Abstract
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare bone marrow failure disorder that manifests with hemolytic anemia, thrombosis, and peripheral blood cytopenias. The absence of two glycosylphosphatidylinositol (GPI)-anchored proteins, CD55 and CD59, leads to uncontrolled complement activation that accounts for hemolysis and other PNH manifestations. GPI anchor protein deficiency is almost always due to somatic mutations in phosphatidylinositol glycan class A (PIGA), a gene involved in the first step of GPI anchor biosynthesis; however, alternative mutations that cause PNH have recently been discovered. In addition, hypomorphic germ-line PIGA mutations that do not cause PNH have been shown to be responsible for a condition known as multiple congenital anomalies-hypotonia-seizures syndrome 2. Eculizumab, a first-in-class monoclonal antibody that inhibits terminal complement, is the treatment of choice for patients with severe manifestations of PNH. Bone marrow transplantation remains the only cure for PNH but should be reserved for patients with suboptimal response to eculizumab.
Introduction
Paroxysmal nocturnal hemoglobinuria (PNH) is a clonal hematopoietic stem cell disorder that manifests with hemolytic anemia, bone marrow failure, and thrombosis.1-4 One of the earliest descriptions of PNH was by Dr Paul Strübing, who in 1882 described a 29-year-old man who presented with fatigue, abdominal pain, and severe nocturnal paroxysms of hemoglobinuria.5 Strübing deduced that the hemolysis was occurring intravascularly as the patient’s plasma turned red following severe attacks of hemoglobinuria. Later reports by Marchiafava and Micheli led to the eponym, Marchiafava-Micheli syndrome, but it was Enneking, in 1925, who introduced the term paroxysmal nocturnal hemoglobinuria.6 In 1937, Thomas Ham reported that PNH erythrocytes were hemolyzed when incubated with normal, acidified serum.7 This seminal discovery resulted in the first diagnostic test for PNH, the acidified serum (Ham) test. The cell lysis following acidified serum appeared to be complement dependent because heat inactivation abrogated the reaction; however, it was not until 1954, with the discovery of the alternative pathway of complement activation, that complement was formally proven to cause the hemolysis of PNH red cells. In the 1980s, it was discovered that PNH cells display a global deficiency in a group of proteins affixed to the cell surface by a glycosylphosphatidylinositol (GPI) anchor. Two of the missing GPI anchored proteins (CD55 and CD59) regulate complement. A few years later, a genetic mutation (phosphatidylinositol glycan class A [PIGA]) responsible for the GPI anchor protein deficiency was discovered,8-11 and most recently, a humanized monoclonal antibody that inhibits terminal complement activation has been shown to ameliorate hemolysis and thrombosis and improve quality of life in PNH patients.12
Pathophysiology
Hemolysis in PNH is complement mediated and is a direct result of PNH cells acquiring a deficiency of complement regulatory proteins. The disease begins with the expansion of a hematopoietic stem cell that has a severe deficiency or absence for GPI, a glycolipid moiety that anchors >150 different proteins to the cell surface (Figure 1). GPI anchor deficiency in virtually all PNH cases is the result of a somatic mutation in PIGA, an X-linked gene whose product is required for the first step in GPI anchor biosynthesis. This results in the deficiency of complement inhibitory proteins CD55 and CD59 that leads to chronic complement-mediated hemolysis of the GPI-deficient erythrocytes, as well as activation of platelets, monocytes, and granulocytes. There are >12 GPI-anchored proteins (GPI-APs) on hematopoietic cells, including blood group antigens, adhesion molecules, and complement regulatory proteins. GPI-APs also serve as receptors for proaerolysin, a pore-forming bacterial toxin secreted by Aeromonas hydrophila13,14 ; however, it is the absence of CD55 and CD59 that accounts for most of the clinical manifestations of PNH.15,16 CD59 is a 19 000-Da glycoprotein that directly interacts with the membrane attack complex (MAC) to prevent lytic pore formation by blocking the aggregation of C9.16 CD55, a 68 000-Da glycoprotein, functions to accelerate the rate of destruction of membrane-bound C3 convertase.17 Hence, CD55 reduces the amount of C3 that is cleaved, and CD59 reduces the number of MAC that is formed (Figure 2). Central to these mechanisms is the alternative pathway of complement activation. In this pathway, C3 protein spontaneously hydrolyzes and leads to the formation of C3 convertase (this process is also known as tick-over). Hemolysis in PNH is chronic because of a continuous state of complement activation through tick-over, but paroxysms resulting in brisk hemolysis coincide with increases in complement activation triggered by surgery, infection, or inflammation. The mechanism of intravascular hemolysis begins with the increased activity of C3 convertases on the surface of PNH erythrocytes as a result of the lack of CD55. This leads to activation of C3, C5, and the terminal pathway of complement culminating in the formation of the MAC. Under normal conditions, formation of the MAC is under the regulation of CD59. The absence of CD59 on PNH erythrocytes leads to uncontrolled formation of the MAC resulting in complement-mediated intravascular hemolysis. Extravascular hemolysis in PNH begins with increased opsonization of PNH erythrocytes by complement fragments (mostly C3d). This is the result of the lack of CD55. Opsonized erythrocytes are cleared and destroyed by cells of the reticulo-endothelial system.18 Extravascular hemolysis is often inconspicuous in the untreated PNH patient because signs and symptoms of intravascular hemolysis dominate. However, extravascular hemolysis can become the primary mechanism of hemolysis in patients treated with the terminal complement inhibitor, eculizumab (Figure 2).
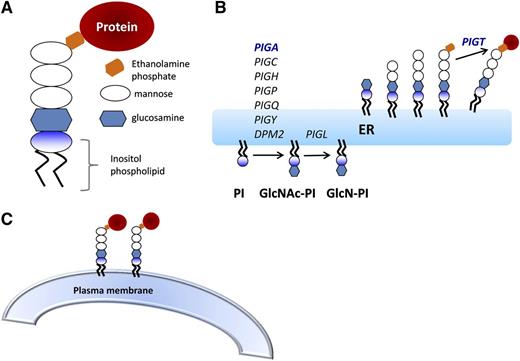
GPI anchor biosynthesis. (A) Core structure of the GPI anchor. The inositol-phospholipid (PI) is anchors into the lipid bilayer of the plasma membrane. The glycan core consists of a molecule of N-glucosamine, 3 manose molecules (Man), and a molecule of ethanolamine phosphate. The protein is covalently attached through an amide bond to an ethanolamine on the terminal mannose. (B) GPI anchor biosynthesis takes place in the endoplasmic reticulum. PIGA is 1 of 7 subunits involved in the first step of GPI anchor biosynthesis. There are ≥10 additional steps and >25 genes involved. After the protein is attached to the GPI anchor, the mature GPI-anchored protein goes to the Golgi, where fatty acid remodeling occurs and (C) eventually the GPI anchored protein is transported to the plasma membrane.
GPI anchor biosynthesis. (A) Core structure of the GPI anchor. The inositol-phospholipid (PI) is anchors into the lipid bilayer of the plasma membrane. The glycan core consists of a molecule of N-glucosamine, 3 manose molecules (Man), and a molecule of ethanolamine phosphate. The protein is covalently attached through an amide bond to an ethanolamine on the terminal mannose. (B) GPI anchor biosynthesis takes place in the endoplasmic reticulum. PIGA is 1 of 7 subunits involved in the first step of GPI anchor biosynthesis. There are ≥10 additional steps and >25 genes involved. After the protein is attached to the GPI anchor, the mature GPI-anchored protein goes to the Golgi, where fatty acid remodeling occurs and (C) eventually the GPI anchored protein is transported to the plasma membrane.
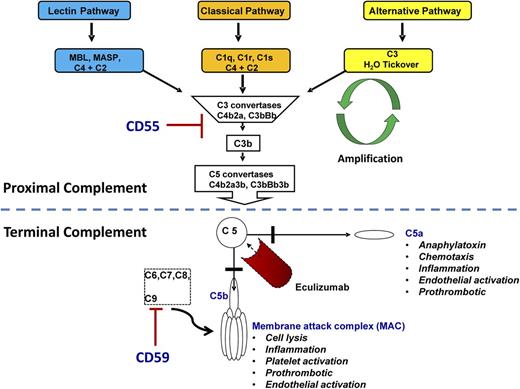
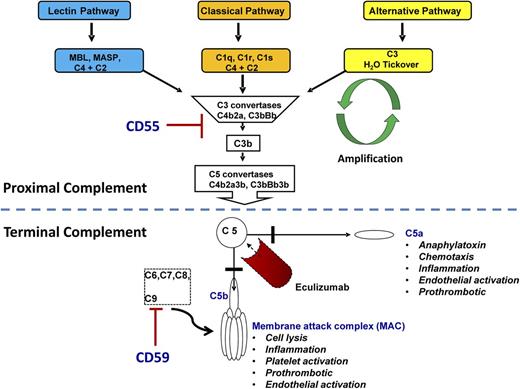
Complement regulation and eculizumab. The lectin, classical, and alternative pathways converge at the point of C3 activation. In PNH, hemolysis is usually chronic because the alternative pathway is always in a low-level activation state through a process known as tick-over. Terminal complement begins with cleavage of C5 to C5a and C5b. C5b oligomerizes with C6, C7, C8, and multiple C9 molecules to form the MAC. CD55 inhibits proximal complement activation by blocking the formation of C3 convertases; CD59 inhibits terminal complement activation by preventing the incorporation of C9 into the MAC. The absence of CD55 and CD59 on PNH cells leads to hemolysis, inflammation, platelet activation, and thrombosis. Eculizumab inhibits terminal complement activation by binding to C5 and preventing generation of C5a and C5b.
Complement regulation and eculizumab. The lectin, classical, and alternative pathways converge at the point of C3 activation. In PNH, hemolysis is usually chronic because the alternative pathway is always in a low-level activation state through a process known as tick-over. Terminal complement begins with cleavage of C5 to C5a and C5b. C5b oligomerizes with C6, C7, C8, and multiple C9 molecules to form the MAC. CD55 inhibits proximal complement activation by blocking the formation of C3 convertases; CD59 inhibits terminal complement activation by preventing the incorporation of C9 into the MAC. The absence of CD55 and CD59 on PNH cells leads to hemolysis, inflammation, platelet activation, and thrombosis. Eculizumab inhibits terminal complement activation by binding to C5 and preventing generation of C5a and C5b.
Genetics
PIGA mutations that lead to PNH
GPI biosynthesis is a post-translational event that occurs in the endoplasmic reticulum.19 There are >10 steps and ≥26 gene products required. The PIGA gene product is 1 of 7 proteins involved in the first step of GPI anchor biosynthesis. Theoretically, a mutation of any gene in the pathway could lead to PNH; however, until recently PIGA was the only mutated gene found in PNH patients.8,10,11,20 This is because PIGA is on the X chromosome; thus, a single somatic mutation in a hematopoietic stem cell is sufficient to produce a PNH phenotype (men have a single X chromosome and women have only one active X chromosome due to lyonization). The remaining known genes in the GPI anchor biosynthethic pathway are on autosomes; thus, 2 hits disrupting function on both alleles would be necessary to interrupt GPI anchor synthesis. The 16-kb-long PIGA gene (mendelian inheritance in man [MIM] #311770) is located at Xp22.1; it encodes for a protein that contains 484 amino acids (60 kDa).9 An intronless pseudogene has been found on chromosome 12q21.21 Numerous somatic mutations throughout the coding region of the PIGA gene have been described in PNH patients. There are no mutational hot spots, although exon 2, which contains almost half of the coding region, is the exon where most mutations occur. Most PIGA mutations are small insertions or deletions, usually 1 or 2 bp, which result in a frameshift in the coding region and consequently a shortened, nonfunctional product.22 Although PIGA function is usually abolished by these frameshift mutations, missense mutations, have also been described where the product of the mutated PIGA gene has some residual activity.
PNH stem cell and bone marrow failure
To cause PNH, PIGA mutations must occur in a self-renewing, hematopoietic stem cell and must achieve clonal dominance.23,24 The mechanisms leading to the clonal expansion and dominance of PNH stem cells remain a topic of continued investigation. Any hypotheisis must also account for the close pathophysiologic relationship between PNH and acquired aplastic anemia, a T cell-mediated autoimmune disease characterized by depletion of hematopoietic stem cells. The leading hypothesis is that PNH stem cells have a conditional survival advantage in the setting of an autoimmune attack (eg, aplastic anemia) that targets the bone marrow.25-27 One hypothesis involves natural killer group 2, member D (NKG2D)-mediated immunity, which is activated by the expression of ligands such as major histocompatibility complex class I chain-related peptides A and B (MICA/B) and cytomegalovirus UL-16 binding proteins (ULBPs).28,29 MICA/B are transmembrane proteins, but the ULBPs are GPI linked. NKG2D is a common receptor for MICA/B and the ULBPs. It is expressed on natural killer cells and CD8+ cytotoxic T cells. Engagement of NKG2D with its ligands (MICA/B and ULBPs) promotes cell death of the NKG2D ligand-expressing cells by the NKG2D+ effectors; thus, PNH cells would be relatively spared from effector cell-mediated killing because they lack GPI-anchored ULBPs. Recently, it has been proposed that CD1d-restricted, GPI-specific T cells might be responsible for the immune killing in PNH.30 Under this scenario, PNH cells would be spared immune-mediated killing because CD1d has been shown to associate with GPI. Others have shown that mutations that confer a survival advantage to the PNH clone can contribute to clonal outgrowth.31
Other mutations that cause PNH
The absence of CD59 is most responsible for the clinical manifestations in PNH. Accordingly, rare cases of inherited mutations in CD59 leading to loss of CD59 on the cell surface have been well documented.32,33 The phenotype of these patients mimics PNH in that they manifest with chronic intravascular hemolysis with paroxysmal flares of hemolysis and a propensity for thrombosis. Unlike PNH patients, those with inherited CD59 deficiency also present with relapsing immune-mediated peripheral neuropathy. In classical PNH, the CD59 deficiency is only found on the blood cells; in patients with germ-line CD59 mutations, CD59 is deficient in all cells in the body. These data suggest that germ-line CD59 deficiency is associated with demyelination via activation of terminal complement.
Recently a 44-year-old man with paroxysms of hemolysis, abdominal pain, fatigue, and headache was found to have GPI-AP-deficient blood cells in multiple lineages but wild-type PIGA. Ultradeep genomic sequencing revealed that the patient was born with a heterozygous germ-line splice site mutation in phosphatidylinositol glycan class T (PIGT) and later acquired a somatic 8-MB deletion involving the other PIGT allele in a myeloid stem cell.34 PIGT is a component of the transamidase complex that is responsible for the attachment of the preassembled GPI anchors to proteins.35,36 The second hit abolished PIGT function in myeloid stem cell, resulting in loss of GPI and clinical manifestations of PNH. The hemolysis in patients with inherited CD59 deficiency and the patient with the compound heterozygous mutation in PIGT responded to terminal complement inhibition with eculizumab.34,37
PIGA mutations that do not cause PNH
Somatic PIGA mutations arising from hematopoietic cells can be found at low frequency (∼1 in 50 000 granulocytes) in healthy control subjects.24,38 These mutations arise from colony-forming cells. Because normal and PIGA mutant colony-forming cells do not self-renew and only survive for 3 to 4 months, these cells cannot contribute to disease. PNH granulocytes (0.01-5%) can also be found in up to 25% of patients with myelodysplastic syndromes (MDS); however, unlike acquired aplastic anemia, it is extremely rare for PNH to evolve from MDS patients.39-41 These small PNH populations in MDS appear not to be clinically relevant because the PIGA mutations in MDS are transient and also arise from colony-forming cells rather than hematopoietic stem cells.42 In contrast, PIGA mutations in PNH patients and patients with acquired aplastic anemia arise from a multipotent hematopoietic stem cell and are found in all lineages, including T lymphocytes.42
Germ-line PIGA loss-of-function mutations were thought to be embryonic lethal.43,44 Indeed, generation of piga knockout mice was unsuccessful. Targeted disruption of PIGA in human-induced pluripotent stem cells results in a block in embryonic development before mesoderm differentiation due to perturbed signaling through bone morphogenic protein 4.45 Although germ-line PIGA null mutations are embryonic lethal, hypomorphic PIGA mutations are responsible for the X-linked form of a recently recognized syndrome known as multiple congenital anomalies–hypotonia-seizure syndrome 2 (MIM 300818).46-49 Children born with hypomorphic PIGA mutations present with severe intellectual disability, dysmorphic facial features, seizures, and early death. Hypomorphic GPI-AP deficiency is most conspicuous on granulocytes. The red cells from these patients have little to no GPI anchor deficiency and no hemolysis; however, the severe phenotype associated with partial deficiency of GPI-APs demonstrates that 1 or more GPI-APs is critical in early development.
Diagnosis and classification of PNH
PNH is a clinical diagnosis that should be confirmed with peripheral blood flow cytometry to detect the absence or severe deficiency of GPI-APs on ≥2 lineages.50,51 Loss of GPI-APs is detected after staining cells with monoclonal antibodies and a reagent known as fluorescent aerolysin (FLAER).52 FLAER is a fluorescein-tagged proaerolysin variant that binds the glycan portion of the GPI anchor. Consensus guidelines for detecting GPI anchor-deficient blood cells that use FLAER in combination with several monoclonal antibodies have been published.53 A classification scheme, proposed by the International PNH Interest Group, includes 3 main categories of PNH: (1) classical PNH, which includes hemolytic and thrombotic patients; (2) PNH in the context of other primary bone marrow disorders, such as aplastic anemia or myelodysplastic syndrome; and (3) subclinical PNH, in which patients have small PNH clones but no clinical or laboratory evidence of hemolysis or thrombosis.54 This classification scheme has resulted in some confusion because varying degrees of bone marrow failure underlie virtually all cases of PNH; thus, the distinction between 3 categories may be difficult in some cases.
Clinical manifestations
Anemia
Anemia in PNH is often multifactorial and may result from a combination of hemolysis and bone marrow failure. Intravascular hemolysis with moderate to severe anemia, an elevated reticulocyte count, and up to a 10-fold increase in lactate dehydrogenase (LDH) is common in classical PNH. Patients with classical PNH often have a high (>50%) percentage of PNH granulocytes. PNH in the context of other primary marrow disorders usually refers to acquired aplastic anemia.55 The anemia in these patients is primarily due to bone marrow failure; thus, these patients frequently have hypocellular bone marrows, more severe thrombocytopenia, small PNH clones, lower reticulocyte counts, and modest or no elevation in LDH levels. Thrombosis may occur but is less common than in patients with classical PNH. Patients with subclinical PNH are by definition asymptomatic with normal or near normal blood counts and few (usually <10%) PNH granulocytes. Often these patients have a diagnosis of mild aplastic anemia or have recovered hematopoiesis after treatment of acquired aplastic anemia.56 Expansion of the PNH clone and PNH symptoms may accompany relapse of their aplastic anemia.
Thrombosis
Thrombosis leads to severe morbidity and is the most common cause of mortality in PNH.57 Thrombosis in PNH may occur at any site; however, venous thrombosis is more common than arterial. For unclear reasons, common sites include intraabdominal (hepatic, portal, mesenteric, splenic, etc) and cerebral (sagittal and cavernous sinus) veins, with hepatic vein thrombosis (Budd-Chiari syndrome) being the most common site of thrombosis in PNH. Deep venous thrombosis, pulmonary emboli, and dermal thrombosis are also relatively common.
Thrombophilia in PNH is multifactorial. The absence of GPI-anchored complement regulatory proteins (CD55 and CD59) on PNH platelets leads to prothrombotic microparticles.58 High levels of free hemoglobin leads to scavenging of nitric oxide (NO), which has been implicated in contributing to platelet activation and aggregation.59 Complement activation also contributes to the prothrombotic tendency of PNH patients. Specifically, C5a may result in proinflammatory and prothrombotic processes by generating inflammatory cytokines such as interleukin-6, interleukin-8, and tumor necrosis factor-α.60 Last, defective fibrinolysis resulting from deficiency or absence of GPI-linked proteins such as urokinase-type plasminogen antivator receptor,61 heparan sulfate, and a GPI anchored coreceptor for tissue factor pathway inhibitor62 have been speculated to contribute to the thrombophilic state in PNH. It is unclear which of these mechanisms contribute most to thrombosis in PNH; however, complement inhibition is the most effective strategy to stop thrombosis in PNH.63,64 Thrombosis may occur in any PNH patient, but those with a large percentage of PNH cells (>50% granulocytes) are at greatest risk.4,65 Anticoagulation and eculizumab are indication for acute thrombotic events; however, primary prophylactic anticoagulation has not been proven to be beneficial in PNH.57 It is also unclear as to whether lifelong anticoagulation is necessary for secondary prophylaxis in PNH patients who are well controlled on eculizumab.66
Smooth muscle dystonia
Abdominal pain, esophageal spasm, dysphagia, and erectile dysfunction are common symptoms associated with classical PNH and are a direct consequence of intravascular hemolysis and the release of free hemoglobin.59,65 Free hemoglobin is normally cleared by haptoglobin, CD163, and hemopexin. These clearing mechanisms are overwhelmed in PNH and lead to accumulation of high levels of free hemoglobin in the plasma and consequently depletion of NO. Free hemoglobin is a potent NO scavenger; the 2 molecules undergo a fast and irreversible reaction that results in the production of nitrate and methemoglobin. Normally, NO is synthesized by endothelial cells and functions to maintain smooth muscle relaxation and inhibit platelet activation and aggregation. The deficiency of NO as a result of scavenging by free hemoglobin contributes to deregulation of smooth muscle tone and platelet activation. Acccordingly, smooth muscle dystonias are more common in patients with a large PNH clone size.65
Other manifestations
PNH patients have a greater than sixfold increased risk of chronic kidney disease.67 Renal tubular damage is caused by microvascular thrombosis and accumulation of iron deposits. Mild to moderate pulmonary hypertension is more common that previously recognized.68,69 Raised pulmonary pressures and reduced right ventricular function caused by subclinical microthrombi and hemolysis-associated NO scavenging contribute to symptoms of fatigue and dyspnea.
Treatment
Terminal complement inhibition with eculizumab and allogeneic bone marrow transplantation (BMT) are the only widely effective therapies for patients with classical PNH. Corticosteroids can improve hemoglobin levels and reduce hemolysis is some PNH patients, but the long-term toxicity and limited efficacy limits enthusiasm for these agents.
Eculizumab
Eculizumab is a humanized monoclonal antibody that blocks terminal complement by binding to C5 and is the only US Food and Drug Administration-approved therapy for PNH.12,70-72 The drug is administered intravenously every 7 days for the first 5 weeks and then biweekly thereafter. Eculizumab inhibits the formation of the MAC and in doing so compensates for the CD59 deficiency of PNH patients (Figure 1). It does not compensate for the CD55 deficiency; thus, eculizumab is highly effective in abrogating the intravascular hemolysis in PNH, but most PNH patients on eculizumab will continue to experience mild to moderate extravascular hemolysis due to C3d deposition on the PNH red cells.18 This explains why >50% of PNH patients treated with eculizumab develop a positive direct antiglobulin test (C3 positive but IgG negative) in conjunction with a mild to moderate anemia and elevated reticulocyte count.73 A common side effect of eculizumab, headache, appears to be a consequence of acutely increasing NO levels and is experienced by up to 50% of patients with the first dose.74 Headache is rarely reported after the first several doses. The most serious risk of terminal complement blockade is life-threatening Neisserial infections (roughly 0.5%/year or 5% after 10 years). Thus, all patients treated with eculizumab should be vaccinated against Neisseria. In severe PNH cases, especially those with concomitant thrombosis, administration of eculizumab and vaccination can be performed on the same day. In such cases, 2 weeks of prophylactic therapy with ciprofloxacin is recommended. Penicillin prophylaxis is also advocated by some investigators, especially in younger patients, but this has not been formally studied.
Despite the limitations described above, eculizumab is highly effective in treating PNH and has changed the natural history of the disease.63,71,72,75 The efficacy and safety of eculizumab has been demonstrated in 2 multinational phase 3 trials and a multinational extension study. The drug is highly effective in stopping intravascular hemolysis, eliminating or decreasing the need for red cell transfusions, improving quality of life, and reducing the risk of thrombosis, the leading cause of mortality from PNH. It has also been shown to improve renal function and to reduce prothrombotic and proinflammatory markers in PNH patients.64,67 Unfortunately, the long-term outcome (median follow-up >7 years) of the phase 3 multinational studies has not been published; thus, we still do not know what percentage of these patients remain on the drug, have breakthrough hemolysis, and remain transfusion independent beyond 5 years.
Eculizumab is expensive and must be administered indefinitely for a sustained response; thus, patients with mild or no symptoms should be followed with watchful waiting. Severe anemia, thrombosis, frequent pain paroxysms, debilitating fatigue, worsening renal insufficiency, or dyspnea are good indications to initiate therapy.51 Therapeutic decisions should not be based solely on the PNH clone size; however, patients with a large clone (>50% PNH granulocytes and >10% PNH red cells) coupled with a markedly elevated LDH (indicator of intravascular hemolysis) and a robust reticulocyte count (indicator of adequate bone marrow reserve) are most likely to benefit. Eculizumab does not alleviate bone marrow failure. Patients with ongoing bone marrow failure from aplastic anemia (hypocellular bone marrow, severe thrombocytopenia, and a relatively low reticulocyte count) are less likely to derive benefit from eculizumab. For these patients, therapy should address the underlying bone marrow failure.
The majority of classical PNH patients will respond to eculizumab; however, the hemoglobin response is highly variable and may depend on underlying bone marrow failure, concurrent inflammatory conditions, genetic factors, and the size of the PNH red cell clone following therapy.76 In fact, 25% to 35% of patients continue to require red cell transfusions despite treatment with eculizumab. The most common reason for continued transfusions is extravascular hemolysis. An increase in the percentage of PNH red cells after eculizumab therapy correlates with response but also with extravascular hemolysis. The PNH red cells that are protected by eculizumab are CD55 deficient and thus are susceptible to opsonization by C3 and premature removal in the spleen.18 This explains why >50% of PNH patients (Coombs negative at diagnosis) become Coombs positive (IgG− and C3+) after treatment with eculizumab. Interestingly, up to 10% of PNH patients treated with eculizumab have a decrease in the percentage of PNH erythrocytes despite a large percentage of PNH granulocytes.76 These patients achieve normal hemoglobin levels without the aid of transfusions. Pharmacogenetics has also been shown to influence response to therapy. Polymorphisms in the complement receptor 1 (CR1) gene are associated with response to eculizumab. CR1, through binding C3b and C4b, enhances the decay of the C3 and C5 convertases.77 The density of CR1 on the surface of red cells modulates binding of C3 fragments to the GPI-negative red cells when C5 is inhibited. PNH patients with polymorphisms in CR1 that lead to low CR1 levels (L/L genotype) are more likely to be suboptimal responders to eculizumab than patients with intermediate (H/L genotype) or high (H/H genotype) levels of CR1.
More recently, it has been discovered that a single missense C5 heterozygous mutation, c.2654G→A, prevents binding and blockade by eculizumab while retaining the functional capacity to cause hemolysis.78 The polymorphism accounts for the poor response to eculizmumab in patients carrying the mutation. The c.2654G→A mutation is present in 3.5% of the Japanese population and has not yet been described in other ethnic groups.
Monitoring the PNH patient on eculizumab
Patients on eculizumab should be monitored with a complete blood count, reticulocyte count, LDH, and biochemical profile weekly for the first 4 weeks and then at least monthly thereafter (Table 1). A direct antiglobulin test should be obtained in patients with evidence of persistent hemolysis, and PNH flow cytometry should by obtained yearly because the PNH clone size may fluctuate over time. The LDH usually returns to normal or near normal within days to weeks after starting eculizumab; however, the reticulocyte count usually remains elevated and the hemoglobin response is highly variable. The reticulocyte count often remains elevated because most PNH patients on eculizumab continue to have some extravascular hemolysis due to deposition of C3 fragments on the PNH red cells. The hemoglobin response is largely dependent on the degree of extravascular hemolysis and the amount of underlying bone marrow failure.
In classical PNH patients who are transfusion dependent, a marked decrease in red cell transfusions is observed in most patients, with >70% achieving transfusion independence. Breakthrough intravascular hemolysis and a return of PNH symptoms occurs in <5% of PNH patients treated with eculizumab. This typically occurs 1 or 2 days before the next scheduled dose and is accompanied by a spike in the LDH level. If this occurs on a regular basis, the interval between dosing can be shortened to 12 or 13 days or the dose of eculizumab can be increased. It is also important to recognize that increased complement activation that accompanies infections (eg, influenza or viral gastroenteritis) or trauma can also result in transient breakthrough hemolysis. These single episodes of breakthrough hemolysis do not require a change in dosing because patients usually return to their baseline hemoglobin once the infection or inflammation has resolved.
BMT
BMT should not be offered as initial therapy for patients with classical PNH given the risks of transplant-related morbidity and mortality.79,80 Exceptions are PNH patients in countries where eculizumab is not available. BMT is also a reasonable option for patients who do not respond to eculizumab therapy due heterozygous c.2654G→A mutations in C5 or the rare patient where eculizumab does not entirely block intravascular hemolysis due to persistent inflammation.76 Patients meeting criteria for severe aplastic anemia with PNH clones continue to be good candidates for BMT if they are young and have a suitable donor. A myeloablative conditioning regimen is not required to eradicate the PNH clone. Allogeneic BMT following non-myeloablative conditioning regimens can cure PNH.81,82 Whether or not there is an advantage to the non-myeloablative approach will require further study; however, non-myeloablative regimens may be preferable in young patients seeking to maintain fertility or patients with moderate organ dysfunction who may not tolerate a myeloablative regimen. Because BMT is the only curative therapy available for PNH, continued use and investigation of this approach in selected patients is reasonable. Recent advances in mitigating graft-versus-host disease such as post-transplant high-dose cyclophosphamide may particularly effective in nonmalignant hematopoietic diseases such as PNH.83,84
Conclusions
Improved knowledge of the molecular and cellular underpinnings of PNH over the last 2 decades has resulted in greater understanding of the biology and natural history of PNH. Recent studies with the monoclonal antibody, eculizumab, demonstrate that terminal complement inhibition controls most of the symptoms and life-threatening complications of PNH. A large international PNH registry has been established. Data from this registry should help define the natural history of PNH since the introduction of therapy that inhibits terminal complement.85 In the coming years, novel inhibitors of the alternative pathway of complement86,87 and complement inhibitors with extended half-lives are likely to further improve quality of life for PNH patients.
Acknowledgments
This work was supported by National Institutes of Health, National Cancer Institute grant P01CA70970 and Maryland State Stem Cell Fund/Technology Development Corporation Maryland Stem Cell Research Fund-0041 (R.A.B.).
Authorship
Contribution: R.A.B. wrote the manuscript.
Conflict-of-interest disclosure: R.A.B. serves on the Alexion Pharmaceuticals International Advisory Board.
Correspondence: Robert A. Brodsky, Ross Research Building, Room 1025, 720 Rutland Ave, Baltimore, MD 21205-2196; e-mail brodsro@jhmi.edu.