Issue Archive
Table of Contents
EDITORIAL
Introduction to a How I Treat series on geriatric hematology
Edited by Associate Editor Thomas L. Ortel, this How I Treat series focuses on geriatric hematology. Using illustrative cases, the authors present their approach to geriatric patients with von Willebrand disorders, anemia, thrombocytopenia, and multiple myeloma.
BLOOD COMMENTARIES
HOW I TREAT SERIES
How I treat von Willebrand disorders in older adults
Edited by Associate Editor Thomas L. Ortel, this How I Treat series focuses on geriatric hematology. Using illustrative cases, the authors present their approach to geriatric patients with von Willebrand disorders, anemia, thrombocytopenia, and multiple myeloma.
How I treat anemia in older adults
Edited by Associate Editor Thomas L. Ortel, this How I Treat series focuses on geriatric hematology. Using illustrative cases, the authors present their approach to geriatric patients with von Willebrand disorders, anemia, thrombocytopenia, and multiple myeloma.
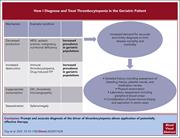
How I diagnose and treat thrombocytopenia in geriatric patients
Edited by Associate Editor Thomas L. Ortel, this How I Treat series focuses on geriatric hematology. Using illustrative cases, the authors present their approach to geriatric patients with von Willebrand disorders, anemia, thrombocytopenia, and multiple myeloma.
How I treat multiple myeloma in geriatric patients
Edited by Associate Editor Thomas L. Ortel, this How I Treat series focuses on geriatric hematology. Using illustrative cases, the authors present their approach to geriatric patients with von Willebrand disorders, anemia, thrombocytopenia, and multiple myeloma.
CLINICAL TRIALS AND OBSERVATIONS
Malignancy-associated hemophagocytic lymphohistiocytosis in Sweden: incidence, clinical characteristics, and survival
Clinical Trials & Observations
Malignancy-associated hemophagocytic lymphohistiocytosis (mal-HLH) is a hyperinflammatory syndrome that carries a dire prognosis. Löfstedt et al describe the incidence and natural history of mal-HLH based on the Swedish Patient Registry covering 1997-2018. With increasing recognition of the syndrome and improved diagnosis, the incidence rose from 0.026 per 100 000 in 1997-2007 to 0.34 in 2008-2018. However, while treatment has improved early mortality, 2-year survival remains dismal at 25%.
HEMATOPOIESIS AND STEM CELLS
Regulation of lymphoid-myeloid lineage bias through regnase-1/3-mediated control of Nfkbiz
Uehata and colleagues report that the mRNA decay factors regnase-1 and -3 (Reg1 and Reg3) play a critical role in lineage bias of hematopoietic stem and progenitor cells (HSPCs), restricting myeloid differentiation in favor of lymphoid commitment. Reg1 and Reg3 control the epigenetics of myeloid gene loci in early stage HSPCs by regulating degradation of the mRNA encoding the epigenetic modifier Nfkbiz.
LYMPHOID NEOPLASIA
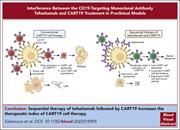
CD19 occupancy with tafasitamab increases therapeutic index of CART19 cell therapy and diminishes severity of CRS
CD19-targeted chimeric antigen receptor T-cell (CART19) therapy requires tumor cell CD19 expression, and it is unclear whether prior anti-CD19 antibody therapy impairs response to CART19 therapy. Sakemura et al studied the impact of tafasitamab exposure on subsequent CART19 therapy in preclinical models. Concomitant treatment leads to competition for binding and impairs response to CART19; however, pretreatment with CD19 antibody does not impair CART19 responses. This pretreatment reduced cytokine release syndrome and showed superior antitumor effect and overall survival in mice, suggesting clinical development of the combination may lead to better outcomes.
PLATELETS AND THROMBOPOIESIS
The bone marrow is the primary site of thrombopoiesis
Brief Report
Recent reports of megakaryocytes within the spleen and lung have generated controversy as to the relative contribution of extramedullary megakaryopoiesis in circulating platelet mass. Asquith et al used a series of elegant studies to establish that there are far more megakaryocytes in the bone marrow than in extramedullary sites and that they have a greater proplatelet-formation capacity, confirming the bone marrow as the major contributor to steady state platelet production.
TRANSPLANTATION
TCRαβ/CD19 cell–depleted HLA-haploidentical transplantation to treat pediatric acute leukemia: updated final analysis
CME
Clinical Trials & Observations
Haploidentical hematopoietic stem cell transplantation (HSCT) has come of age through improved pre- or posttransplant T-cell manipulation by graft T-cell depletion or posttransplant cyclophosphamide, respectively. In this month’s CME article, Merli and coauthors report long-term outcomes of 213 children receiving haploidentical HSCT with ex vivo TCRαβ/CD19-cell depletion with median follow-up of 4 years. Results were excellent, with projected 10-year overall survival of 75.4%. Nonrelapse mortality and graft-versus-host disease rates were low. Relapse occurred in 22.7% of patients, with pre-HSCT disease status and minimal residual disease predicting relapse.
BLOOD WORK
CONTINUING MEDICAL EDUCATION (CME) QUESTIONS
-
Cover Image
Cover Image
![issue cover]()
A structured illumination microscopy fluorescence image of an ex vivo differentiated bone marrow megakaryocyte making platelets via elongated proplatelet intermediates. The DNA content of the megakaryocytes is shown in blue, microtubules of megakaryocytes and proplatelets in cyan, and the canonical megakaryocyte marker CD41 in magenta, highlighting how the bone marrow is the primary site of thrombopoiesis. See the article by Asquith et al on page 272.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Back MatterBack Matter
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals










Just in time: mal-HLH in Sweden, 1997 to 2018
Clinical Trials & Observations