Key Points
Mcl-1 inhibition by pan-active Bcl-2 inhibitor (–)BI97D6 kills AML cells via induction of mitochondrial apoptosis.
Mcl-1 inhibition by (–)BI97D6 overcomes intrinsic and extrinsic drug resistance to ABT-737.
Abstract
Overexpression of antiapoptotic Bcl-2 proteins such as Bcl-2, Bcl-xL, and Mcl-1 is widely associated with tumor initiation, progression, and chemoresistance. Furthermore, it has been demonstrated that Mcl-1 upregulation renders several types of cancers resistant to the Bcl-2/Bcl-xL inhibitors ABT-737 and ABT-263. The emerging importance of Mcl-1 in pathogenesis and drug resistance makes it a high-priority therapeutic target. In this study, we showed that inhibition of Mcl-1 with a novel pan–Bcl-2 inhibitor (–)BI97D6 potently induced apoptosis in acute myeloid leukemia (AML) cells. (–)BI97D6 induced hallmarks of mitochondrial apoptosis, disrupted Mcl-1/Bim and Bcl-2/Bax interactions, and stimulated cell death via the Bak/Bax-dependent mitochondrial apoptosis pathway, suggesting on-target mechanisms. As a single agent, this pan–Bcl-2 inhibitor effectively overcame AML cell apoptosis resistance mediated by Mcl-1 or by interactions with bone marrow mesenchymal stromal cells. (–)BI97D6 was also potent in killing refractory primary AML cells. Importantly, (–)BI97D6 killed AML leukemia stem/progenitor cells while largely sparing normal hematopoietic stem/progenitor cells. These findings demonstrate that pan–Bcl-2 inhibition by an Mcl-1–targeting inhibitor not only overcomes intrinsic drug resistance ensuing from functional redundancy of Bcl-2 proteins, but also abrogates extrinsic resistance caused by the protective tumor microenvironment.
Introduction
Cancer cells are subject to various intrinsic and extrinsic stresses, including oncogene activation, mitotic checkpoint violation, hypoxia, and low nutrient availability.1-3 Various innate tumor-suppressive mechanisms have evolved to kill stressed malignant cells, predominantly by induction of apoptosis.1,2,4 However, evasion of apoptosis is one of the hallmarks of cancer, driven in part by upregulation of antiapoptotic members of the Bcl-2 protein family.3,5-7 Overexpression of the antiapoptotic Bcl-2 proteins, especially Bcl-2, Bcl-xL, Mcl-1, and Bfl-1, has been widely implicated in resistance to conventional chemotherapy and novel targeted therapeutics. Therefore, the development of selective inhibitors of Bcl-2 family antiapoptotic proteins has become a pressing pharmacologic need for treatment of refractory malignancies.
Small molecules mimicking the BH3 domains of Bcl-2 family proapoptotic proteins have been developed to directly inhibit Bcl-2 antiapoptotic proteins. To date, the most successful BH3 mimetics are the Abbott Laboratories (ABT) compounds, including the Bcl-2/Bcl-xL inhibitors ABT-7378 and ABT-263 (navitoclax),9 and the Bcl-2–selective ABT-199 (GDC-0199).10 Early clinical trials with navitoclax have demonstrated single-agent efficacy in Bcl-2/Bcl-xL–dependent cancers.11,12 However, the ABT compounds bind poorly to Mcl-1; thus, tumor cells expressing high Mcl-1 display resistance to these agents.11,13-16
High-resolution analyses of somatic copy number alterations identified MCL1 as one of the most amplified genes in cancer.17 Mcl-1 overexpression has been implicated in the pathogenesis and drug resistance of various cancers. For example, bench-to-bedside studies identified Mcl-1 as a critical factor in resistance to ABT-737.11,13-16,18 Furthermore, ABT-737 was recently found to induce Mcl-1 expression, likely via mechanisms involving Erk activation18 or upregulation of Mcl-1 deubiquinase USP9X.19 The induced expression/stabilization of Mcl-1 protein further enhanced tumor resistance to ABT compounds.
The emerging pathogenic role of Mcl-1 makes it a high-priority therapeutic target. Given that the Bcl-2 proteins are functionally redundant, a promising strategy would be to develop BH3 mimetics that inhibit Mcl-1 and other antiapoptotic Bcl-2 proteins. Guided by nuclear magnetic resonance binding assays, fluorescence polarization, and computational docking studies, we previously synthesized a series of apogossypolone (ApoG2) derivatives.20 Among them, the optically pure compound (–)BI97D6 potently binds Mcl-1, Bcl-2, Bcl-xL, and Bfl-1, with IC50 values of 0.025, 0.031, 0.076, and 0.122 μM, respectively.21 The high affinity of (–)BI97D6 for the 4 predominant antiapoptotic members, especially Mcl-1, makes it a promising BH3 mimetic.
Acute myeloid leukemia (AML) is a hematopoietic neoplasia characterized by the rapid expansion of malignant myeloid cells.22 AML is primarily treated with chemotherapy, but the 5-year survival has only marginally increased over the last few decades. Most AMLs develop chemoresistance during treatment and relapse after initial response. The fact that ∼70% of AML patients die of this disease highlights the urgent need for novel therapies. Recently, Mcl-1 was reported to be essential for AML development, survival, and drug resistance.13,23 In this study, we examined the efficacy and underlying mechanisms of action of (–)BI97D6 in AML cells, especially those with high Mcl-1 expression. We investigated the effectiveness of pan–Bcl-2 inhibition in abrogating AML intrinsic and extrinsic drug resistance and evaluated the potential therapeutic window of targeting Mcl-1 with (–)BI97D6.
Methods
Assessment of cell viability/apoptosis and determination of IC50 values
Cells were treated as indicated and analyzed by fluorescence-activated cell sorting (FACS). For detection of apoptosis, treated cells were pelleted by centrifugation and washed twice with 2 mL Annexin V binding buffer (ABB).24 The cells were then resuspended in 100 μL ABB containing Annexin V–fluorescein isothiocyanate (FITC; Roche Applied Sciences, Indianapolis, IN) and incubated in darkness at room temperature for 15 minutes. Next, the cells were washed once to remove excessive Annexin V–FITC and resuspended in 300 μL ABB. Propidium iodide (PI; Sigma-Aldrich, St Louis, MO) was added immediately before analysis by a Gallios flow cytometer (Beckman Coulter, Indianapolis, IN). To determine cell number, CountBright beads (Life Technologies, Carlsbad, CA) were added to each sample. Data were analyzed using Kaluza (Beckman Coulter) and Flowjo (Tree Star, Ashland, OR). IC50 values were calculated using Calcusyn software (Biosoft, Great Shelford, UK), based on the absolute number of live cells (ie, Annexin V−/PI−).
Immunoblot and immunoprecipitation
We performed immunoblot and immunoprecipitation (IP) as previously described.14 The Odyssey infrared imaging system and companion software v2.0 (LI-COR Biosciences, Lincoln, NE) were used to scan immunoblot membranes and to quantify band intensity according to the manufacturer’s manual. The ratios of band intensity of Mcl-1/α-tubulin, Bcl-2/Bax, Bcl-2/α-tubulin, and Bcl-xL/α-tubulin in treated samples were normalized to their counterparts in untreated cells. The antibodies used in this study are listed in supplemental Methods available on the Blood Web site.
Primary cell isolation, treatment, and viability analysis
Primary samples from AML patients and healthy donors were obtained by informed consent from The University of Texas MD Anderson Cancer Center according to protocols approved by the institute’s Institutional Review Board, in accordance with the Declaration of Helsinki. The patients’ clinical characteristics are presented in Table 1. Mononuclear cells were isolated from bone marrow (BM) or peripheral blood samples by Ficoll (Sigma-Aldrich) density centrifugation and used immediately. The isolated cells were treated with (–)BI97D6 in RPMI-1640 medium containing 10% fetal bovine serum. After 48 hours, cell viability was assessed by flow cytometry following Annexin V and PI staining as already described. Samples with spontaneous apoptosis >30% were excluded from analysis. For stem/progenitor cell studies, the primary cells were also stained with hCD34-allophycocyanin (APC) and hCD38-phycoerythrin (BD Biosciences). Then, live cells were enumerated after gating on bulk, CD34+, or CD34+/CD38− cells.
Coculture assays
BM-derived mesenchymal stromal cells (MSCs) were isolated and cultured as previously described.24 On day 1, BM MSCs were plated in their growth medium at 2.5 × 104 cells per well in 24-well plates. After 24 hours, the medium was removed and replaced with 1.0 × 105 OCI-AML3 cells in their growth medium. After coculture for 24 hours, the medium was removed with care not to disturb the attached cells and replaced with growth medium containing drug as indicated. The cells were cocultured for 72 hours and then stained and analyzed by FACS. Human CD90-APC (BD Biosciences) was used to distinguish BM MSCs (CD90+) from AML cells (CD90−).
In vivo engraftment experiment
The mouse study was conducted in accordance with guidelines approved by the Institutional Animal Care and Use Committees at MD Anderson Cancer Center. Female NOD SCID γ (NSG) mice (6 weeks old; Jackson Laboratory, Bar Harbor, ME) were sublethally irradiated (250 cGy) 1 day before intravenous injection of control or treated patient-derived AML cells (1.0 × 106). Five weeks after injection, 50 μL blood was collected from each mouse by retroorbital bleeding, and following lysis of red blood cells, cells were stained with human CD45-phycoerythrin and murine CD45-APC (BD Biosciences) for FACS analysis. After confirmation of AML engraftment, the mice in each group (n = 5) were monitored for survival.
Statistical analyses
Unless otherwise indicated, the data represent the mean ± standard deviation from ≥3 independent experiments. P ≤ .05 was considered statistically significant. Differences between control and treated cells were determined using the paired Student t test. Statistical analyses were performed using Prism software v6.0 (GraphPad Software, La Jolla, CA).
Results
Pan–Bcl-2 inhibitor (–)BI97D6 promotes cell death via mitochondrial apoptosis
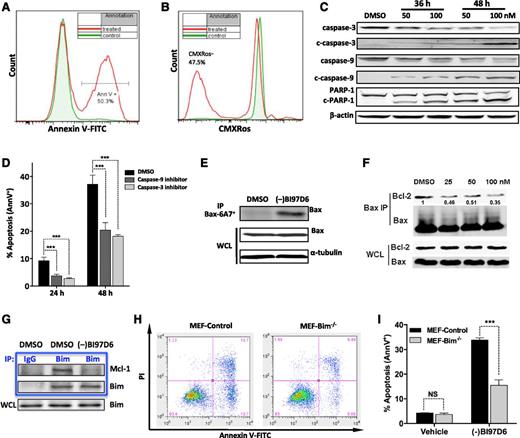
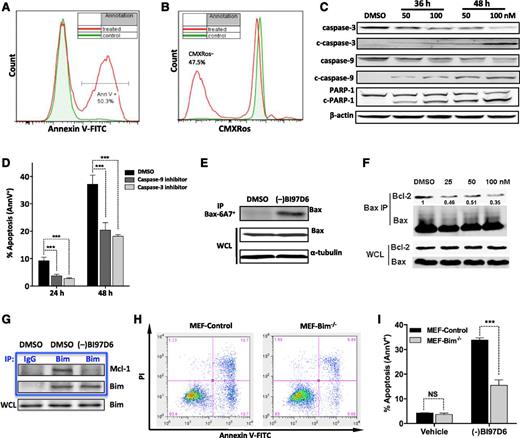
We first studied the cell death mechanisms triggered by (–)BI97D6. The externalization of plasma membrane phosphatidylserine and the loss of mitochondrial membrane potential (∆Ψm) are hallmarks of apoptosis. After incubation of OCI-AML3 cells with 50 nM (–)BI97D6, phosphatidylserine externalization was readily detected by Annexin V staining (Figure 1A). Similarly, the loss of ∆Ψm was observed in about half the cells, as measured by CMXRos assay (Figure 1B) or by JC-1 staining (data not shown). Consistent with these apoptotic hallmarks, the treated OCI-AML3 cells exhibited cleavage of caspase-3, caspase-9, and poly ADP ribose polymerase (PARP)-1 (Figure 1C). Furthermore, preincubation with caspase-9 or -3 inhibitors significantly reduced (–)BI97D6-induced apoptosis of OCI-AML3 cells (Figure 1D).
(–)BI97D6 induces multiple hallmarks of mitochondrial apoptosis. (A-B) Phosphatidylserine externalization as determined by (A) Annexin V (AnnV) staining and (B) loss of mitochondrial membrane potential as measured by CMXRos assay in OCI-AML3 cells after 48-hour treatment with 50 nM (–)BI97D6. (C) Cleavage of caspase-3, caspase-9, and PARP-1 in OCI-AML3 cells after (–)BI97D6 treatment of 36 or 48 hours. (D) Apoptosis induction (AnnV+) by 50 nM (–)BI97D6 in OCI-AML3 cells pretreated with a caspase-3 or -9 inhibitor for 2 hours. ***P < .001. (E) Bax conformational change as measured by immunoprecipitation (IP) with an anti-Bax 6A7 monoclonal antibody. OCI-AML3 cells were treated with 100 nM (–)BI97D6 for 24 hours. WCL, whole cell lysate. (F) Disruption of Bcl-2/Bax association by (–)BI97D6 as shown by Bax/Bcl-2 co-IP. Bax was immunoprecipitated from OCI-AML3 cells following (–)BI97D6 treatment of 24 hours. (G) Disruption of Mcl-1/Bim association by (–)BI97D6. Bim was immunoprecipitated from OCI-AML3 cells treated with 100 nM (–)BI97D6 or vehicle for 24 hours. (H-I) Bim deficiency reduced apoptosis induction by (–)BI97D6. (H) Representative flow cytometry plots of MEF control and Bim−/− cells following treatment with 300 nM (–)BI97D6 for 48 hours. (I) Apoptosis induction as measured by AnnV/PI flow cytometry after 48-hour treatment with 300 nM (–)BI97D6.
(–)BI97D6 induces multiple hallmarks of mitochondrial apoptosis. (A-B) Phosphatidylserine externalization as determined by (A) Annexin V (AnnV) staining and (B) loss of mitochondrial membrane potential as measured by CMXRos assay in OCI-AML3 cells after 48-hour treatment with 50 nM (–)BI97D6. (C) Cleavage of caspase-3, caspase-9, and PARP-1 in OCI-AML3 cells after (–)BI97D6 treatment of 36 or 48 hours. (D) Apoptosis induction (AnnV+) by 50 nM (–)BI97D6 in OCI-AML3 cells pretreated with a caspase-3 or -9 inhibitor for 2 hours. ***P < .001. (E) Bax conformational change as measured by immunoprecipitation (IP) with an anti-Bax 6A7 monoclonal antibody. OCI-AML3 cells were treated with 100 nM (–)BI97D6 for 24 hours. WCL, whole cell lysate. (F) Disruption of Bcl-2/Bax association by (–)BI97D6 as shown by Bax/Bcl-2 co-IP. Bax was immunoprecipitated from OCI-AML3 cells following (–)BI97D6 treatment of 24 hours. (G) Disruption of Mcl-1/Bim association by (–)BI97D6. Bim was immunoprecipitated from OCI-AML3 cells treated with 100 nM (–)BI97D6 or vehicle for 24 hours. (H-I) Bim deficiency reduced apoptosis induction by (–)BI97D6. (H) Representative flow cytometry plots of MEF control and Bim−/− cells following treatment with 300 nM (–)BI97D6 for 48 hours. (I) Apoptosis induction as measured by AnnV/PI flow cytometry after 48-hour treatment with 300 nM (–)BI97D6.
Caspase-9 cleavage and loss of ∆Ψm suggest that (–)BI97D6 might kill cells via the intrinsic mitochondrial apoptosis pathway. However, this compound also induced cleavage of caspase-8 (supplemental Figure 1A available on the Blood Web site), an event classically associated with the extrinsic apoptosis pathway.25 To determine whether caspase-8 is required for (–)BI97D6-induced apoptosis, mutant caspase-8 Jurkat I9.2 cells and parental Jurkat A3 cells expressing functional caspase-8 were examined. The induction of apoptosis was similar in Jurkat I9.2 and A3 cells (supplemental Figure 1B), indicating caspase-8 is not required for (–)BI97D6-induced apoptosis. Notably, ABT-737 also induces caspase-8 cleavage,14 which might be explained by the feedback cleavage of caspase-8 by activated caspase-3.26
During mitochondrial apoptosis, activated Bax undergoes a conformational change resulting in exposure of an N-terminal epitope that can be detected by Bax antibody clone 6A7.27 As shown in Figure 1E, (–)BI97D6 treatment did not change total Bax expression but induced the 6A7+ proapoptosis conformation. Thus, (–)BI97D6 appears to stimulate Bax activation, consistent with its BH3 mimetic properties.
Next, we studied whether (–)BI97D6 disrupts the interactions of Bcl-2 and Mcl-1 with proapoptotic Bcl-2 proteins. As seen in Figure 1F, treatment with (–)BI97D6 did not alter the expression level of Bcl-2 or Bax. Nevertheless, markedly less Bcl-2 coimmunoprecipitated with Bax in treated cells (Figure 1F), implying that (–)BI97D6 treatment disrupted the association between Bcl-2 and Bax. Mcl-1 neutralizes the activity of Bax activator protein Bim by binding and sequestering it.28 Consistent with (–)BI97D6’s high affinity to Mcl-1, much less Mcl-1 protein coimmunoprecipitated with Bim in treated cells (Figure 1G), suggesting that (–)BI97D6 could release Bim from Mcl-1 sequestration. Furthermore, Bim deficiency significantly reduced apoptosis induction in mouse embryonic fibroblast (MEF) cells (Figure 1H-I). Similarly, Bax or Bak single deficiency greatly decreased, but did not block, (–)BI97D6-induced apoptosis (supplemental Figure 2), reflecting the functional redundancy of Bax and Bak.29,30 Importantly, Bax−/−Bak−/− MEF cells were completely resistant to (–)BI97D6 (supplemental Figure 2), further supporting the hypothesis that at the concentrations used here, (–)BI97D6 mediates cytotoxicity via on target mechanisms—namely, via the Bax/Bak-dependent mitochondrial apoptosis pathway. (–)BI97D6 did not significantly modulate the expression of Bcl-2, Bax, Bak, Bad, Bid, and NOXA. Interestingly, a concurrent decrease of Mcl-1 and Bim was observed (supplemental Figure 3). Because (–)BI97D6 disrupts the Mcl-1/Bim association, this observation is consistent with previous reports that Mcl-1 and Bim reciprocally stabilize each other from degradation when in association.31-33 Mcl-1, Bim, and Bcl-xL can be degraded by active caspases in dying cells,34-39 which might also contribute to the observed decrease of these 3 proteins (supplemental Figure 3).
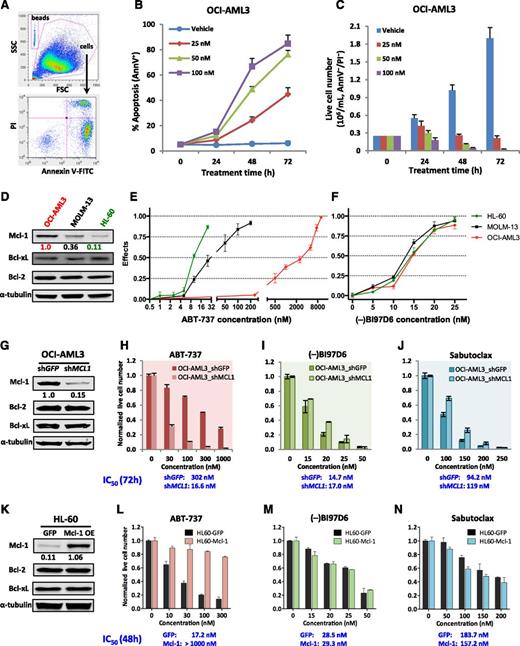
Pan–Bcl-2 inhibition by (–)BI97D6 overcomes Mcl-1–mediated drug resistance
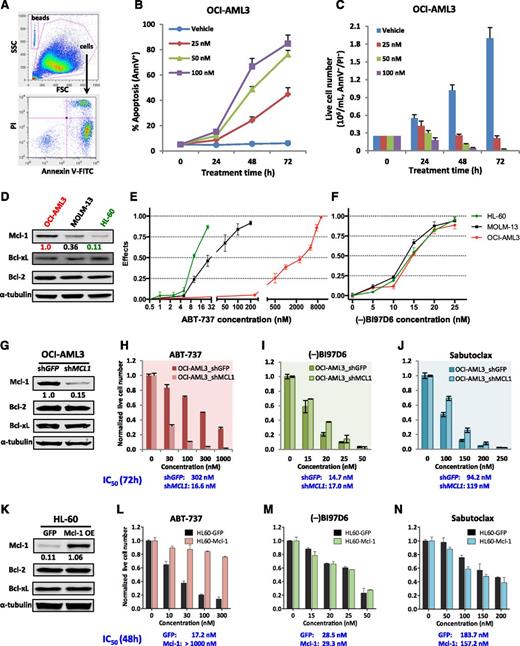
We previously demonstrated that OCI-AML3 cells, which express high levels of Mcl-1, were inherently resistant to ABT-737 or ABT-199.14,15 The pan–Bcl-2 inhibitor (–)BI97D6 has high binding affinity to Mcl-121 and disrupts Mcl-1/Bim association. Therefore, we examined whether (–)BI97D6 could overcome OCI-AML3 inherent resistance to ABT compounds. OCI-AML3 cells were treated with various concentrations of (–)BI97D6. The percentages of apoptotic cells (ie, Annexin V+) and absolute numbers of live cells (ie, Annexin V−/PI−) were determined by FACS analysis, and representative plots displaying the gating strategy are shown in Figure 2A. As shown in Figure 2B-C, (–)BI97D6 induced a dose- and time-dependent increase of apoptosis and a corresponding decrease of live cell numbers. Next the effects of (–)BI97D6 and ABT-737 were compared in 3 AML cell lines: OCI-AML3, MOLM-13, and HL-60. These cell lines were chosen because they represent AML cells expressing high, intermediate, and low levels of Mcl-1 while expressing similar levels of Bcl-2 and Bcl-xL (Figure 2D). ABT-737 potently killed Mcl-1low HL-60 cells (IC50 = 10.7 nM) and was less effective against Mcl-1intermediate MOLM-13 cells (IC50 = 27.9 nM). However, it was almost ineffective against Mcl-1high OCI-AML3 cells (IC50 = 1950 nM; Figure 2E). Conversely, all 3 cell lines displayed similar sensitivity to (–)BI97D6 (Figure 2F). Furthermore, (–)BI97D6 showed similar cytotoxic effects against 4 additional AML cell lines examined (supplemental Figure 4).
(–)BI97D6 effectively induces apoptosis in AML cells regardless of high expression of Mcl-1. (A) Representative FACS plots showing gating strategy and apoptosis induction by (–)BI97D6 in OCI-AML3 cells. (B-C) Time- and dose-dependent (B) induction of apoptosis and (C) reduction of live cell numbers of OCI-AML3 cells after (–)BI97D6 treatment. (D) Mcl-1 expression in 3 AML cell lines as determined by immunoblot densitometry using the Odyssey Infrared Imaging System. α-Tubulin served as loading control. The ratio of Mcl-1/α-tubulin was normalized to that of untreated OCI-AML3 cells. (E-F) The effects of (E) ABT-737 and (F) (–)BI97D6 on 3 AML cell lines with low, intermediate, or high expression of Mcl-1 protein. Effect = 1 – live cell numbertreated/live cell numbercontrol. (G) Immunoblot showing stable Mcl-1 knockdown by lentiviral shRNA in OCI-AML3 cells. (H-J) Comparison of the sensitivities of OCI-AML3 shGFP and shMCL1 cells to ABT-737, (–)BI97D6, and Sabutoclax. The cells were treated with indicated concentrations for 72 hours. (K) Immunoblot showing stable Mcl-1 overexpression in HL-60 cells. (L-N) Comparison of the sensitivities of HL60-GFP and HL60-Mcl-1 overexpressing cells to ABT-737, (–)BI97D6, and Sabutoclax. The cells were treated for 48 hours. The live cell numbers were enumerated by FACS analysis using CountBright counting beads and normalized to those of untreated controls. Calcusyn software was used to calculate the IC50 values based on live cell numbers. All data in line/bar graphs represent the means of triplicate experiments, with error bars indicating the standard deviations.
(–)BI97D6 effectively induces apoptosis in AML cells regardless of high expression of Mcl-1. (A) Representative FACS plots showing gating strategy and apoptosis induction by (–)BI97D6 in OCI-AML3 cells. (B-C) Time- and dose-dependent (B) induction of apoptosis and (C) reduction of live cell numbers of OCI-AML3 cells after (–)BI97D6 treatment. (D) Mcl-1 expression in 3 AML cell lines as determined by immunoblot densitometry using the Odyssey Infrared Imaging System. α-Tubulin served as loading control. The ratio of Mcl-1/α-tubulin was normalized to that of untreated OCI-AML3 cells. (E-F) The effects of (E) ABT-737 and (F) (–)BI97D6 on 3 AML cell lines with low, intermediate, or high expression of Mcl-1 protein. Effect = 1 – live cell numbertreated/live cell numbercontrol. (G) Immunoblot showing stable Mcl-1 knockdown by lentiviral shRNA in OCI-AML3 cells. (H-J) Comparison of the sensitivities of OCI-AML3 shGFP and shMCL1 cells to ABT-737, (–)BI97D6, and Sabutoclax. The cells were treated with indicated concentrations for 72 hours. (K) Immunoblot showing stable Mcl-1 overexpression in HL-60 cells. (L-N) Comparison of the sensitivities of HL60-GFP and HL60-Mcl-1 overexpressing cells to ABT-737, (–)BI97D6, and Sabutoclax. The cells were treated for 48 hours. The live cell numbers were enumerated by FACS analysis using CountBright counting beads and normalized to those of untreated controls. Calcusyn software was used to calculate the IC50 values based on live cell numbers. All data in line/bar graphs represent the means of triplicate experiments, with error bars indicating the standard deviations.
To further investigate the Mcl-1–mediated drug resistance, the MCL1 gene was stably knocked down by ectopic expression of a well-validated MCL1-specific shRNA14,15 (Figure 2G). Consistent with our previous data,15 Mcl-1 knockdown greatly sensitized OCI-AML3 cells to ABT-737 (Figure 2H). In contrast, (–)BI97D6 was equally potent against the control and MCL1 knockdown cells (72-hour IC50 = 14.7 and 17.0 nM, respectively; Figure 2I). A similar result was observed with another Mcl-1–targeting pan–Bcl-2 inhibitor, Sabutoclax (Figure 2J). HL-60 cells expressing low level of Mcl-1 are sensitive to ABT-737. We stably overexpressed Mcl-1 in HL-60 cells by ∼10-fold (Figure 2K). Mcl-1 overexpression conferred HL-60 cells high resistance to ABT-737 (Figure 2L) and ABT-199 (supplemental Figure 5). In contrast, the control and Mcl-1 overexpressing cells were similarly sensitive to the Mcl-1 targeting (–)BI97D6 or Sabutoclax (Figure 2M-N).
Together, these results indicate that (–)BI97D6 is able to overcome Mcl-1–mediated resistance to ABT-737. Although specific AML cell lines might depend on particular Bcl-2 antiapoptotic proteins for survival, the similar efficacy of (–)BI97D6 against 7 AML cell lines (supplemental Figure 4) and Mcl-1 knockdown or overexpressing cells implies that its cytotoxic effects probably result from collective inhibition of multiple antiapoptotic Bcl-2 proteins.
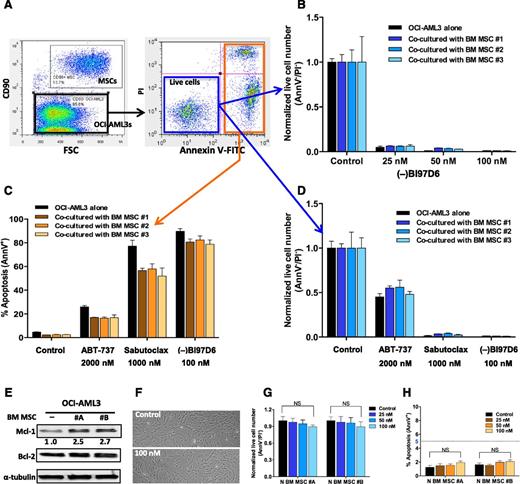
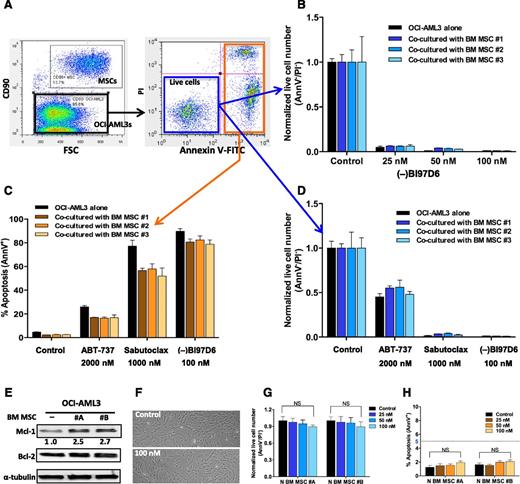
Pan–Bcl-2 inhibition abrogates BM MSC-mediated drug resistance
Over the last decade, tumor microenvironment has been increasingly implicated in tumor drug resistance.3 BM MSCs are critical components of the BM microenvironment. Using coculture models mimicking BM microenvironment, our group and others have shown that MSCs protect AML cells from conventional chemotherapeutics (eg, cytarabine and platinum analogs) and novel targeted agents (eg, ABT-737 and FI-700).24,40,41 In this study, we found that coculture with MSCs increased Mcl-1 protein in OCI-AML3 cells by more than twofold (Figure 3E). Because Mcl-1 contributes significantly to leukemia cell resistance to ABTs, we would expect that Mcl-1 inhibitors can abrogate MSC-mediated protection. To test this hypothesis, we cocultured OCI-AML3 cells with BM MSCs (Figure 3A) and found no significant difference in (–)BI97D6-mediated killing between cells cultured alone and cells cultured with BM MSCs. As shown in Figure 3B, (–)BI97D6 dramatically reduced live cell number in the presence of protective MSCs. In parallel, we tested the antileukemia effects of ABT-737 and Sabutoclax on cocultured OCI-AML3 cells. As expected, OCI-AML3 cells were resistant to 2 μM ABT-737 with or without MSC protection, whereas Sabutoclax (1 μM) induced marked decreases of live cell numbers comparable to 0.1 μM (–)BI97D6, even in the presence of BM MSCs (Figure 3C-D). Importantly, 72-hour exposure to 100 nM (–)BI97D6 had no apparent effects on the morphology, proliferation, or viability of BM MSCs (Figure 3F-H).
BM MSC coculture increases Mcl-1 protein level in OCI-AML3 cells and Mcl-1 inhibition by the pan–Bcl-2 inhibitor (–)BI97D6 abrogates BM MSC-mediated protection. (A) Representative FACS plots showing the gating strategy used to determine apoptosis and viability of OCI-AML3 cells cocultured with BM MSCs. (B) Viability of OCI-AML3 cells following treatment with increasing concentrations of (–)BI97D6 for 72 hours, with or without coculture with protective MSCs. The live cell number (AnnV−/PI−) was enumerated by FACS analysis using CountBright counting beads and normalized to the counts of untreated controls. (C) Apoptosis (AnnV+) as assessed by FACS in OCI-AML3 cells after incubation with indicated compounds for 72 hours; cells were cultured alone or cocultured with protective MSCs. (D) Live cell numbers after incubation with indicated compounds for 72 hours. The methodology is as described in B. Both Sabutoclax and (–)BI97D6 effectively killed OCI-AML3 cells cocultured with BM MSCs. (E) Coculture with BM MSCs for 24 hours significantly increased Mcl-1 protein level in OCI-AML3 cells. (F-H) (–)BI97D6 (100 nM) had minimal effects on BM MSC (F) morphology, (G) proliferation, and (H) viability. NS, not significant. All data in bar graphs represent the means of triplicate experiments, with error bars indicating the standard deviations.
BM MSC coculture increases Mcl-1 protein level in OCI-AML3 cells and Mcl-1 inhibition by the pan–Bcl-2 inhibitor (–)BI97D6 abrogates BM MSC-mediated protection. (A) Representative FACS plots showing the gating strategy used to determine apoptosis and viability of OCI-AML3 cells cocultured with BM MSCs. (B) Viability of OCI-AML3 cells following treatment with increasing concentrations of (–)BI97D6 for 72 hours, with or without coculture with protective MSCs. The live cell number (AnnV−/PI−) was enumerated by FACS analysis using CountBright counting beads and normalized to the counts of untreated controls. (C) Apoptosis (AnnV+) as assessed by FACS in OCI-AML3 cells after incubation with indicated compounds for 72 hours; cells were cultured alone or cocultured with protective MSCs. (D) Live cell numbers after incubation with indicated compounds for 72 hours. The methodology is as described in B. Both Sabutoclax and (–)BI97D6 effectively killed OCI-AML3 cells cocultured with BM MSCs. (E) Coculture with BM MSCs for 24 hours significantly increased Mcl-1 protein level in OCI-AML3 cells. (F-H) (–)BI97D6 (100 nM) had minimal effects on BM MSC (F) morphology, (G) proliferation, and (H) viability. NS, not significant. All data in bar graphs represent the means of triplicate experiments, with error bars indicating the standard deviations.
Supportive stromal cell cocultures have been reported to induce upregulation of MCL1 and other antiapoptotic BCL2 family genes.24,42 The effectiveness of (–)BI97D6 in abrogating stroma-mediated protection implies that development of Mcl-1–targeting pan–Bcl-2 inhibitors represent a promising strategy to overcome tumor microenvironment-mediated resistance.
(–)BI97D6 effectively induced apoptosis in primary myeloblasts from patients with refractory AML
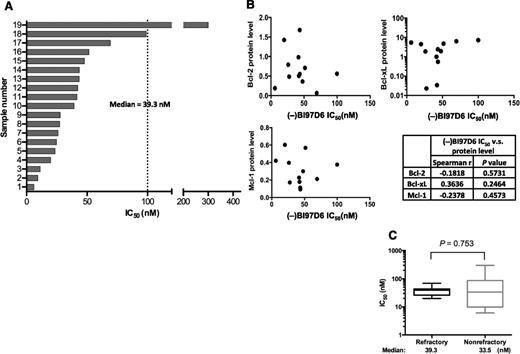
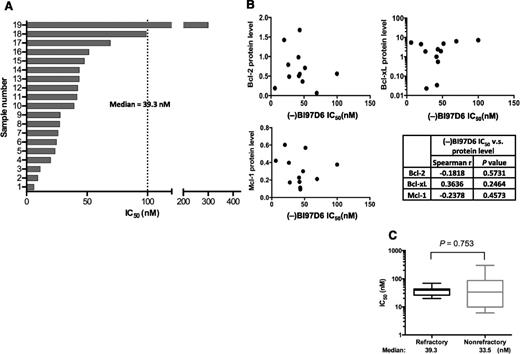
We next evaluated the efficacy of (–)BI97D6 on primary AML samples and found that it potently induced apoptosis of AML blast cells at low nanomolar concentrations (median 48-hour IC50 = 39.3 nM; Figure 4A). Importantly, AML samples with the FLT3 mutation (n = 3; IC50 = 19.9-51.4 nM) or NRAS mutation (n = 3; IC50 = 6.1-43.6 nM) showed sensitivities similar to AML myeloblasts without these poor prognosis mutations (Table 1).
(–)BI97D6 effectively kills primary AML myeloblasts from refractory patients. (A) (–)BI97D6 IC50 values in primary AML samples. Fresh mononuclear cells from AML patients were isolated and incubated with (–)BI97D6 for 48 hours. Calcusyn software was used to calculate the IC50 values based on live cell numbers (Annexin V−/PI−). Patient information is provided in Table 1. (B) Protein expression measured by quantitative immunoblot was plotted against the corresponding (–)BI97D6 IC50 values of patient samples (n = 12). No significant correlations were observed between IC50 values and the expression levels of Bcl-2, Bcl-xL, or Mcl-1 (Spearman’s rank correlation). (C) The IC50 values of (–)BI97D6 against refractory or nonrefractory primary AML samples. There is no significant difference in the median IC50 values (Mann-Whitney test).
(–)BI97D6 effectively kills primary AML myeloblasts from refractory patients. (A) (–)BI97D6 IC50 values in primary AML samples. Fresh mononuclear cells from AML patients were isolated and incubated with (–)BI97D6 for 48 hours. Calcusyn software was used to calculate the IC50 values based on live cell numbers (Annexin V−/PI−). Patient information is provided in Table 1. (B) Protein expression measured by quantitative immunoblot was plotted against the corresponding (–)BI97D6 IC50 values of patient samples (n = 12). No significant correlations were observed between IC50 values and the expression levels of Bcl-2, Bcl-xL, or Mcl-1 (Spearman’s rank correlation). (C) The IC50 values of (–)BI97D6 against refractory or nonrefractory primary AML samples. There is no significant difference in the median IC50 values (Mann-Whitney test).
We next determined whether the (–)BI97D6 IC50 values correlated with the expression of Bcl-2 proteins in primary AML cells. Unlike the Bcl-2–specific ABT-199, for which a significant correlation exists between IC50 and Bcl-2 protein levels,15 no statistically significant correlations were observed between (–)BI97D6 sensitivity and protein levels of Bcl-2, Bcl-xL, or Mcl-1 (Figure 4B). This finding further indicates that (–)BI97D6-induced apoptosis likely reflects simultaneous inhibition of multiple antiapoptotic Bcl-2 proteins rather than blockade of an individual member. Importantly, even samples from refractory AML patients were similarly sensitive to (–)BI97D6 (Figure 4C).
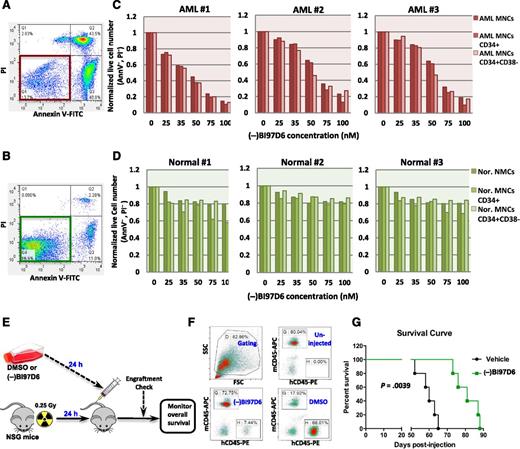
(–)BI97D6 potently kills leukemia stem/progenitor cells while sparing normal hematopoietic stem/progenitor cells
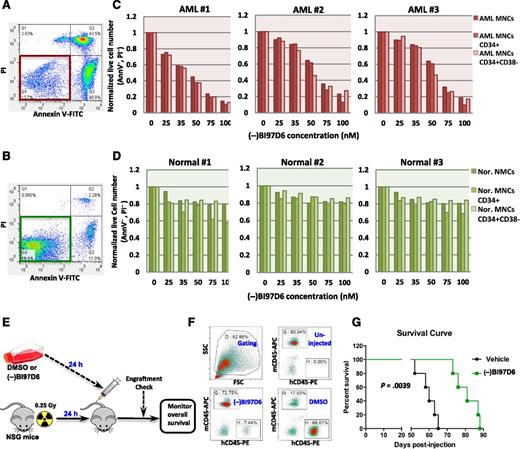
Leukemia stem cells (LSCs) are at the top of the hierarchy of malignant hematopoiesis and possess the ability to drive leukemogenesis. Although most leukemia cells are initially sensitive to conventional chemotherapies, LSCs are typically quiescent and resistant and thus can potentially drive leukemia relapse after an initial response. Although methods of prospectively identifying and isolating human LSCs remain controversial, AML LSCs are believed to be enriched in immunophenotypically defined CD34+CD38− blasts. To explore whether simultaneous inhibition of multiple antiapoptotic Bcl-2 proteins, including Mcl-1, could eliminate LSCs, we isolated BM mononuclear cells from 3 AML patients and 3 healthy donors. The numbers of live cells in the bulk, the CD34+, and the CD34+/CD38− fractions after treatment were measured via FACS (Figure 5A-B). The compound (–)BI97D6 induced marked decreases of live cell numbers in all 3 fractions of AML cells while sparing their normal counterparts (Figure 5C-D). To further examine its potential toxicity on normal hematopoietic stem/progenitor cells, we performed colony formation assays using BM mononuclear cells from 4 healthy donors. The methycellulose semisolid medium was added with 100 nM (−)BI97D6, a dose that actively kills AML cells. We found that (−)BI97D6 had only minimal effects on the numbers of burst forming unit erythroid (BFU-E), granulocyte-macrophage progenitor (CFU-GM), and CFU-granulocyte, erythroid, macrophage, megakaryocyte (CFU-GEMM) colonies (supplemental Figure 6), consistent with our flow cytometry results (Figure 5D).
Pan–Bcl-2 inhibition by (–)BI97D6 potently kills leukemia stem/progenitor cells at doses sparing normal hematopoietic stem/progenitor cells. (A-B) Representative FACS plots of (A) AML blast cells or (B) normal MNCs following treatment with 100 nM of (–)BI97D6 for 48 hours. (C-D) Change in live cell numbers (AnnV−/PI−) as a function of (–)BI97D6 concentration. Fresh AML or normal MNCs were isolated and treated with indicated doses of (–)BI97D6 for 48 hours. Live cell numbers were enumerated and normalized to untreated controls. (E) Diagram showing the experimental design. AML patient cells (1.0 × 106) were intravenously injected into NSG mice following 24-hour incubation with 100 nM (–)BI97D6 or DMSO (vehicle). (F) Representative FACS plots showing engraftment of human AML cells in mouse peripheral blood 6 weeks after injection. (–)BI97D6 pretreatment significantly reduced engraftment/progression of AML patient cells. (G) Kaplan-Meier survival curves for the mouse experiment described in E (5 mice per arm).
Pan–Bcl-2 inhibition by (–)BI97D6 potently kills leukemia stem/progenitor cells at doses sparing normal hematopoietic stem/progenitor cells. (A-B) Representative FACS plots of (A) AML blast cells or (B) normal MNCs following treatment with 100 nM of (–)BI97D6 for 48 hours. (C-D) Change in live cell numbers (AnnV−/PI−) as a function of (–)BI97D6 concentration. Fresh AML or normal MNCs were isolated and treated with indicated doses of (–)BI97D6 for 48 hours. Live cell numbers were enumerated and normalized to untreated controls. (E) Diagram showing the experimental design. AML patient cells (1.0 × 106) were intravenously injected into NSG mice following 24-hour incubation with 100 nM (–)BI97D6 or DMSO (vehicle). (F) Representative FACS plots showing engraftment of human AML cells in mouse peripheral blood 6 weeks after injection. (–)BI97D6 pretreatment significantly reduced engraftment/progression of AML patient cells. (G) Kaplan-Meier survival curves for the mouse experiment described in E (5 mice per arm).
Thus far, engraftment of human leukemias in a xeno-transplantation animal model represents the ultimate proof for the presence of LSCs. Accordingly, the capacity of a therapeutic agent to kill LSCs could be further evaluated if pretreatment with the drug in vitro could prevent or significantly postpone AML engraftment and progression in vivo. Figure 5E depicts the experimental design of the xeno-transplantation mouse model. The AML patient cells used here demonstrated their capacity of serial transplantation in NSG mice, reflecting the self-renewal ability of LSC cells. Leukemic cells were recovered from secondary transplanted mice, treated with 100 nM (–)BI97D6 or vehicle, and then intravenously injected into 6-week-old NSG mice. Six weeks after injection, peripheral blood was collected, stained for human and murine CD45, and analyzed by FACS. Human AML engraftment was confirmed in all injected mice by identification of hCD45+ cells in each animal (data not shown). However, the percentage of hCD45+ cells was higher in control mice than in mice injected with pretreated AML cells (representative flow plots; Figure 5F). Moreover, pretreatment of AML cells markedly prolonged mouse survival (Figure 5G; n = 5 per arm). The results of this xeno-transplantation study indicate that the Mcl-1–targeting pan–Bcl-2 inhibitor (–)BI97D6 effectively killed AML LSCs. This is consistent with a previous report that simultaneous inhibition of multiple antiapoptotic proteins by Sabutoclax inhibited blast crisis chronic myeloid leukemia stem cells while sparing normal hematopoietic cells.42
Discussion
Despite the significant advancement in targeted cancer therapies, current strategies still face significant challenges owing to acquired drug resistance. The majority of targeted therapeutics focuses on the upstream nodes of cancer signaling pathways. The initial response might be promising, but resistance is often inevitable because of various compensatory mechanisms mediated via the cross-wired cancer signaling pathways. The ultimate therapeutic effects of conventional chemotherapies, or novel targeted therapies, usually converge on apoptotic cell death. Therefore, targeting the downstream overexpressed Bcl-2 antiapoptotic proteins would appear to be a superior strategy because it directly elicits apoptosis in tumor cells and might minimize the development of drug resistance.
A recent study showed heterogeneous but overlapping expression of Bcl-2, Mcl-1, and Bcl-xL in 577 AML patient samples.43 Because the functional redundancy of Bcl-2 antiapoptotic proteins is the major cause of resistance to selective Bcl-2 antagonists (eg, ABT-199), concomitant inhibition of multiple Bcl-2 proteins can presumably overcome this resistance. This notion is supported by our finding that AML cells with high Mcl-1 expression were highly resistant to Bcl-2/Bcl-xL inhibitor ABT-737, whereas all AML cell lines tested showed similar sensitivity to the pan–Bcl-2 inhibitor (–)BI97D6.
Most putative pan–Bcl-2 inhibitors, such as obatoclax and gossypol, bind their targets with poor to moderate affinity and trigger cell death independent of Bax and Bak, suggesting additional off-target effects.44,45 For example, gossypol (AT-101) had been reported to induce cell death by endoplasmic reticulum stress-mediated mechanisms.46 The ApoG2 derivative (–)BI97D6 binds Bcl-2 antiapoptotic proteins with much higher affinity than other reported pan–Bcl-2 inhibitors (supplemental Table 1). We reason that the higher affinity makes it more selective and minimizes potential off-target effects. Unlike gossypol, (–)BI97D6 did not induce hallmarks of endoplasmic reticulum stress (supplemental Figure 7), such as DDIT3 upregulation or eIF2α phosphorylation.47,48 Instead, (–)BI97D6 induced multiple intrinsic apoptotic hallmarks, promoted externalization of plasma membrane phosphatidylserine within 12 hours (supplemental Figures 8 and 9), and required Bax or Bak for cell killing. Deficiency of Bim, Bax, or Bak all significantly reduced apoptosis induction by (–)BI97D6. Furthermore, (–)BI97D6 disrupted the associations of Mcl-1/Bim and Bcl-2/Bax, as would be expected for on-target activities of BH3 mimetics. Although we cannot rule out possible minor off-target activities of (–)BI97D6, especially when used at very high doses, our results suggest that (–)BI97D6 acts mainly as a BH3 mimetic, thus inducing cell death essentially via the Bax/Bak-dependent mitochondrial apoptosis pathway.
The role of Mcl-1 as a mediator of drug resistance has been a subject of intense investigation in recent years.13,23,49 Meanwhile, reverse-phase protein array analysis of putative AML LSCs found that these cells have high levels of Mcl-1.50 However, toxicity might be an issue when targeting proteins expressed in both leukemic cell and hematopoietic stem cells. In this regard, Opferman and colleagues reported that Mcl-1 might play an essential role in the survival of murine hematopoietic stem cells and early myeloid precursors. In the same study, murine AML cells were demonstrated to be more sensitive to Mcl-1 deletion than hematopoietic stem and progenitor cells,49 suggesting that a therapeutic window might exist. Also, pancytopenia and bone marrow failure, observed on MCL1 germ-line deletion, were not unequivocally related to Mcl-1’s antiapoptotic function because of increasing evidence for nonapoptotic functions of Bcl-2 family proteins.51-54 For example, Perciavalle et al found that an N-terminal truncated form of Mcl-1 located in the mitochondrial matrix is essential for normal mitochondrial fusion, ATP production, respiration, and other functions.55 Therefore, eliminating the Mcl-1 protein entirely, including its nonapoptotic functions, might be lethal to normal cells. If Mcl-1 has nonapoptotic functions independent of the BH3 domain interactions, then BH3 mimetics like (–)BI97D6 presumably do not interfere with these functions and can be better tolerated than MCL1 gene deletion. Indeed, our results demonstrated that Mcl-1 inhibition by (–)BI97D6 effectively killed AML cells while being well tolerated by normal hematopoietic stem/progenitor cells. Similarly, (–)BI97D6 treatment was tolerated by hepatocytes in a previous study,21 whereas MCL1 gene deletion was reported to cause hepatocyte toxicity in mice.56
LSCs are considered to be resistant to conventional chemotherapies and to drive leukemia relapse. Recent evidence suggests that most functionally defined LSCs have relatively low levels of reactive oxygen species and aberrantly overexpress Bcl-2 protein.57 Furthermore, Bcl-2–mediated oxidative phosphorylation is reportedly essential for LSC energy homeostasis, such that Bcl-2 inhibition reduces oxidative phosphorylation and selectively eradicates quiescent LSCs.45 However, other published results have demonstrated that suppression of Mcl-1 kills transformed AML cells, suggesting a critical role of Mcl-1 for LSC survival,13 although not ruling out a concomitant requirement for Bcl-2. Overall, it is still equivocal which Bcl-2 family proteins are critical for LSC survival. For this reason, it is germane that (–)BI97D6 binds not only Mcl-1 with high affinity (IC50 = 25 nM) but also retains relatively high binding affinity for Bcl-2 (IC50 = 31 nM). In agreement with this idea, the pan–Bcl-2 inhibitor effectively killed CD34+CD38− AML stem/progenitor cells while sparing normal hematopoietic stem/progenitor cells.
In summary, our studies indicated that (–)BI97D6 mediated its cytotoxicity mainly as a BH3 mimetic pan–Bcl-2 inhibitor to promote mitochondrial apoptosis. We demonstrated that inhibition of Mcl-1 by (–)BI97D6 abrogates intrinsic drug resistance (functional redundancy of antiapoptotic Bcl-2 family proteins) and extrinsic drug resistance (protective tumor microenvironment) of AML cells to ABT-737. Furthermore, pan–Bcl-2 inhibition effectively killed leukemia stem/progenitor cells. These results strongly encourage further development of Mcl-1–specific or pan-active Mcl-1–targeting BH3 mimetics to combat AML and other refractory cancers.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Teresa McQueen for administrative assistance and Dr Numsen Hail Jr and Kathryn Hale for advice and helpful comments on the manuscript.
This work was supported by National Institutes of Health, National Cancer Institute grants P01 CA-55164 (to M.A.), RO1 CA168517 (to M.P.), RO1 CA149668 (to M.P.), and PO1 CA081534 (to J.C.R.) and a Developmental Research Project award from MD Anderson Cancer Center Leukemia Specialized Program of Research Excellence grant CA-100632 (to P.P.R.).
Authorship
Contribution: R.P. conceived the study, designed and performed the research, analyzed and interpreted data, and wrote and edited the manuscript; V.R.R. performed the experiments and edited the manuscript; J.W. and M.P. contributed vital reagents; M.K. and J.C.R. interpreted the data and edited the manuscript; M.A. conceived the study, interpreted data, and edited the manuscript; and P.P.R. designed research, performed experiments, interpreted data, and wrote the manuscript.
Conflict-of-interest disclosure: M.A. and M.K. have sponsored research agreements from AbbVie. All other authors declare no competing financial interests.
Correspondence: Michael Andreeff, Department of Leukemia, Unit 448, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Houston, TX 77030; e-mail: mandreef@mdanderson.org.
References
Author notes
M.A. and P.P.R. contributed equally to this work.