Issue Archive
Table of Contents
BLOOD COMMENTARIES
HOW I TREAT
How I treat pediatric pulmonary embolism
Pulmonary embolism (PE) is a potentially life-threatening and life-altering diagnosis for children. Zia et al use 2 case studies to illustrate current acute care and postacute management of children with PE. They highlight recent and ongoing clinical studies that should guide future improvements in clinical approaches to this uncommon but potentially devastating illness.
CLINICAL TRIALS AND OBSERVATIONS
Marstacimab prophylaxis in hemophilia A/B without inhibitors: results from the phase 3 BASIS trial
Clinical Trials & Observations
New therapies for hemophilia A and B include a class of monoclonal antibodies that target tissue factor pathway inhibitor (TFPI), thereby increasing thrombin production and reducing bleeding risk when factor VIII or IX levels are very low. Matino and colleagues report the results of a pivotal open-label multicenter crossover phase 3 study comparing a new anti-TFPI agent, marstacimab, with standard factor prophylaxis and on-demand treatment in people with hemophilia A or B. Weekly subcutaneous marstacimab reduced the annualized bleeding rate and target joint bleeding, and no instances of thromboembolism were observed, leading to approval of this agent by the US Food and Drug Administration.
Matched donor allogeneic CAR-T for adult B-ALL: toxicity, efficacy, repeat dosing, and the importance of lymphodepletion
Clinical Trials & Observations
Allogeneic hematopoietic stem cell transplantation is the most successful therapy for adults with relapsed acute lymphoblastic leukemia, but relapse remains a problem. Roddie et al present a phase 1 study of locally produced, donor-derived anti-CD19 chimeric antigen receptor (CAR) T-cell infusion, termed CAR-DLI, in patients with relapse after allograft. Data on 14 patients indicate that lymphodepletion is necessary for durable efficacy and that escalating repeat doses of CAR-DLI did not provide additional benefit. While preliminary, these findings point to encouraging feasibility and efficacy of this type of regimen, which should be further tested in larger, randomized trials.
LYMPHOID NEOPLASIA
Remission conversion drives outcomes after CAR T-cell therapy for multiple myeloma: a registry analysis from the DRST
Clinical Trials & Observations
Merz et al report a large national registry–based analysis of standard-of-care chimeric antigen receptor (CAR) T-cell therapy with idecabtagene vicleucel (ida-cel) or ciltacabtagene autoleucel (cilta-cel) for patients with heavily pretreated multiple myeloma following the introduction of these treatments into Germany’s universal health care system. Using multivariable analyses and propensity matching, they identified depth of disease control before and after infusion as key determinants of outcomes and showed cilta-cel to be more efficacious but significantly more toxic than ide-cel in real-world practice. These data reinforce the applicability of clinical trial data to routine care.
A new prognostic index (CLIPI) for advanced cutaneous lymphoma enables precise patient risk stratification
Clinical Trials & Observations
Brief Report
Therapeutic decision-making in primary cutaneous T-cell lymphomas is largely dependent on the extent of cutaneous and extracutaneous involvement and is guided by an established staging system. Prognostication, however, has been problematic, especially for advanced disease. Scarisbrick and consortium colleagues describe development of the cutaneous lymphoma international prognostic index (CLIPI) from an international multicenter prospective study of advanced-stage mycosis fungoides and Sézary syndrome. The CLIPI comprises 4 prognostic factors; effectively stratifies patients into high-, intermediate-, and low-risk groups with 5-year overall survival rates of 18.3%, 44.7%, and 63.3%, respectively; and represents a major opportunity for both personalizing and improving care.
MYELOID NEOPLASIA
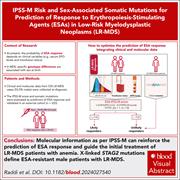
IPSS-M risk and specific sex-associated somatic mutations predict response to ESA therapy in LR-MDS: building a new score
Clinical Trials & Observations
In patients with low-risk myelodysplastic syndrome (LR-MDS), a key goal is to improve anemia and alleviate its impact on quality of life. However, not all patients respond to erythropoiesis-stimulating agents (ESAs). Raddi et al introduce and provide validation for a new molecular predictive scoring system, ESA-PSS-M, which improves prediction of response to first-line ESAs. While no single gene mutation explains most resistance to ESAs, mutations in the X-linked gene STAG2 in men but not women are associated with an eightfold lower chance of response in LR-MDS. ESA-PSS-M should be readily adoptable in practice.
PHAGOCYTES, GRANULOCYTES, AND MYELOPOIESIS
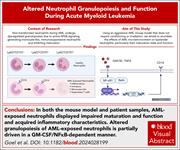
The acute myeloid leukemia microenvironment impairs neutrophil maturation and function through NF-κB signaling
RED CELLS, IRON, AND ERYTHROPOIESIS
The endothelial mTORC2-Foxo1 axis serves as an iron-responsive sensor governing systemic iron homeostasis
Liver sinusoidal endothelial cells (LSECs) regulate systemic iron metabolism by secreting bone morphogenetic proteins (BMPs), key modulators of systemic iron homeostasis. Zhao and colleagues uncovered a critical role of mTORC2 and Foxo1 as iron sensors in LSECs. They demonstrate that iron triggers lysosomal degradation of the Rictor subunit of the mTORC2 complex, which allows Foxo1 translocation to the nucleus for transcriptional activation of BMP2 and BMP6, the major inducers of the iron-regulatory hormone hepcidin, which prevents systemic iron overload.
BLOOD WORK
-
Cover Image
Cover Image
![issue cover]()
The colocalization of rapamycin-insensitive companion of mTOR (Rictor) (green) and Lamp2 (red) in liver sinusoidal endothelial cells treated with holo-transferrin demonstrates iron-induced lysosomal degradation of Rictor, a mechanistic target of rapamycin complex 2-specific component, is a key iron-sensing mechanism. Nuclei are shown in blue. See the review by Zhao et al on page 1722.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals





Rebalancing the hemophilia teeter-totter
Clinical Trials & Observations