Issue Archive
Table of Contents
BLOOD COMMENTARIES
REVIEW ARTICLE
What’s new in the pathogenesis and treatment of therapy-related myeloid neoplasms
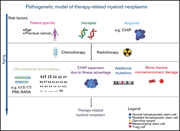
Voso et al review the current understanding of pathogenesis and treatment of t-MNs. They discuss the interplay of genomic variants, clonal hematopoiesis of indeterminate potential, aging, and other factors predisposing to acquisition of secondary mutations, especially in p53, in evolution to myeloid malignancy. They also describe new drugs and targeted agents that may improve the outcome on the terrible prognosis of t-MNs.
LYMPHOID NEOPLASIA
FoxO1-GAB1 axis regulates homing capacity and tonic AKT activity in chronic lymphocytic leukemia
14q32 rearrangements deregulating BCL11B mark a distinct subgroup of T-lymphoid and myeloid immature acute leukemia
Di Giacomo and colleagues describe a heterogeneous group of acute leukemias associated with 14q32/BCL11B rearrangements. Depending on the nature of the rearrangements, the translocations are associated with immature M0 or M1 acute myeloid leukemia, mixed-phenotype acute leukemia, and early T-cell precursor acute lymphoblastic leukemia. Nevertheless, all display a specific gene expression signature that distinguishes these cases from other immature leukemias.
MYELOID NEOPLASIA
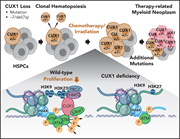
Loss of a 7q gene, CUX1, disrupts epigenetically driven DNA repair and drives therapy-related myeloid neoplasms
Imgruet et al investigated the role of the epigenetic modulator CUX1 in the pathogenesis of therapy-related myeloid neoplasms (t-MNs) in elegant in vitro and in vivo studies of mice with graded expression of CUX1. They demonstrate that CUX1 is critical for DNA repair and reduced CUX1 (as is commonly seen in t-MNs) leads to accumulation of DNA damage in cells that nevertheless continue to proliferate. In this model of t-MNs, restoring CUX1 reduces transformation, offering a possible entry point for preventing progression of clonal hematopoiesis to t-MNs.
PHAGOCYTES, GRANULOCYTES, AND MYELOPOIESIS
Upregulated PD-L1 delays human neutrophil apoptosis and promotes lung injury in an experimental mouse model of sepsis
Brief Report
PD-L1, the ligand for PD-1, has been demonstrated to be upregulated in neutrophils in sepsis. Wang et al report that neutrophil PD-L1 complexes with PI3 kinase to delay neutrophil apoptosis, enhancing neutrophil survival, and contributes to prolonging inflammation. PD-L1 inhibition is a candidate for reducing inflammation in the setting of inflammatory disease and sepsis.
LETTERS TO BLOOD
Impaired humoral responses to COVID-19 vaccination in patients with lymphoma receiving B-cell–directed therapies
Clinical Trials & Observations
Following a similar report on multiple myeloma, Ghione and colleagues report the expected observation that patients with non-Hodgkin lymphoma (NHL) receiving anti-B cell therapies have markedly reduced antibody responses to COVID-19 immunization. Although there is no information regarding T-cell immunity, this suggests that while vaccination is certainly still recommended for this population, patients should be strongly encouraged to maintain social distancing precautions and should be revaccinated after an appropriate interval from the end of their antilymphoma therapy.
Preanalytic depletion of medicinal anti-CD38 antibody from patient plasma for immunohematology testing
Monoclonal antibodies such as daratumumab that target antigens that are also expressed on red blood cells impede blood group typing. The preferred approach to potential transfusion is to do prior extensive antigen typing of patients' red cells; however, this is not always possible. Ehrend et al describe a technique for absorbing the antibodies from serum to allow accurate red cell typing for transfusion.
BLOOD WORK
-
Cover Image
Cover Image
![issue cover]()
This image from the spleen of a Cux1 knockdown mouse with a therapy-related erythroleukemia demonstrates extensive erythroblast infiltration with effacement of normal splenic architecture as shown by GATA1 immunohistochemistry (4×). See the article by Imgruet et al on page 790.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Back MatterBack Matter
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals






BCL11B, the Cerberus of human leukemia