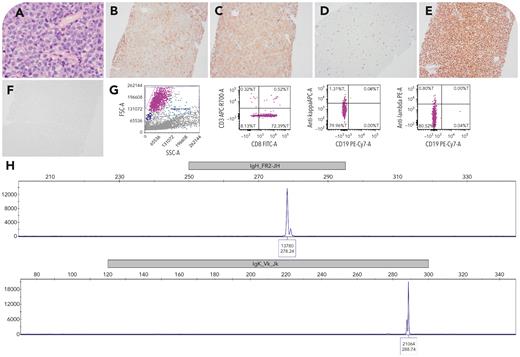
A 57-year-old woman with a long history of chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) presented with worsening lymphadenopathy. A lymph node biopsy showed diffuse infiltration of large lymphoid cells (panel A; 40× lens objective) with T-cell marker expression including CD7 (majority; panel B; 10× lens objective), CD8 (panel C; 10× lens objective), and partial CD5 (not shown) but negative CD3 (panel D; 10× lens objective) and B-cell marker expression including PAX5 (panel E; 10× lens objective) and CD79A (not shown) but negative CD20 (panel F; 10× lens objective). Atypical cells were also positive for CD23, BCL2, cMYC, BCL6, MUM1, κ in situ hybridization (ISH) and negative for CD2, CD22, CD30, CD138, ALK, TIA, granzyme B, EBER, λ ISH, with KI-67 ∼60%. Concurrent flow cytometry showed CD8- and CD45-positive lymphocytes negative for CD3, CD19, and surface immunoglobulin light chain (panel G). Review of the prior CLL/SLL specimen showed CD10 and CD20 positivity without CD7 or CD8 positivity. Clonal rearrangements of both immunoglobulin heavy and κ genes were detected (panel H), showing identical clones compared with the prior CLL/SLL specimen for this patient (not shown). T-cell receptor γ gene rearrangement was not detected.
This interesting case of Richter transformation to diffuse large B-cell lymphoma with aberrant T-cell marker expression highlights immunophenotypic variability, which can pose a diagnostic pitfall. Further workup confirming a B-cell neoplasm can guide appropriate treatment.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal