CD19 (TCRαβ) cells. TCRαβ depletion yielded better 3-year event-free survival and lower rates of acute graft-versus-host disease. PTCY was associated with higher rates of veno-occlusive disease, acute kidney injury, and pulmonary complications; TCRαβ depletion was associated with more adenoviremia, primary graft failure, and second HSCT. Further study is needed to determine which is the better approach in mismatched HSCT for IEIs.
LETTER TO BLOOD
BLOOD WORK
ERRATA
-
Cover Image
Cover Image
![issue cover]()
Immunofluorescence image illustrating chromatin accessibility in primary human plasmablasts, showing H3K27me3 histone modification levels (green) and DNA (red) in the nucleus. See the article by Alaterre et al on page 496.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals