Key Points
Biomarker scores generated after 1 week of steroid treatment of GVHD are prognostic.
Biomarkers reflect prognosis better than early clinical response to GVHD treatment.
Abstract
Acute graft-versus-host disease (GVHD) is treated with systemic corticosteroid immunosuppression. Clinical response after 1 week of therapy often guides further treatment decisions, but long-term outcomes vary widely among centers, and more accurate predictive tests are urgently needed. We analyzed clinical data and blood samples taken 1 week after systemic treatment of GVHD from 507 patients from 17 centers of the Mount Sinai Acute GVHD International Consortium (MAGIC), dividing them into a test cohort (n = 236) and 2 validation cohorts separated in time (n = 142 and n = 129). Initial response to systemic steroids correlated with response at 4 weeks, 1-year nonrelapse mortality (NRM), and overall survival (OS). A previously validated algorithm of 2 MAGIC biomarkers (ST2 and REG3α) consistently separated steroid-resistant patients into 2 groups with dramatically different NRM and OS (P < .001 for all 3 cohorts). High biomarker probability, resistance to steroids, and GVHD severity (Minnesota risk) were all significant predictors of NRM in multivariate analysis. A direct comparison of receiver operating characteristic curves showed that the area under the curve for biomarker probability (0.82) was significantly greater than that for steroid response (0.68, P = .004) and for Minnesota risk (0.72, P = .005). In conclusion, MAGIC biomarker probabilities generated after 1 week of systemic treatment of GVHD predict long-term outcomes in steroid-resistant GVHD better than clinical criteria and should prove useful in developing better treatment strategies.
Medscape Continuing Medical Education online

In support of improving patient care, this activity has been planned and implemented by Medscape, LLC and the American Society of Hematology. Medscape, LLC is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1.00 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 75% minimum passing score and complete the evaluation at http://www.medscape.org/journal/blood; and (4) view/print certificate. For CME questions, see page 2870.
Disclosures
CME questions author Laurie Barclay, freelance writer and reviewer, Medscape, LLC, owns stock, stock options, or bonds from Pfizer. Authors Umut Özbek, James L. M. Ferrara, and John E. Levine are joint inventors on a graft-versus-host disease biomarker patent. Associate Editor Robert Zeiser and the remaining authors declare no competing financial interests.
Learning objectives
Upon completion of this activity, participants will be able to:
Describe the prognostic value of biomarker scores and clinical features after 1 week of steroid treatment for graft-versus-host disease (GVHD), based on a clinical study
Compare the prognostic value of these biomarker scores with that of early clinical response to GVHD treatment
Determine the clinical implications of the prognostic value of biomarker scores generated after 1 week of steroid treatment for GVHD
Release date: June 21, 2018; Expiration date: June 21, 2019
Introduction
Improvements in survival following allogeneic hematopoietic cell transplantation (HCT) have led to its increasing use to cure hematologic malignancies and other disorders,1 but the leading cause of nonrelapse mortality (NRM) after HCT remains graft-versus-host disease (GVHD).2,3 Many patients do not respond to primary therapy, high-dose systemic corticosteroids; therefore, survival for patients with treatment-resistant GVHD remains particularly poor.4 The clinical response after 4 weeks of treatment is a validated surrogate for long-term survival,5 but physicians usually cannot wait 1 month before deciding whether to modify therapy, particularly for patients who do not achieve or maintain a convincing clinical response. In clinical practice, 1 week of treatment is commonly used to determine escalation or de-escalation of immunosuppressive therapy, but this early response correlates poorly with long-term outcomes.6 Patient who do not respond early to systemic steroids have a generally poor prognosis, but results are inconsistent among transplant centers, and biomarkers that accurately predict long-term outcomes in this highly immunosuppressed population are urgently needed.
The Mount Sinai Acute GVHD International Consortium (MAGIC) comprises 17 HCT centers and was established to provide consistent multicenter monitoring of acute GVHD severity during treatment, as well as to obtain samples that could be interrogated for potential predictive biomarkers. We have previously validated an algorithm that uses the serum concentrations of the GVHD biomarkers suppressor of tumorigenicity-2 (ST2) and regenerating islet-derived protein 3-α (REG3α) to generate a probability for NRM and predict resistance to treatment.7,8 In this study, we first determined the extent to which early clinical responses to steroid treatment could predict long-term outcome of patients with acute GVHD. We then evaluated biomarkers obtained at the time of the clinical evaluation. We hypothesized that the probabilities would predict long-term outcomes, even if the biomarkers are measured at a time when the initial response to treatment was already known.
Methods
Study design
Patients from the 17 centers in MAGIC underwent their first allogeneic HCT between May 2001 and December 2016 and provided blood samples for a biorepository 7 days after initiation of corticosteroid treatment for newly diagnosed acute GVHD. All patients consented to participation in an Institutional Review Board–approved protocol at each MAGIC center (supplemental Table 1, available on the Blood Web site). Patients transplanted before 2016 whose data and GVHD-onset samples had contributed to the development of the initial algorithm formed the test cohort (n = 236),7,8 whereas patients not previously analyzed formed the first validation cohort (n = 142). Patients transplanted in 2016 (n = 129) formed the second validation cohort.
GVHD was staged using published guidelines.9 MAGIC centers were trained via webinar in the use of these guidelines, and data entry personnel needed to pass a GVHD staging test prior to enrolling patients in the MAGIC protocol. GVHD staging guidance was reinforced in monthly webinars.
Nonrelapse deaths were considered related to GVHD only if the patient died of GVHD itself or from an infection that developed while receiving systemic steroids (≥10 mg of prednisone daily or equivalent) for the treatment of GVHD. Noninfectious contributing causes of death from GVHD included cardiac and pulmonary events, multiorgan failure, and hemorrhage. Clinical response to treatment was determined at 1 and 4 weeks after the start of treatment, according to published criteria.10 Complete response (CR) was defined as the complete resolution of acute GVHD manifestations in all organs. Partial response (PR) was defined as improvement, but not complete resolution, of GVHD in all initially affected organs without new target organ involvement. Nonresponse was defined as all other responses or death before response assessment. Relapse risk was assessed according to published criteria.11
Biomarker determination and statistical analyses
Samples were shipped to a central laboratory where they were analyzed in batches for ST2 and REG3α by enzyme-linked immunosorbent assay, as previously described.12,13 We then created a competing risks model, with relapse as the competing risk, that predicted 6-month NRM after 1 week of systemic GVHD treatment using the concentrations of ST2 and REG3α. We compared the performance of this model with the previously published MAGIC prediction model by calculating the area under the curve (AUC) of the receiver operating characteristic curve of each model in the validation cohort. The AUC was the same for both models (0.82, P = .977); therefore, we used the previously published MAGIC prediction model log[−log(1–p̂)] = −11.263 + 1.844(log10ST2) + 0.577(log10REG3α) to calculate the probability value (p̂) for each patient.8 An unsupervised learning algorithm, K-medoids clustering, which maximized the differences between groups while minimizing the differences in probabilities within each group, was used to identify the threshold that best separated test cohort patients into 2 groups.14
Clinical characteristics of patients between cohorts were compared using the χ2 or Wilcoxon rank-sum test, as appropriate. Competing risks regression, with relapse as the competing risk, was used to model 1-year NRM, with early treatment response, clinical severity (Minnesota risk staging),10 and biomarkers as predictors. Patients with complete resolution of GVHD symptoms after 1 week of treatment were assigned to Minnesota standard risk. Logistic regression was used to model week 4 resistance to treatment. Differences in the cumulative incidence of NRM and relapse between groups were calculated by the Gray test. OS was estimated by the Kaplan-Meier method, and differences between groups were calculated using the log-rank test. Areas under the receiver operating characteristic curves were compared using the DeLong method.15 Univariate analyses for NRM were performed on the combined validation cohort patients and included pretransplant characteristics that are important risk factors for GVHD (Table 1), clinical severity after 1 week of treatment, initial response to treatment, and either biomarker concentrations or the categorical variable of the probability group. Multivariate analyses included all variables that are risk factors for GVHD and that were statistically significant on univariate analysis and were performed on the combined validation cohort patients. All analyses were performed using R statistical package version 3.4.0 (R Development Core Team 2017). Error bars represent the standard error of proportion in all figures in which error bars are shown.
Patient characteristics
| Characteristic . | Test cohort (n = 236) . | Validation cohort 1 (n = 142) . | Validation cohort 2 (n = 129) . | P . |
|---|---|---|---|---|
| Median age, y (range) | 51 (1-73) | 49.5 (1-74) | 48 (1-74) | .840 |
| Indication for HCT, n (%) | .004 | |||
| Acute leukemia | 121 (51.3) | 73 (51.4) | 65 (50.4) | |
| MDS/MPN | 48 (20.3) | 24 (16.9) | 43 (33.2) | |
| Lymphoma | 38 (16.1) | 19 (13.4) | 6 (4.7) | |
| Other malignant | 22 (9.3) | 20 (14.1) | 9 (7.0) | |
| Nonmalignant | 7 (3.0) | 6 (4.2) | 6 (4.7) | |
| Disease risk index at HCT, n (%) | .326 | |||
| Low | 16 (6.8) | 7 (4.9) | 3 (2.3) | |
| Intermediate | 120 (50.8) | 78 (54.9) | 81 (62.8) | |
| High | 61 (25.8) | 38 (26.8) | 31 (24.0) | |
| Very high | 20 (8.5) | 7 (4.9) | 8 (6.2) | |
| Unknown | 19 (8.1) | 12 (8.5) | 6 (4.7) | |
| Donor type, n (%) | .529 | |||
| Related | 67 (28.4) | 46 (32.4) | 34 (26.4) | |
| Unrelated | 169 (71.6) | 96 (67.6) | 95 (73.6) | |
| HLA match, n (%) | .485 | |||
| Matched | 159 (67.4) | 95 (66.9) | 94 (72.9) | |
| Mismatched | 77 (32.6) | 47 (33.1) | 35 (27.1) | |
| Stem cell source, n (%) | .433 | |||
| Marrow | 36 (15.3) | 30 (21.1) | 19 (14.7) | |
| Peripheral blood | 179 (75.8) | 104 (73.2) | 101 (78.3) | |
| Cord blood | 21 (8.9) | 8 (5.7) | 9 (7.0) | |
| Conditioning regimen intensity, n (%) | .007 | |||
| Full | 194 (82.2) | 104 (73.2) | 88 (68.2) | |
| Reduced | 42 (17.8) | 38 (26.8) | 41 (31.8) | |
| Antithymocyte globulin in conditioning, n (%) | .0001 | |||
| Yes | 58 (24.6) | 30 (21.1) | 55 (42.6) | |
| No | 178 (75.4) | 112 (78.9) | 74 (57.4) | |
| GVHD prophylaxis, n (%) | .024 | |||
| CNI/MTX ± other | 144 (61.0) | 84 (59.2) | 61 (47.3) | |
| CNI/MMF ± other | 77 (32.6) | 47 (33.1) | 47 (36.4) | |
| CNI/sirolimus | 1 (0.4) | 0 (0) | 2 (1.6) | |
| Posttransplant cyclophosphamide ± other | 8 (3.4) | 9 (6.3) | 13 (10) | |
| T-cell depleted | 2 (0.9) | 0 (0) | 2 (1.6) | |
| Other | 4 (1.7) | 2 (1.4) | 4 (3.1) | |
| Onset GVHD: median day (range) | 26 (9-275) | 31 (7-204) | 26 (8-180) | .0005 |
| Onset GVHD: organ distribution, n (%) | .891 | |||
| Isolated skin | 116 (49.2) | 67 (47.2) | 68 (52.7) | |
| Isolated GI (upper and/or lower) | 63 (26.7) | 39 (27.5) | 34 (26.3) | |
| Isolated liver | 2 (0.8) | 3 (2.1) | 2 (1.6) | |
| ≥2 organs involved | 55 (23.3) | 33 (23.2) | 25 (19.4) | |
| Onset GVHD grade, n (%) | .112 | |||
| 1 | 73 (30.9) | 39 (27.5) | 51 (39.6) | |
| 2 | 105 (44.5) | 64 (45.1) | 57 (44.2) | |
| 3 | 50 (21.2) | 31 (21.8) | 14 (10.8) | |
| 4 | 8 (3.4) | 8 (5.6) | 7 (5.4) | |
| Minnesota risk score (onset), n (%) | .016 | |||
| Standard | 183 (77.5) | 107 (75.4) | 114 (88.4) | |
| High | 53 (22.5) | 35 (24.6) | 15 (11.6) | |
| Week 1 response, n (%) | .674 | |||
| CR or PR | 114 (48.3) | 62 (43.7) | 61 (47.3) | |
| Nonresponse | 122 (51.7) | 80 (56.3) | 68 (52.7) | |
| Minnesota risk score (week 1), n (%) | .045 | |||
| Standard | 187 (79.2) | 110 (77.5) | 114 (88.4) | |
| High | 49 (20.8) | 32 (22.5) | 15 (11.6) | |
| Long-term outcomes by cohort, % | ||||
| 1-year NRM | 31.3 | 28.9 | 20.5 | .084 |
| 1-year relapse rate | 20.3 | 16.3 | 8.9 | .030 |
| 1-year OS | 56.9 | 59.8 | 72.2 | .019 |
| Characteristic . | Test cohort (n = 236) . | Validation cohort 1 (n = 142) . | Validation cohort 2 (n = 129) . | P . |
|---|---|---|---|---|
| Median age, y (range) | 51 (1-73) | 49.5 (1-74) | 48 (1-74) | .840 |
| Indication for HCT, n (%) | .004 | |||
| Acute leukemia | 121 (51.3) | 73 (51.4) | 65 (50.4) | |
| MDS/MPN | 48 (20.3) | 24 (16.9) | 43 (33.2) | |
| Lymphoma | 38 (16.1) | 19 (13.4) | 6 (4.7) | |
| Other malignant | 22 (9.3) | 20 (14.1) | 9 (7.0) | |
| Nonmalignant | 7 (3.0) | 6 (4.2) | 6 (4.7) | |
| Disease risk index at HCT, n (%) | .326 | |||
| Low | 16 (6.8) | 7 (4.9) | 3 (2.3) | |
| Intermediate | 120 (50.8) | 78 (54.9) | 81 (62.8) | |
| High | 61 (25.8) | 38 (26.8) | 31 (24.0) | |
| Very high | 20 (8.5) | 7 (4.9) | 8 (6.2) | |
| Unknown | 19 (8.1) | 12 (8.5) | 6 (4.7) | |
| Donor type, n (%) | .529 | |||
| Related | 67 (28.4) | 46 (32.4) | 34 (26.4) | |
| Unrelated | 169 (71.6) | 96 (67.6) | 95 (73.6) | |
| HLA match, n (%) | .485 | |||
| Matched | 159 (67.4) | 95 (66.9) | 94 (72.9) | |
| Mismatched | 77 (32.6) | 47 (33.1) | 35 (27.1) | |
| Stem cell source, n (%) | .433 | |||
| Marrow | 36 (15.3) | 30 (21.1) | 19 (14.7) | |
| Peripheral blood | 179 (75.8) | 104 (73.2) | 101 (78.3) | |
| Cord blood | 21 (8.9) | 8 (5.7) | 9 (7.0) | |
| Conditioning regimen intensity, n (%) | .007 | |||
| Full | 194 (82.2) | 104 (73.2) | 88 (68.2) | |
| Reduced | 42 (17.8) | 38 (26.8) | 41 (31.8) | |
| Antithymocyte globulin in conditioning, n (%) | .0001 | |||
| Yes | 58 (24.6) | 30 (21.1) | 55 (42.6) | |
| No | 178 (75.4) | 112 (78.9) | 74 (57.4) | |
| GVHD prophylaxis, n (%) | .024 | |||
| CNI/MTX ± other | 144 (61.0) | 84 (59.2) | 61 (47.3) | |
| CNI/MMF ± other | 77 (32.6) | 47 (33.1) | 47 (36.4) | |
| CNI/sirolimus | 1 (0.4) | 0 (0) | 2 (1.6) | |
| Posttransplant cyclophosphamide ± other | 8 (3.4) | 9 (6.3) | 13 (10) | |
| T-cell depleted | 2 (0.9) | 0 (0) | 2 (1.6) | |
| Other | 4 (1.7) | 2 (1.4) | 4 (3.1) | |
| Onset GVHD: median day (range) | 26 (9-275) | 31 (7-204) | 26 (8-180) | .0005 |
| Onset GVHD: organ distribution, n (%) | .891 | |||
| Isolated skin | 116 (49.2) | 67 (47.2) | 68 (52.7) | |
| Isolated GI (upper and/or lower) | 63 (26.7) | 39 (27.5) | 34 (26.3) | |
| Isolated liver | 2 (0.8) | 3 (2.1) | 2 (1.6) | |
| ≥2 organs involved | 55 (23.3) | 33 (23.2) | 25 (19.4) | |
| Onset GVHD grade, n (%) | .112 | |||
| 1 | 73 (30.9) | 39 (27.5) | 51 (39.6) | |
| 2 | 105 (44.5) | 64 (45.1) | 57 (44.2) | |
| 3 | 50 (21.2) | 31 (21.8) | 14 (10.8) | |
| 4 | 8 (3.4) | 8 (5.6) | 7 (5.4) | |
| Minnesota risk score (onset), n (%) | .016 | |||
| Standard | 183 (77.5) | 107 (75.4) | 114 (88.4) | |
| High | 53 (22.5) | 35 (24.6) | 15 (11.6) | |
| Week 1 response, n (%) | .674 | |||
| CR or PR | 114 (48.3) | 62 (43.7) | 61 (47.3) | |
| Nonresponse | 122 (51.7) | 80 (56.3) | 68 (52.7) | |
| Minnesota risk score (week 1), n (%) | .045 | |||
| Standard | 187 (79.2) | 110 (77.5) | 114 (88.4) | |
| High | 49 (20.8) | 32 (22.5) | 15 (11.6) | |
| Long-term outcomes by cohort, % | ||||
| 1-year NRM | 31.3 | 28.9 | 20.5 | .084 |
| 1-year relapse rate | 20.3 | 16.3 | 8.9 | .030 |
| 1-year OS | 56.9 | 59.8 | 72.2 | .019 |
CNI, calcineurin inhibitor; GI, gastrointestinal; MMF; mycophenolic acid; MTX, methotrexate.
Results
Patient characteristics
Clinical data and samples were available from 507 patients with acute GVHD who were treated with systemic corticosteroids. Patients were divided into a test cohort (n = 236) and 2 validation cohorts (n = 142 and n = 129). The median starting dose of steroids was 2.0 mg/kg per day for patients with grade 2-4 disease and 1.0 mg/kg per day for grade 1 disease. All GVHD treatments are listed in supplemental Table 2.
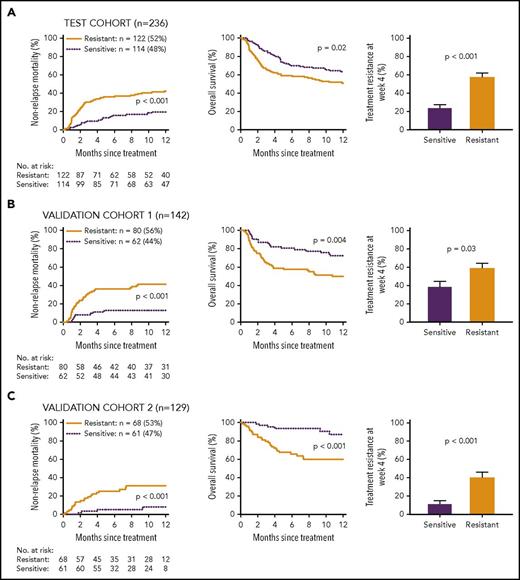
Clinical response after 1 week of treatment predicts outcomes
Because the clinical response after 1 week of systemic steroid treatment often guides further treatment,16,17 we first determined whether clinical response alone could predict NRM at 1 year. Patients with CRs and PRs in the test cohort had similar NRM (supplemental Figure 1), and we categorized these patients as early treatment sensitive, whereas all other patients were categorized as early treatment resistant. NRM at 1 year was significantly higher in patients with early treatment resistance (Figure 1A). Relapse did not consistently correlate with response (supplemental Table 3), with the result that the early treatment resistance group experienced significantly worse OS (Figure 1A). Some early treatment–resistant patients eventually showed responses to treatment by 4 weeks, an important surrogate end point for long-term outcomes,5,6,18 but most early treatment–resistant patients remained resistant at 4 weeks. Similarly, a significant minority of early treatment–sensitive patients became resistant to treatment at 4 weeks. Results were the same in both validation cohorts, demonstrating that the response to systemic steroids at 1 week can reliably predict long-term outcomes (Figure 1B-C).
Long-term outcomes by clinical response to 1 week of treatment in all patients. Patients were divided into 2 groups based on response to treatment: early treatment sensitive (ETS; dotted line) and early treatment resistant (ETR; solid line). (A) Test cohort (n = 236). Twelve-month cumulative incidence of NRM (ETS 20% vs ETR 42%, P < .001) and OS (ETS 63% vs ETR 51%, P = .02) and proportion of patients resistant to treatment at week 4 (ETS 24% vs ETR 57%, P < .001). (B) Validation cohort 1 (n = 142). Twelve-month cumulative incidence of NRM (ETS 13% vs ETR 41%, P < .001) and OS (ETS 72% vs ETR 50%, P = .004) and proportion of patients resistant to treatment at week 4 (ETS 39% vs ETR 59%, P = .03). (C) Validation cohort 2 (n = 129). Twelve-month cumulative incidence of NRM (ETS 8% vs ETR 31%, P = .001) and OS (ETS 87% vs ETR 60%, P < .001) and proportion of patients resistant to treatment at week 4 (ETS 11% vs ETR 41%, P < .001).
Long-term outcomes by clinical response to 1 week of treatment in all patients. Patients were divided into 2 groups based on response to treatment: early treatment sensitive (ETS; dotted line) and early treatment resistant (ETR; solid line). (A) Test cohort (n = 236). Twelve-month cumulative incidence of NRM (ETS 20% vs ETR 42%, P < .001) and OS (ETS 63% vs ETR 51%, P = .02) and proportion of patients resistant to treatment at week 4 (ETS 24% vs ETR 57%, P < .001). (B) Validation cohort 1 (n = 142). Twelve-month cumulative incidence of NRM (ETS 13% vs ETR 41%, P < .001) and OS (ETS 72% vs ETR 50%, P = .004) and proportion of patients resistant to treatment at week 4 (ETS 39% vs ETR 59%, P = .03). (C) Validation cohort 2 (n = 129). Twelve-month cumulative incidence of NRM (ETS 8% vs ETR 31%, P = .001) and OS (ETS 87% vs ETR 60%, P < .001) and proportion of patients resistant to treatment at week 4 (ETS 11% vs ETR 41%, P < .001).
Biomarker stratification
We have recently shown that serum biomarker concentrations can be used to predict long-term outcomes of patients at the onset of GVHD.7,8 We hypothesized that an algorithm of the same 2 biomarkers, ST2 and REG3α, would predict long-term outcomes when measured in patients after 1 week of treatment, when the early clinical response was already known. Because the accuracy of the newly derived algorithm was the same as the previously validated algorithm (see “Methods”), we used the original algorithm in all of our analyses. We first determined whether patients could be segregated into 2 groups (low and high probability) based only on the predicted probabilities of NRM generated by the biomarker algorithm and without reference to any known clinical characteristics or outcomes (see “Methods”). A threshold of p̂ ≤ 0.291 best separated patients into groups with low probability (n = 143, 61%) and high probability (n = 93, 39%) (supplemental Figure 2).
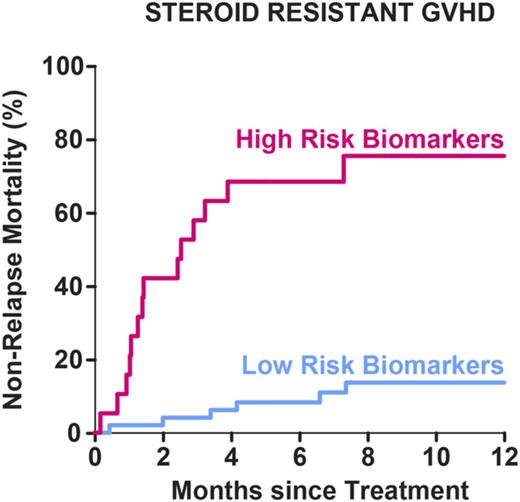
Biomarkers predict NRM within response groups
We evaluated the long-term outcomes of early treatment–resistant patients by their probability status. The algorithm analysis identified an unexpectedly large proportion (48%-72%) of the early treatment–resistant patients as low probability and who experienced strikingly less NRM than the high-probability group in all 3 cohorts (Figure 2). Relapse was not consistently different between probability groups (supplemental Table 3), resulting in dramatically better OS in the low-probability group that was similar to that of steroid-sensitive patients. Low-probability patients were also significantly less likely to remain resistant to treatment at week 4 compared with high-probability patients. As expected, GVHD was the leading cause of death in early treatment–resistant patients (supplemental Table 4).
Long-term outcomes by biomarker probabilities in early treatment–resistant patients. Early treatment–resistant patients were subdivided based on biomarker probabilities into low and high groups. (A) Test cohort of patients (n = 122). Twelve-month cumulative incidence of NRM (low 22% vs high 63%, P < .001) and OS (low 68% vs high 34%, P < .001) and proportion of patients resistant to treatment at week 4 (low 33% vs high 82%, P < .001). (B) Validation cohort 1 (n = 80). Twelve-month cumulative incidence of NRM (low 13% vs high 67%, P < .001) and OS (low 76% vs high 26%, P < .001) and proportion of patients resistant to treatment at week 4 (low 45% vs high 71%, P = .03). (C) Validation cohort 2 (n = 68). Twelve-month cumulative incidence of NRM (low 14% vs high 75%, P < .001) and OS (low 78% vs high 14%, P < .001) and proportion of patients resistant to treatment at week 4 (low 29% vs high 68%, P = .004).
Long-term outcomes by biomarker probabilities in early treatment–resistant patients. Early treatment–resistant patients were subdivided based on biomarker probabilities into low and high groups. (A) Test cohort of patients (n = 122). Twelve-month cumulative incidence of NRM (low 22% vs high 63%, P < .001) and OS (low 68% vs high 34%, P < .001) and proportion of patients resistant to treatment at week 4 (low 33% vs high 82%, P < .001). (B) Validation cohort 1 (n = 80). Twelve-month cumulative incidence of NRM (low 13% vs high 67%, P < .001) and OS (low 76% vs high 26%, P < .001) and proportion of patients resistant to treatment at week 4 (low 45% vs high 71%, P = .03). (C) Validation cohort 2 (n = 68). Twelve-month cumulative incidence of NRM (low 14% vs high 75%, P < .001) and OS (low 78% vs high 14%, P < .001) and proportion of patients resistant to treatment at week 4 (low 29% vs high 68%, P = .004).
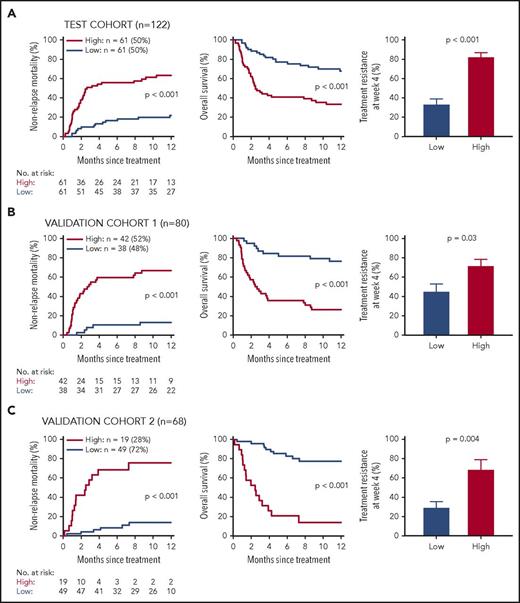
We then evaluated biomarker stratification for patients whose GVHD was sensitive to the first week of systemic treatment. The biomarker algorithm again separated patients into 2 groups, with different outcomes in the test and first validation cohorts, but not in the second validation cohort, where the NRM of the early-response group was only 8% (Figure 3). Again, relapse rates were not different between groups (supplemental Table 3). A similar pattern was seen for prediction of resistance to treatment at week 4. Thus, the biomarker algorithm did not reliably segregate patients into distinct risk groups when the NRM of the group was very low.
Long-term outcomes by biomarker probabilities in early treatment sensitive patients. Early treatment–sensitive patients were subdivided based on biomarker probabilities into low and high groups. (A) Test cohort of patients (n = 114). Twelve-month cumulative incidence of NRM (low 11% vs high 41%, P < .001) and OS (low 70% vs high 47%, P = .004) and proportion of patients resistant to treatment at week 4 (low 18% vs high 38%, P = .06). (B) Validation cohort 1 (n = 62). Twelve-month cumulative incidence of NRM (low 6% vs high 33%, P = .005) and OS (low 79% vs high 53%, P = .03) and proportion of patients resistant to treatment at week 4 (low 30% vs high 67%, P = .03). (C) Validation cohort 2 (n = 61). Twelve-month cumulative incidence of NRM (low 6% vs high 20%, P = .46) and OS (low 88% vs high 80%, P = .80) and proportion of patients resistant to treatment at week 4 (low 8% vs high 28%, P = .18).
Long-term outcomes by biomarker probabilities in early treatment sensitive patients. Early treatment–sensitive patients were subdivided based on biomarker probabilities into low and high groups. (A) Test cohort of patients (n = 114). Twelve-month cumulative incidence of NRM (low 11% vs high 41%, P < .001) and OS (low 70% vs high 47%, P = .004) and proportion of patients resistant to treatment at week 4 (low 18% vs high 38%, P = .06). (B) Validation cohort 1 (n = 62). Twelve-month cumulative incidence of NRM (low 6% vs high 33%, P = .005) and OS (low 79% vs high 53%, P = .03) and proportion of patients resistant to treatment at week 4 (low 30% vs high 67%, P = .03). (C) Validation cohort 2 (n = 61). Twelve-month cumulative incidence of NRM (low 6% vs high 20%, P = .46) and OS (low 88% vs high 80%, P = .80) and proportion of patients resistant to treatment at week 4 (low 8% vs high 28%, P = .18).
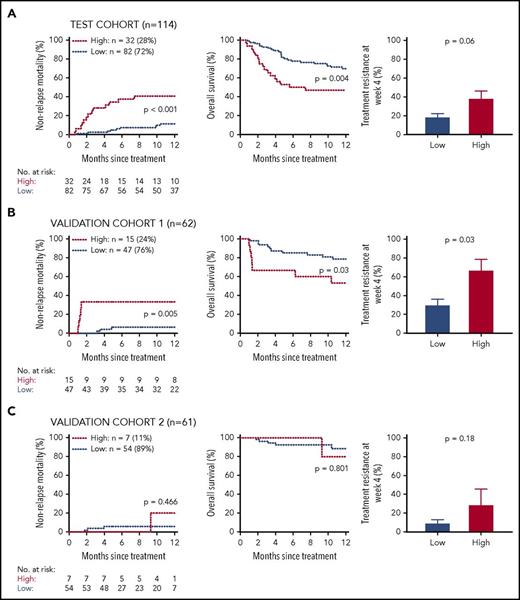
Biomarker probability scores predict NRM better than initial response to treatment or Minnesota clinical severity
The Minnesota clinical staging system has been shown to predict patient outcomes at the onset of GVHD symptoms, but its validity at later time points during treatment is unknown.10 We found that Minnesota risk after 1 week of treatment was highly significant in predicting resistance to treatment at week 4 and NRM at 1 year (supplemental Table 5). Univariate analyses of important pretransplant and GVHD clinical variables showed that only biomarker probability, early response to treatment, and Minnesota risk consistently significantly predicted response to treatment at 4 weeks and 1-year NRM. When these 3 variables were included in multivariate analysis of long-term outcomes in the combined validation cohorts, the biomarker and Minnesota risk ratios remained highly significant (Figure 4A). We then directly compared the ability of each variable to predict NRM by creating receiver operating characteristic curves (Figure 4B). The AUC for the biomarker probabilities was 0.82, significantly higher than 0.68 for early clinical response (P = .004) and 0.72 for Minnesota clinical risk (P = .005). The sensitivity, specificity, positive predictive value, and negative predictive values for 1-year NRM at the threshold used were 74%, 83%, 58%, and 91%, respectively, for the combined validation cohorts. These values are shown in Table 2 for each cohort and for the combined validation cohorts stratified by GVHD severity and initial treatment response. A separate algorithm that included the concentrations of ST2 and REG3α, early treatment response, and Minnesota risk to predict 1-year NRM produced an AUC of 0.84, which was slightly better than the 0.82 for the biomarkers-only algorithm (P = .024); however, the individual clinical characteristics were not statistically significant elements of the algorithm (supplemental Table 6).
Prediction of long-term outcomes by early clinical response and biomarker probability status. (A) Forest plots. Left panel: Effect of early treatment resistance, Minnesota high-risk and high biomarker probability status on odds of resistance to treatment at week 4. Right panel: Effect of early treatment resistance, Minnesota high risk and high biomarker probability status on hazard of NRM at 1 year. Data are ratios and 95% confidence intervals. (B) Receiver operating characteristic curves to predict NRM. Curves are shown for early treatment response, biomarker probabilities, and Minnesota risk. The diamond (♦) indicates the threshold that defines low- versus high-risk groups. AUC for early treatment response = 0.68 (P = .004 compared with biomarker probability), for Minnesota risk = 0.72 (P = .005 compared with biomarker probability), and for biomarker probability = 0.82.
Prediction of long-term outcomes by early clinical response and biomarker probability status. (A) Forest plots. Left panel: Effect of early treatment resistance, Minnesota high-risk and high biomarker probability status on odds of resistance to treatment at week 4. Right panel: Effect of early treatment resistance, Minnesota high risk and high biomarker probability status on hazard of NRM at 1 year. Data are ratios and 95% confidence intervals. (B) Receiver operating characteristic curves to predict NRM. Curves are shown for early treatment response, biomarker probabilities, and Minnesota risk. The diamond (♦) indicates the threshold that defines low- versus high-risk groups. AUC for early treatment response = 0.68 (P = .004 compared with biomarker probability), for Minnesota risk = 0.72 (P = .005 compared with biomarker probability), and for biomarker probability = 0.82.
Sensitivity, specificity, positive-predictive value, and negative-predictive value analyses for 1-year NRM
| . | Sensitivity . | Specificity . | PPV . | NPV . | |
|---|---|---|---|---|---|
| Test cohort | 0.70 | 0.74 | 0.55 | 0.85 | |
| Validation cohort 1 | 0.80 | 0.76 | 0.58 | 0.91 | |
| Validation cohort 2 | 0.63 | 0.93 | 0.58 | 0.91 | |
| Minnesota risk | Early treatment response | ||||
| Standard | Response | 0.50 | 0.86 | 0.29 | 0.94 |
| Standard | Nonresponse | 0.55 | 0.84 | 0.46 | 0.88 |
| High* | Response | NA | NA | NA | NA |
| High | Nonresponse | 0.94 | 0.54 | 0.84 | 0.78 |
| . | Sensitivity . | Specificity . | PPV . | NPV . | |
|---|---|---|---|---|---|
| Test cohort | 0.70 | 0.74 | 0.55 | 0.85 | |
| Validation cohort 1 | 0.80 | 0.76 | 0.58 | 0.91 | |
| Validation cohort 2 | 0.63 | 0.93 | 0.58 | 0.91 | |
| Minnesota risk | Early treatment response | ||||
| Standard | Response | 0.50 | 0.86 | 0.29 | 0.94 |
| Standard | Nonresponse | 0.55 | 0.84 | 0.46 | 0.88 |
| High* | Response | NA | NA | NA | NA |
| High | Nonresponse | 0.94 | 0.54 | 0.84 | 0.78 |
NPV, negative-predictive value; PPV, positive-predictive value.
Too few patients with Minnesota high risk and early treatment response to calculate sensitivity, specificity, positive-predictive value, and negative-predictive value
ST2 and REG3α reflect damage to lower gastrointestinal (GI) mucosa, particularly in the crypts,12,19 and patients with high probabilities eventually experience sixfold more GI GVHD (supplemental Table 7). It should be noted that approximately one third of patients in the study were treated with systemic steroids for grade 1 GVHD (limited skin disease). If one excludes these patients from the analysis (some centers do not routinely use systemic treatment for isolated skin GVHD), the biomarker probabilities continue to divide patients into 2 groups, with significantly different outcomes based on whether patients were resistant to early systemic treatment (supplemental Figure 3). Patients with lower-GI symptoms (≥500 mL of diarrhea) demonstrated a significantly higher 1-year NRM than those with no diarrhea (55% vs 17%, P < .001); however, biomarker probabilities continue to separate both of these populations into 2 groups, with highly significant differences in NRM (supplemental Figure 4).
Discussion
Little progress has been made during the last several decades in validating new treatments for GVHD, for several reasons. The immune systems of all bone marrow transplantation patients have been largely eradicated by the pretransplant conditioning regimens to prevent rejection of the stem cell graft, and half of GVHD develops within the first month of transplant when immunologic reconstitution from the new graft is in its earliest phases.20,21 All strategies to treat acute GVHD suppress multiple elements of the immune system, further diminishing the immunologic competence of the patient. Even successful treatment requires at least a month of additional immunosuppression, increasing vulnerability to potentially fatal opportunistic infections. Thus, treatment of GVHD leads to severe infections that are directly related to the cumulative steroid dose.22,23 Additionally, acute GVHD symptom severity can fluctuate widely on a day-to-day basis, introducing significant uncertainty into assessments of response to treatment.9 GVHD can progress rapidly if not adequately treated, and clinicians often react quickly to worsening symptom severity, even though these might resolve without further intervention. Thus, accurate prediction of durable responses and long-term outcomes is key to escalation and de-escalation of immunosuppressive therapy.
Previous studies have found that early clinical response to GVHD treatment correlates poorly with later clinical response and long-term survival.6,24 In this study, we found that, although early clinical responses continued to evolve, overall response at 1 week continued to have a significant predictive value for long-term outcomes in multivariate analysis (Figure 4). Measurement of serum concentrations of 2 MAGIC biomarkers (ST2 and REG3α) at the same time as the clinical response segregated patients with steroid-resistant GVHD into 2 groups with strikingly different outcomes in all 3 patient cohorts. Patients with a low probability score who have not yet responded to treatment may be slow responders and may not require escalation of immunosuppression, despite the appearance of steroid resistance. Given the serious infectious risks of further immunosuppression, clinicians might adopt a stance of watchful waiting for such patients, an approach that could be addressed in a carefully controlled clinical trial.
We hypothesize that the accuracy of biomarker probabilities reflect the ability of serum concentrations of ST2 and REG3α to measure immunologically mediated changes in tissue more accurately than the severity of the clinical disease or resistance to systemic steroids after 1 week of treatment. The superior predictive accuracy of biomarkers, when added to the presence of clinical symptoms, may be attributed to the number of processes that can simultaneously contribute to clinical GVHD symptoms. For example, diarrhea worsened by a concomitant viral gastroenteritis may be treated as GVHD with systemic steroids that, in fact, may prolong or intensify the viral disease; however, infection does not increase the serum concentration of REG3α and, thus, would not raise the biomarker probability.12 In pediatric patients, increased levels of ST2 correlate with transplant-associated thrombotic microangiopathy, as well as 6-month NRM.25 Transplant-associated thrombotic microangiopathy and damage to the endothelium have been associated with acute GVHD,26,27 but whether such an association also exists in this study cannot be determined due to lack of relevant data.
Previous studies have found prognostic value for combinations of different biomarkers after 2 weeks of systemic steroid treatment, but none have determined the prognostic utility of biomarkers obtained earlier than 14 days into treatment.28,29 In 1 single-center study of 165 patients, the clinical status after 2 weeks of systemic steroid treatment of GVHD was a slightly worse predictor for 1-year NRM than 2 biomarkers (TIM3 and TNFR1) measured at the same time (AUC of 0.81 and 0.85, respectively). It is not surprising that the clinical status after 2 weeks of therapy better reflects long-term outcomes than after 1 week, but some physicians might feel uncomfortable with such a delay, particularly if the patient has not responded to therapy. Thus, an important strength of the current study is the time of analysis at 1 week after therapy, when information is likely to be actionable. A second strength is the fact that the patients contributing data and samples from multiple centers were treated without prescriptive directives, including the second multicenter validation cohort that represents current practice and, therefore, reflects the heterogeneity of “real-life” GVHD treatment practices. A third strength of this study is that, although biomarkers were measured only at a single time point, the same algorithm that generated the probability score following treatment can predict outcomes when used prior to (and at) the onset of GVHD symptoms.8 The use of the same algorithm should enable the comparisons of probabilities generated serially at multiple time points following HCT, facilitating the incorporation of biomarker measurements into clinical practice. One limitation of this study is that the GVHD prophylaxis regimens of posttransplant cyclophosphamide, T-cell depletion, and tacrolimus/sirolimus were used in very few of the patients (Table 1); thus, these results should be applied with caution in these patients populations. It is also important to note that this study has not demonstrated that therapeutic decisions based on biomarker probabilities can change the outcome for patients with GVHD. But such probabilities should prove to be valuable clinical research tools because even relatively large clinical trials for acute GVHD generally do not enroll more than a few hundred patients.24,30 As a result, experimental therapies need to demonstrate a large benefit to prove beneficial, an outcome that has proved elusive over the past 40 years. The inclusion of patients who are likely to respond to standard therapy in a placebo-controlled trial reduces the likelihood of detecting a difference between arms; stratification of treatments by biomarker probability will avoid such a pitfall. Thus, the ability of the biomarker probability to risk stratify for patients who are not responding to systemic therapy should prove useful in clinical trial design and, ultimately, may help to tailor GVHD treatment to the risks and benefits for individual patients.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the patients, their families, and the research staff for their participation.
This work was supported by grants from the National Institutes of Health, National Cancer Institute (R21CA173459, P01CA03942, and P30CA196521), an American Cancer Society Clinical Research Professorship (J.L.M.F.), and a Doris Duke Charitable Foundation Clinical Research Mentorship (M.J.H.).
Authorship
Contribution: H.M.-M., A.S.R., U.Ö., J.L.M.F., and J.E.L. designed the study, analyzed data, and wrote the paper; H.M.-M., M.J.H., M.A., S.K., G.M., and I.T. performed laboratory analyses; U.Ö., M.S.C., J.L.M.F., and J.E.L. created the figures; H.M.-M., A.S.R., A.P., F.A., E.H., Y.A.E., W.J.H., M.W., M.Q., E.O.H., K.W., R.O., R.Y., J.S., A.E., G.A.Y., D.W., A.C.H., M.P., and R.R. collected data; and all authors interpreted the data and contributed to the writing of the paper.
Conflict-of-interest disclosure: J.E.L., J.L.M.F., and U.Ö. are joint inventors on a GVHD biomarker patent. The remaining authors declare no competing financial interests.
Correspondence: John E. Levine, The Tisch Cancer Institute, Mount Sinai School of Medicine, 1 Gustave Levy Place, Box 1410, New York, NY 10029; e-mail: john.levine@mssm.edu.
References
Author notes
H.M.-M. and A.S.R. contributed equally to this work.
U.Ö., J.L.M.F., and J.E.L. contributed equally to this work.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal