Issue Archive
Table of Contents
BLOOD COMMENTARIES
REVIEW SERIES
Defining and treating high-grade B-cell lymphoma, NOS
Edited by Associate Editor Laurie Sehn, this 3-part Review Series covers rare, aggressive B-cell lymphomas. First, Olszewski et al discuss a recently-designated new diagnostic category of “high-grade B-cell lymphoma, not otherwise specified (HBCL, NOS).” While lacking a cardinal molecular feature, they share a gene expression profile signature, and 45% have MYC rearrangement. Heterogeneity of HBCL, NOS has impeded treatment standardization, but new insights into molecular pathophysiology may offer entry points for better therapy. In the second article, Savage provides an updated review of primary mediastinal large B-cell lymphoma, highlighting its distinct molecular signature that overlaps with nodular sclerosis Hodgkin lymphoma, including JAK-STAT and NF-κB signaling pathways leading to immune evasion. Treatment outcomes are variable, but recent data confirming the efficacy of PD1 inhibitors have led to studies using immunotherapy in first-line therapy. In the third article, Schaff and Grommes review the clinical presentation, evaluation, and treatment of primary central nervous system lymphoma. They highlight improvement in outcomes with the use of high-dose methotrexate chemotherapy; however, survival at 5 years is only 30-40%. More recent studies of targeted therapies have had promising preliminary results.
Primary mediastinal large B-cell lymphoma
Edited by Associate Editor Laurie Sehn, this 3-part Review Series covers rare, aggressive B-cell lymphomas. First, Olszewski et al discuss a recently-designated new diagnostic category of “high-grade B-cell lymphoma, not otherwise specified (HBCL, NOS).” While lacking a cardinal molecular feature, they share a gene expression profile signature, and 45% have MYC rearrangement. Heterogeneity of HBCL, NOS has impeded treatment standardization, but new insights into molecular pathophysiology may offer entry points for better therapy. In the second article, Savage provides an updated review of primary mediastinal large B-cell lymphoma, highlighting its distinct molecular signature that overlaps with nodular sclerosis Hodgkin lymphoma, including JAK-STAT and NF-κB signaling pathways leading to immune evasion. Treatment outcomes are variable, but recent data confirming the efficacy of PD1 inhibitors have led to studies using immunotherapy in first-line therapy. In the third article, Schaff and Grommes review the clinical presentation, evaluation, and treatment of primary central nervous system lymphoma. They highlight improvement in outcomes with the use of high-dose methotrexate chemotherapy; however, survival at 5 years is only 30-40%. More recent studies of targeted therapies have had promising preliminary results.
Primary central nervous system lymphoma
Edited by Associate Editor Laurie Sehn, this 3-part Review Series covers rare, aggressive B-cell lymphomas. First, Olszewski et al discuss a recently-designated new diagnostic category of “high-grade B-cell lymphoma, not otherwise specified (HBCL, NOS).” While lacking a cardinal molecular feature, they share a gene expression profile signature, and 45% have MYC rearrangement. Heterogeneity of HBCL, NOS has impeded treatment standardization, but new insights into molecular pathophysiology may offer entry points for better therapy. In the second article, Savage provides an updated review of primary mediastinal large B-cell lymphoma, highlighting its distinct molecular signature that overlaps with nodular sclerosis Hodgkin lymphoma, including JAK-STAT and NF-κB signaling pathways leading to immune evasion. Treatment outcomes are variable, but recent data confirming the efficacy of PD1 inhibitors have led to studies using immunotherapy in first-line therapy. In the third article, Schaff and Grommes review the clinical presentation, evaluation, and treatment of primary central nervous system lymphoma. They highlight improvement in outcomes with the use of high-dose methotrexate chemotherapy; however, survival at 5 years is only 30-40%. More recent studies of targeted therapies have had promising preliminary results.
CLINICAL TRIALS AND OBSERVATIONS
Sutimlimab in patients with cold agglutinin disease: results of the randomized placebo-controlled phase 3 CADENZA trial
Clinical Trials & Observations
Röth and colleagues present results of a phase 3 trial of the C1s classical complement pathway inhibitor sutimlimab for the treatment of patients with cold agglutinin disease (CAD) who did not receive a transfusion within the previous 6 months. In a randomized placebocontrolled study of 41 patients, 73% of patients treated with sutimlimab required no transfusion or additional therapy, and treatment increased mean hemoglobin and fatigue scores, as compared to only 15% in the placebo arm. This supports sutimlimab as an important new agent for the treatment of CAD.
HEMATOPOIESIS AND STEM CELLS
LYMPHOID NEOPLASIA
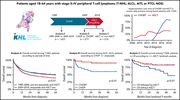
Impact of etoposide and ASCT on survival among patients aged <65 years with stage II to IV PTCL: a population-based cohort study
Clinical Trials & Observations
Brink et al report on a population-based analysis of 1427 patients in the Netherlands Cancer Registry with anaplastic large T-cell lymphoma, angioimmunoblastic T-cell lymphoma, and peripheral T-cell lymphoma not otherwise specified to assess the impacts on outcomes of the addition of etoposide to frontline chemotherapy and autologous stem cell transplantation (ASCT) as consolidation. ASCT yielded superior survival (81% vs 39% for patients who did not receive a transplant). No randomized trial data are available, but this retrospective analysis suggests that eligible patients should be considered for ASCT.
RED CELLS, IRON, AND ERYTHROPOIESIS
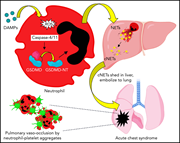
Liver-to-lung microembolic NETs promote gasdermin D–dependent inflammatory lung injury in sickle cell disease
Acute chest syndrome is a major cause of morbidity and mortality in sickle cell disease (SCD) and often occurs in the setting of a vasoocclusive crisis. Sundd et al demonstrated by intravital microscopy in murine SCD mice that inflammation promotes activation of neutrophil gasdermin D, which promotes shedding of neutrophil extracellular traps. Surprisingly, these form not in the lung but rather in the liver, from which they travel to the lung, inducing sterile inflammation.
THROMBOSIS AND HEMOSTASIS
Protein tyrosine phosphatase PTPN22 negatively modulates platelet function and thrombus formation
BLOOD WORK
-
Cover Image
Cover Image
![issue cover]()
Confocal image showing neutrophil extracellular traps in the liver of mice with sickle cell disease. Neutrophils (white), neutrophil elastase (red), and neutrophil-associated extracellular DNA strands (green) are highlighted. Colocalization of red and white appears pink. See the article by Vats et al on page 1020.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Back MatterBack Matter
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals





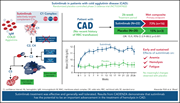



A virtuosic CADENZA played by sutimlimab
Clinical Trials & Observations