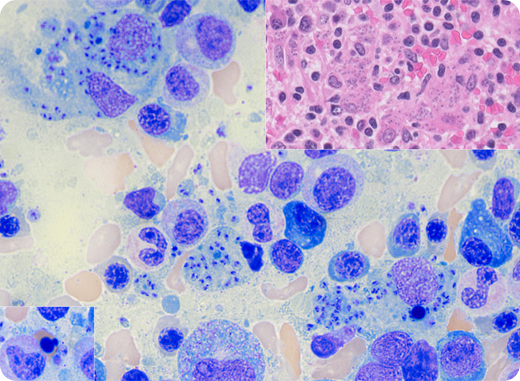
A 25-year-old previously healthy man presented to an outside clinic because he had experienced 6 weeks of left upper quadrant abdominal pain and new onset of fevers, headache, and watery diarrhea. He was admitted to an outside hospital and was found to have splenomegaly with splenic infarcts and pancytopenia (white blood cell count, 1.6 × 109/L; hemoglobin, 5.8 g/dL; platelet count, 60 × 109/L). A bone marrow biopsy reported findings of suspected myelodysplastic syndrome. Upon referral to our hospital, a repeat bone marrow biopsy identified numerous kinetoplast-containing organisms in the aspirate (central portion of figure: 100× lens objective, total magnification ×120; Wright-Giemsa stain) and biopsy (upper inset: intrahistiocytic organisms; 40× lens objective, total magnification ×400; hematoxylin and eosin stain), with only rare morphologic evidence of dysplasia with <10% nuclear dyserythropoiesis as shown in the lower inset (100× lens objective, total magnification ×120; Wright-Giemsa stain) and 46,XY karyotype. Fungal and gram stains were negative. DNA extracted from the aspirate and sequenced in-house was positive for Leishmania donovani complex. The patient’s history revealed that he had lived in the Oaxaca Mountains in Mexico for the past 3 years. He was promptly diagnosed with visceral leishmaniasis (VL) and was treated with liposomal amphotericin B with good response.
Symptomatic VL is a life-threatening parasitic infection that frequently presents with dyserythropoiesis and may be misdiagnosed as a hematologic disorder. Detailed travel history in addition to repeat microscopic examinations of bone marrow or suspected infected tissue is often required for definitive diagnosis.
A 25-year-old previously healthy man presented to an outside clinic because he had experienced 6 weeks of left upper quadrant abdominal pain and new onset of fevers, headache, and watery diarrhea. He was admitted to an outside hospital and was found to have splenomegaly with splenic infarcts and pancytopenia (white blood cell count, 1.6 × 109/L; hemoglobin, 5.8 g/dL; platelet count, 60 × 109/L). A bone marrow biopsy reported findings of suspected myelodysplastic syndrome. Upon referral to our hospital, a repeat bone marrow biopsy identified numerous kinetoplast-containing organisms in the aspirate (central portion of figure: 100× lens objective, total magnification ×120; Wright-Giemsa stain) and biopsy (upper inset: intrahistiocytic organisms; 40× lens objective, total magnification ×400; hematoxylin and eosin stain), with only rare morphologic evidence of dysplasia with <10% nuclear dyserythropoiesis as shown in the lower inset (100× lens objective, total magnification ×120; Wright-Giemsa stain) and 46,XY karyotype. Fungal and gram stains were negative. DNA extracted from the aspirate and sequenced in-house was positive for Leishmania donovani complex. The patient’s history revealed that he had lived in the Oaxaca Mountains in Mexico for the past 3 years. He was promptly diagnosed with visceral leishmaniasis (VL) and was treated with liposomal amphotericin B with good response.
Symptomatic VL is a life-threatening parasitic infection that frequently presents with dyserythropoiesis and may be misdiagnosed as a hematologic disorder. Detailed travel history in addition to repeat microscopic examinations of bone marrow or suspected infected tissue is often required for definitive diagnosis.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal