Issue Archive
Table of Contents
BLOOD COMMENTARIES
HOW I TREAT
How I treat refractory and relapsed acute myeloid leukemia
Using a series of 3 illustrative cases, Thol and colleagues discuss their approach to relapsed/refractory acute myeloid leukemia. Although allogeneic hematopoietic cell transplantation is the only potential cure, many patients are not candidates for this intervention. The authors discuss the options for targeted therapies, treatment at the first detection of measurable residual disease, and novel agents that may improve the dismal prognosis of this difficult disease.
CLINICAL TRIALS AND OBSERVATIONS
A phase 2 trial of CD24Fc for prevention of graft-versus-host disease
Clinical Trials & Observations
Recipients of matched unrelated donor allogeneic stem cell transplantation often develop acute graft-versus-host-disease (GVHD) despite standard calcineurin inhibitor/methotrexate prophylaxis. Hypothesizing that this is in part related to inflammatory sequelae of intensive conditioning due to damage-associated molecular patterns (DAMPs), Magenau et al report on a phase 2a trial of adding CD24Fc, a CD24 fusion protein that targets DAMP-mediated inflammation. CD24Fc is well tolerated and results in acute GVHD-free survival of 96%, encouraging a larger trial of this novel therapeutic agent.
HEMATOPOIESIS AND STEM CELLS
Chronic active Epstein-Barr virus disease originates from infected hematopoietic stem cells
Clinical Trials & Observations
Epstein-Barr virus (EBV) is typically viewed as an organism that infects B lymphocytes, causing a self-limited disease that is associated with a residual reservoir of infected B cells held in check by T cells. Chronic active EBV (CAEBV) is a syndrome of persistent EBV infection that is nearly always fatal unless treated with allogeneic hematopoietic stem cell transplantation (HSCT) and is known to manifest with infection outside of the B-cell population. Wang and colleagues, using PrimeFlow and single-cell RNA sequencing, report that CAEBV is associated with EBV infections of hematopoietic stem cells, giving rise to multilineage infection. Successful HSCT eradicates EBV-infected stem cells.
LYMPHOID NEOPLASIA
Integrated epigenetic and transcriptional single-cell analysis of t(11;14) multiple myeloma and its BCL2 dependency
Multiple myeloma (MM) associated with translocation t(11;14) accounts for about 20% of MM cases, is associated with BCL2 dependency in about two-thirds of cases, and is especially sensitive to venetoclax. Leblay and colleagues used single-cell analysis to characterize the transcriptional landscape of t(11;14) MM. The authors report that this subgroup of MM is enriched for a “B-cell–like” epigenetic signature, suggesting a strong link to B-cell rather than plasma-cell biology. Acquired venetoclax resistance correlates with transition to a more plasma cell–like profile.
Ibrutinib-based therapy reinvigorates CD8+ T cells compared to chemoimmunotherapy: immune monitoring from the E1912 trial
Clinical Trials & Observations
Brief Report
The E1912 trial comparing ibrutinib/rituximab (IR) to fludarabine/cyclophosphamide/rituximab (FCR) confirmed the superiority of IR for the initial treatment of chronic lymphocytic leukemia (CLL). Papazoglou et al report on a longitudinal secondary immunophenotypic analysis of these patients, reporting that IR enhances anti-CLL T-cell killing through reversal of T-cell exhaustion, whereas T-cell responses are not improved with FCR, correlating with the observation of no infections and improved progression-free survival in the IR arm.
PLATELETS AND THROMBOPOIESIS
PF4 activates the c-Mpl–Jak2 pathway in platelets
Brief Report
Platelet factor 4 (PF4) is released from platelet alpha granules upon activation, and anti-PF4 antibodies are central to the pathophysiology of platelet activation in vaccine-induced immune thrombocytopenia and thrombosis (VITT). Buka and colleagues demonstrate that PF4 binds and activates the thrombopoietin receptor, triggering activation of JAK-STAT signaling and platelet aggregation. Inhibition of JAK-STAT signaling with ruxolitinib inhibits platelet aggregation in response to PF4, to VITT serum, and to PF4 and IgG isolated from VITT patient plasma. This suggests a potential role for JAK2 inhibition in the treatment of the range of PF4-mediated platelet aggregation syndromes.
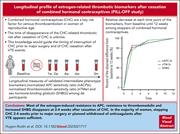
THROMBOSIS AND HEMOSTASIS
Longitudinal profile of estrogen-related thrombotic biomarkers after cessation of combined hormonal contraceptives
Clinical Trials & Observations
The duration of prothrombotic risk following cessation of combined hormonal contraceptives (CHC) is unknown. Hugon-Rodin and colleagues report on a prospective cohort study assessing the time to normalization of estrogen-related biomarkers over 12 weeks following discontinuation of CHC in 28 women without prior history of thrombosis or current anticoagulation. These biomarkers rapidly decreased and were 80-90% corrected at 2-4 weeks, providing possible guidance that thrombotic risk resolves over 2-4 weeks.
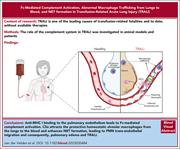
TRANSFUSION MEDICINE
Complement activation drives antibody-mediated transfusion-related acute lung injury via macrophage trafficking and formation of NETs
Transfusion-related acute lung injury (TRALI) is one of the leading causes of transfusion-related fatalities. van der Velden et al investigated the role of complement activation in TRALI. The authors show that Fc-mediated complement activation plays a critical role in TRALI, which is associated with macrophage trafficking from the lungs to the blood and with neutrophil extracellular trap formation. This suggests that targeting complement activation may be a potential therapy for TRALI.
BLOOD WORK
ERRATUM
-
Cover Image
Cover Image
![issue cover]()
Strong immune synapses between helper CD4+ T cells and chronic lymphocytic leukemia (CLL) cells at baseline correlate with unfavorable clinical responses during ibrutinib-rituximab therapy. CD4+ T cells are shown as green, F-actin is red, and CLL cells are blue. Advantageously, ibrutinib therapy promotes a switch to CD8+ T-cell synapses. See the article by Papazoglou et al on page 57.
- PDF Icon Front MatterFront Matter
- PDF Icon Table of ContentsTable of Contents
- PDF Icon Back MatterBack Matter
- PDF Icon Editorial BoardEditorial Board
Advertisement intended for health care professionals
Email alerts
Advertisement intended for health care professionals







CD24Fc to DAMPen GVHD
Clinical Trials & Observations