Retrospective studies have suggested that older adolescents and young adults (AYAs) with acute lymphoblastic leukemia (ALL) have better survival rates when treated using a pediatric ALL regimen administered by pediatric treatment teams. To address the feasibility and efficacy of using a pediatric treatment regimen for AYA patients with newly diagnosed ALL administered by adult treatment teams, we performed a prospective study, CALGB 10403, with doses and schedule identical to those in the Children's Oncology Group study AALL0232. From 2007 to 2012, 318 patients were enrolled; 295 were eligible and evaluable for response. Median age was 24 years (range, 17-39 years). Use of the pediatric regimen was safe; overall treatment-related mortality was 3%, and there were only 2 postremission deaths. Median event-free survival (EFS) was 78.1 months (95% confidence interval [CI], 41.8 to not reached), more than double the historical control of 30 months (95% CI, 22-38 months); 3-year EFS was 59% (95% CI, 54%-65%). Median overall survival (OS) was not reached. Estimated 3-year OS was 73% (95% CI, 68%-78%). Pretreatment risk factors associated with worse treatment outcomes included obesity and presence of the Philadelphia-like gene expression signature. Use of a pediatric regimen for AYAs with ALL up to age 40 years was feasible and effective, resulting in improved survival rates compared with historical controls. CALGB 10403 can be considered a new treatment standard upon which to build for improving survival for AYAs with ALL. This trial was registered at www.clinicaltrials.gov as #NCT00558519.
Using an intensive pediatric regimen for AYAs with ALL is feasible.
High rates of EFS and OS were seen compared with historical controls.
Visual Abstract
Introduction
Treatment outcomes for acute lymphoblastic leukemia (ALL) in children are 1 of the tremendous successes of combination chemotherapy in oncology, with high survival rates of 80% to 90%.1 In contrast, treatment of adults with ALL has been much less successful, with overall survival (OS) rates of only 30% to 40%, despite equivalent complete remission (CR) rates >90%.2-6 To better understand the potential causes of these dramatic differences in survival, a number of retrospective studies were performed, demonstrating surprising differences in outcomes for adolescents and young adults (AYAs; age 16-39 years) depending on trial enrollment in pediatric compared with adult cooperative group studies.7-10 In almost all of these analyses, AYA patients had significantly better outcomes when treated in pediatric cooperative trials. Despite the evolution of most adult treatment regimens from the multiagent approach employed by pediatric groups worldwide, there were clear differences in treatment design. Pediatric groups employed significantly more intensive dosing of several key therapeutic agents in ALL, including glucocorticoids, vincristine, and L-asparaginase, as well as more intensive and prolonged central nervous system (CNS) prophylaxis.11 Most of these children were treated in experienced pediatric cancer centers. Therefore, we performed a prospective US cooperative group trial, CALGB (Cancer and Leukemia Group B) 10403, to determine whether AYA patients with ALL could tolerate an intensive pediatric regimen and achieve improved survival rates when treated by adult hematologists/oncologists.
Methods
Patients
From November 2007 through September 2012, 318 AYAs (age 17-39 years) with newly diagnosed precursor B- or T-cell ALL (World Health Organization diagnostic criteria) were enrolled in CALGB 10403 from 3 US cooperative groups (CALGB, Eastern Cooperative Oncology Group [ECOG], SWOG). Patients were required to have ECOG performance status of 0 to 2. No prior treatment of ALL was allowed, with the exception of emergency treatment with corticosteroids or hydroxyurea for hyperleukocytosis, superior vena cava syndrome, or renal failure resulting from leukemic infiltration of the kidneys. A single dose of intrathecal chemotherapy was allowed before registration. Patients with a Burkitt immunophenotype were not eligible. Patients found to have Philadelphia chromosome–positive (Ph+) leukemia who enrolled were encouraged to receive alternative treatment that incorporated a tyrosine kinase inhibitor and were excluded from all analyses. Each participant signed an institutional review board–approved, protocol-specific informed consent document in accordance with federal and institutional guidelines.
Chemotherapy
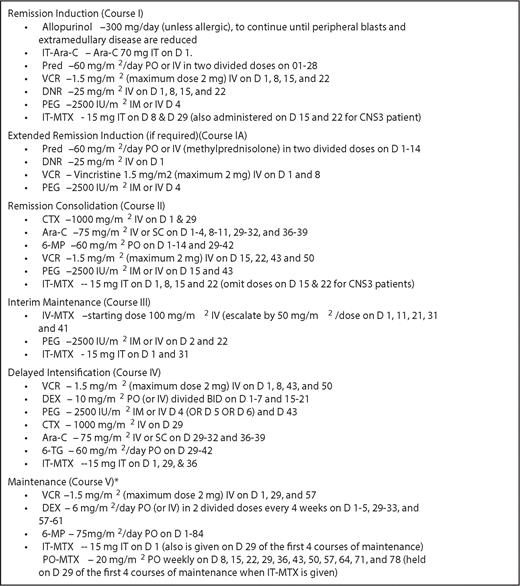
CALGB 10403 treatment consisted of induction, consolidation, interim maintenance, delayed intensification, and long-term maintenance therapy (detailed dosing schedule provided in Figure 1) and replicated exactly 1 arm of the Children's Oncology Group (COG) randomized study AALL0232 for high-risk childhood ALL.11
Treatment schema for CALGB 10403. *Maintenance therapy consisted of 12-week courses continuing until 3 years from initiation of interim maintenance for male and 2 years for female patients. Patients with precursor T-cell ALL received 24 Gy of prophylactic cranial irradiation during first cycle of maintenance therapy; those with CNS involvement at presentation received 18 Gy. 6-MP, 6-mercaptopurine; 6-TG, 6-thioguanine; Ara-C, cytarabine; CTX, cyclophosphamide; DEX, dexamethasone; DNR, daunorubicin; IT, intrathecally; MTX, methotrexate; PEG, pegylated asparaginase; PO, orally; pred, prednisone; VCR, vincristine.
Treatment schema for CALGB 10403. *Maintenance therapy consisted of 12-week courses continuing until 3 years from initiation of interim maintenance for male and 2 years for female patients. Patients with precursor T-cell ALL received 24 Gy of prophylactic cranial irradiation during first cycle of maintenance therapy; those with CNS involvement at presentation received 18 Gy. 6-MP, 6-mercaptopurine; 6-TG, 6-thioguanine; Ara-C, cytarabine; CTX, cyclophosphamide; DEX, dexamethasone; DNR, daunorubicin; IT, intrathecally; MTX, methotrexate; PEG, pegylated asparaginase; PO, orally; pred, prednisone; VCR, vincristine.
Statistical analysis
The primary end points of this study were induction response rate, event-free survival (EFS), disease-free survival (DFS), and OS for the overall populations and separately within precursor B- and T-cell subsets, with comparison of these outcomes with historical controls consisting of patients with newly diagnosed, non-Ph+ ALL age 16 to 29 years who were enrolled in previous CALGB trials and had median EFS of 30 months. Planned enrollment was 300 patients. Secondary end points included toxicities as well as impact of pretreatment patient characteristics on outcomes. Data were locked on 31 July 2018.
Bone marrow response was defined using the M bone marrow criteria for ALL; if M0 to M1 status (blast cells <5%) was achieved by the end of induction or extended induction, the patient was considered a responder. EFS was defined as time from registration in this study to the earliest occurrence of any of the following: failure to achieve bone marrow response by day 60, death, relapse at any site, or development of second malignant disease. DFS was considered the same as EFS except calculated from the date of bone marrow response. OS was defined from registration to death resulting from any cause. EFS, DFS, and OS were analyzed using Kaplan-Meier methods. Patients lost to follow-up were censored at the date last seen. Medians with their 95% confidence intervals (CIs) were used to compare patients in this trial with historical control estimates and between subgroups. The study was designed to test whether median EFS for patients in this trial was significantly better than 30 months. At least 126 EFS events were needed to test the null hypothesis that the true median EFS was 32 months against the alternative hypothesis that the true median EFS was 42 months, with a 1-sided type 1 error of 0.10 and power of 0.90.
Response rates were calculated with 95% CIs and were compared with historical controls using a 1-sample binomial test. Toxicities were summarized using Common Terminology Criteria for Adverse Events (version 3.0), and the maximum grade per patient of events at least possibly related to treatment was reported. All P values were based on 2-sided tests. Hazard ratios (HRs) and associated 95% CIs were reported.
To examine whether EFS, DFS, and OS are predicted by pretreatment characteristics such as age, sex, body mass index (BMI), ethnicity, immunophenotype, white blood cell (WBC) count, or cytogenetic or molecular genetic characteristics, log-rank tests were used for subgroup analyses, and Cox proportional hazards model was used to test univariable and multivariable associations. Patients were classified into cytogenetic risk groups according to the criteria we used for classification of patients who were treated in the CALGB 19802 study.6 Specifically, the unfavorable-risk category included patients who carried t(4;11)(q21;q23) or any other balanced translocation involving band 11q23, monosomy of chromosome 7 (−7), or trisomy of chromosome 8 (+8) and/or had hypodiploid karyotype defined as karyotype with chromosome number ≤43 with or without a near-triploid (ie, with near 69 chromosomes) clone (or had a near-triploid clone without a hypodiploid clone). The intermediate-risk category was defined by presence of either normal karyotype or structural abnormalities involving the short arm of chromosome 9 (9p), t(1;19)(q23;p13.3) or a derivative of chromosome 19 resulting from this reciprocal translocation [der(19)t(1;19)(q23;p13.3)], deletions of the long arm of chromosome 6 [del(6q)] and the long arm of chromosome 13 [del(13q)], trisomy of chromosome 21 (+21), and high hyperdiploidy defined as chromosome number ≥50 (excluding near triploidy and near tetraploidy). The favorable-risk category was defined by presence of abnormalities involving bands 14q11, 7p14∼15, or 7q34∼36 and deletions and translocations involving the short arm of chromosome 12 (12p). Patients who did not harbor any of the aforementioned chromosome abnormalities were prognostically unclassified. For quantitation of minimal residual disease (MRD), quantitative clone-specific polymerase chain reaction analyses for detection of clonal immunoglobulin heavy chain or T-cell receptor gene rearrangements were performed as previously described.12 For identification of Ph-like ALL signature, diagnostic marrow aspirates or blood cells were subjected to a validated Clinical Laboratory Improvement Amendments–approved low-density array as described previously.13 Because both MRD and Ph-like signature were analyzed in a subset of patients, comparison analyses were performed to assure that these patients were representative of the entire study population. For these analyses, there were no significant differences in presenting features between those available vs unavailable for Ph-like signature. There was a trend (P = .05) toward initial higher WBC counts among those available for end-of-induction MRD analysis compared with those not available.
Data collection and statistical analyses were conducted by the Alliance Statistics and Data Center. Data quality was ensured by review of data by the Alliance Statistics and Data Center and by the study chairperson following Alliance policies.
Results
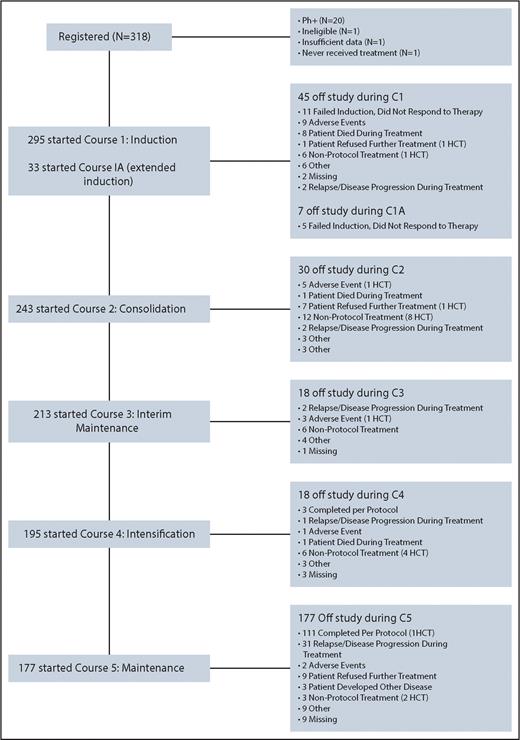
A total of 318 patients were registered (Figure 2). Twenty patients were found to have Ph+ ALL after registration and were excluded from all analyses. In addition, 1 ineligible patient with acute undifferentiated leukemia, 1 patient without BCR-ABL1 testing, and 1 patient who never received protocol treatment were excluded. Thus, 295 patients were analyzed.
This figure is a graphical representation of enrollment, treatment, and follow-up of the 318 patients registered to CALGB 10403.
This figure is a graphical representation of enrollment, treatment, and follow-up of the 318 patients registered to CALGB 10403.
Patient demographics and pretreatment characteristics are summarized in Table 1. Median age was 24 years; 25% of patients were 30 to 39 years old. Pretreatment samples were evaluable for Ph-like signature and CRLF2 expression in 131 of the 223 B-cell patients; 41 patients (31% of those tested) had Ph-like signature, and 28 (21% of those tested) had aberrant CRLF2 expression. Twenty-six patients were positive by both assays. Among the 223 B-cell ALL patients, 202 had CD20 expression on lymphoblasts, 65 had CD20 >20% or were strongly positive, 83 had CD20 <20%, and 51 had no CD20 expression.
Patient pretreatment characteristics
| Characteristic . | N (%) . |
|---|---|
| Total (N = 295) . | |
| Sex | |
| Male | 180 (61) |
| Female | 115 (39) |
| Race | |
| Unknown | 24 (8.1) |
| White | 220 (74.6) |
| Black/African American | 29 (9.8) |
| Asian | 9 (3.1) |
| Native Hawaiian or Pacific Islander | 2 (0.7) |
| Native American or Alaska native | 7 (2.4) |
| Not reported | 3 (1.0) |
| Multiple races reported | 1 (0.3) |
| Ethnicity | |
| Hispanic | 45 (15.3) |
| Non-Hispanic | 218 (73.9) |
| Not Reported | 4 (1.4) |
| Unknown | 28 (9.5) |
| Age at diagnosis, yr | |
| Median | 24.0 |
| Range | 17.0-39.0 |
| 16-20 | 74 (25.1) |
| 21-29 | 146 (49.5) |
| 30-39 | 75 (25.4) |
| BMI, kg/m2 | |
| Median | 26.5 |
| Range | 14.9-54.3 |
| <30 | 201 (68.1) |
| 30-40 | 72 (24.4) |
| >40 | 22 (7.5) |
| Performance status (ECOG) | |
| 0 | 116 (39.3) |
| 1 | 153 (51.9) |
| 2 | 26 (8.8) |
| Immunophenotype (n = 294) | |
| B cell | 223 (75.9) |
| T cell | 71 (24.1) |
| CNS extramedullary disease (n = 294) | |
| Involved | 31 (10.5) |
| Not involved | 255 (86.4) |
| Unknown | 8 (2.7) |
| Not done | 24 (8.2) |
| WBC, ×109/L (n = 292) | |
| Median | 9 |
| Range | 0.4-444.6 |
| ≤30 | 217 (74.3) |
| >30 | 75 (25.7) |
| Ph-like genetic profile (n = 131) | |
| Yes | 41 (31.3) |
| No | 90 (68.7) |
| Aberrant CRLF2 expression (n = 131) | |
| Yes | 28 (21.4) |
| No | 103 (78.6) |
| Cytogenetics6(n = 257) | |
| Favorable | 16 (6.2) |
| Intermediate | 112 (43.6) |
| Unfavorable | 18 (7.0) |
| Unclassified | 25 (9.8) |
| Not fully evaluable | 86 (33.5) |
| Characteristic . | N (%) . |
|---|---|
| Total (N = 295) . | |
| Sex | |
| Male | 180 (61) |
| Female | 115 (39) |
| Race | |
| Unknown | 24 (8.1) |
| White | 220 (74.6) |
| Black/African American | 29 (9.8) |
| Asian | 9 (3.1) |
| Native Hawaiian or Pacific Islander | 2 (0.7) |
| Native American or Alaska native | 7 (2.4) |
| Not reported | 3 (1.0) |
| Multiple races reported | 1 (0.3) |
| Ethnicity | |
| Hispanic | 45 (15.3) |
| Non-Hispanic | 218 (73.9) |
| Not Reported | 4 (1.4) |
| Unknown | 28 (9.5) |
| Age at diagnosis, yr | |
| Median | 24.0 |
| Range | 17.0-39.0 |
| 16-20 | 74 (25.1) |
| 21-29 | 146 (49.5) |
| 30-39 | 75 (25.4) |
| BMI, kg/m2 | |
| Median | 26.5 |
| Range | 14.9-54.3 |
| <30 | 201 (68.1) |
| 30-40 | 72 (24.4) |
| >40 | 22 (7.5) |
| Performance status (ECOG) | |
| 0 | 116 (39.3) |
| 1 | 153 (51.9) |
| 2 | 26 (8.8) |
| Immunophenotype (n = 294) | |
| B cell | 223 (75.9) |
| T cell | 71 (24.1) |
| CNS extramedullary disease (n = 294) | |
| Involved | 31 (10.5) |
| Not involved | 255 (86.4) |
| Unknown | 8 (2.7) |
| Not done | 24 (8.2) |
| WBC, ×109/L (n = 292) | |
| Median | 9 |
| Range | 0.4-444.6 |
| ≤30 | 217 (74.3) |
| >30 | 75 (25.7) |
| Ph-like genetic profile (n = 131) | |
| Yes | 41 (31.3) |
| No | 90 (68.7) |
| Aberrant CRLF2 expression (n = 131) | |
| Yes | 28 (21.4) |
| No | 103 (78.6) |
| Cytogenetics6(n = 257) | |
| Favorable | 16 (6.2) |
| Intermediate | 112 (43.6) |
| Unfavorable | 18 (7.0) |
| Unclassified | 25 (9.8) |
| Not fully evaluable | 86 (33.5) |
Remission induction
Two hundred sixty-three patients (89%) achieved complete bone marrow response at end of induction (n = 237) or after extended induction therapy (n = 26; Figure 1). There were 9 deaths (3%) during induction therapy. Of the induction deaths, 6 were treatment related (2 patients died as a result of sepsis, 2 because of hepatic failure, 1 as a result of ventricular arrhythmia, and 1 because of ventricular tachycardia). Of the 263 patients who achieved remission, 20 underwent allogeneic hematopoietic cell transplantation in first remission; 3 of these patients had t(4;11). The protocol recommended transplantation in first CR (CR1) for these patients; the rest underwent transplantation at the discretion of the treating physician/patient.
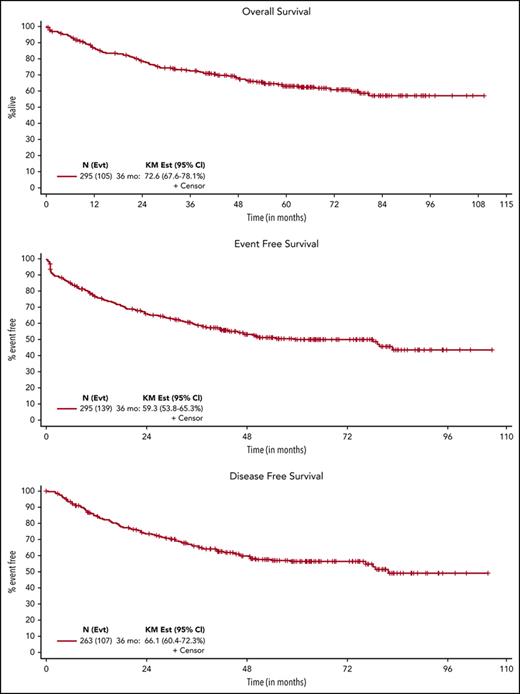
DFS, EFS, and OS
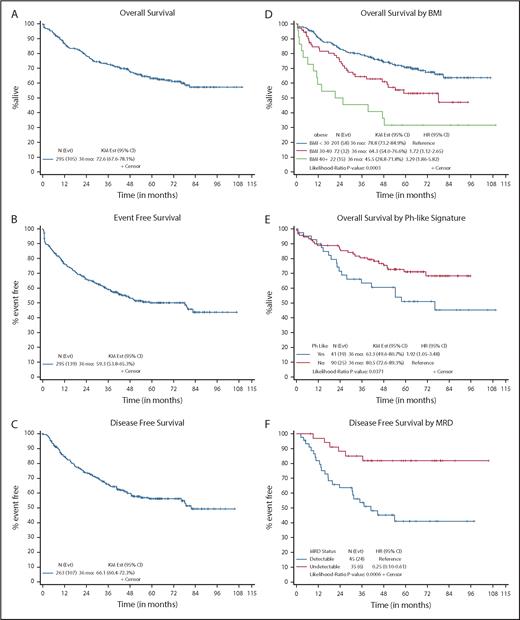
After median follow-up of 64 months for surviving patients, 190 (64%) were alive and 105 (36%) had died. Median OS was not reached. Estimated 3-year OS was 73% (95% CI, 68%-78%), compared with a historical rate of 58% (95% CI, 52%-64%) for CALGB patients age 16 to 29 years.2,6,14,15 Ninety patients relapsed, and 9 had progressive disease. Median EFS was 78.1 months (95% CI, 41.8 to not reached), more than double the historical control of 30 months (95% CI, 22-38 months); 3-year EFS was 59% (95% CI, 54%-65%). Among the 263 patients who achieved a bone marrow response, median DFS was 81.7 months (95% CI, 58.4 months to not reached), and 3-year DFS was 66% (95% CI, 60%-72%), both significantly higher than the historical control (median DFS, 34 months; 95% CI, 28-50 months; 3-year DFS, 48%; 95% CI, 41%-55%; Table 2; Figure 3A-C). Of the 20 patients who underwent allogeneic transplantation in CR1, 12 died. Median DFS for these patients was 36 months.
Outcomes
| . | Overall . | Historical controls . |
|---|---|---|
| Median (range) follow-up for surviving patients, mo | 64.2 (0.4-109.5) | |
| Induction death rate, N (%) | 9 (3) | |
| Response/progression | ||
| M status CR, N (%)* | 263 (89) | |
| 95% exact CI, % | 85-92 | |
| OS | ||
| N of patients | 295 | |
| N of events | 105 | |
| Median (95% CI), mo | NE | 61 (39-89) |
| 3 yr (95% CI), % | 73 (68-78) | 58 (52-64) |
| EFS | ||
| N of patients | 295 | |
| N of events | 139 | |
| Median (95% CI), mo | 78.1 (41.8-NE) | 30 (22-38) |
| 3 yr (95% CI), % | 59 (54-65) | |
| DFS | ||
| N of patients | 263 | |
| N of events | 107 | |
| Median (95% CI), mo | 81.7 (58.4-NE) | 34 (28-50) |
| 3 yr (95% CI), % | 66 (60-72) | 48 (41-55) |
| . | Overall . | Historical controls . |
|---|---|---|
| Median (range) follow-up for surviving patients, mo | 64.2 (0.4-109.5) | |
| Induction death rate, N (%) | 9 (3) | |
| Response/progression | ||
| M status CR, N (%)* | 263 (89) | |
| 95% exact CI, % | 85-92 | |
| OS | ||
| N of patients | 295 | |
| N of events | 105 | |
| Median (95% CI), mo | NE | 61 (39-89) |
| 3 yr (95% CI), % | 73 (68-78) | 58 (52-64) |
| EFS | ||
| N of patients | 295 | |
| N of events | 139 | |
| Median (95% CI), mo | 78.1 (41.8-NE) | 30 (22-38) |
| 3 yr (95% CI), % | 59 (54-65) | |
| DFS | ||
| N of patients | 263 | |
| N of events | 107 | |
| Median (95% CI), mo | 81.7 (58.4-NE) | 34 (28-50) |
| 3 yr (95% CI), % | 66 (60-72) | 48 (41-55) |
NE, not estimable.
Achieved M0 to M1 status by end of induction or extended induction.
Survival data. After median follow-up of 64 months for surviving patients, 190 (64%) were alive and 105 (36%) had died. (A) Median OS was not reached. Estimated 3-year OS was 73% (95% CI, 68%-78%). (B) Median EFS was 78.1 months (95% CI, 41.8 months to not reached), more than double the historical control of 30 months (95% CI, 22-38 months); 3-year EFS was 59% (95% CI, 54%-66%). (C) Median DFS was 81.7 months (95% CI, 58.4 months to not reached); 3-year DFS was 66% (95% CI, 60%-72%). (D) In comparison with patients with BMI <30 kg/m2, those with BMI between 30 and 40 kg/m2 and those with BMI >40 kg/m2 had significantly higher risk of death (HR, 1.72 and 3.29, respectively). Estimated 3-year survival for patients with BMI <30 kg/m2 was 79% (95% CI, 73%-85%); for those with BMI from 30 to 40 kg/m2, 3-year survival was 64% (95% CI, 54%-77%); and for those with BMI >40 kg/m2, 3-year survival was 46% (95% CI, 29%-72%; P = .0003). (E) Ph-like signature was associated with worse survival; 3-year OS rate was 63% (95% CI, 50%-81%) for patients with Ph-like signature, in contrast to 81% (95% CI, 73%-89%) for those without Ph-like signature. (F) Detection of MRD using quantitative polymerase chain reaction after induction therapy was strongly associated with worse DFS; 3-year DFS rate for those with undetectable MRD was 85% (95% CI, 74%-98%); in contrast, for those with detectable MRD, DFS was only 54% (95% CI, 41%-71%; P = .001). KM est, Kaplan-Meier estimate.
Survival data. After median follow-up of 64 months for surviving patients, 190 (64%) were alive and 105 (36%) had died. (A) Median OS was not reached. Estimated 3-year OS was 73% (95% CI, 68%-78%). (B) Median EFS was 78.1 months (95% CI, 41.8 months to not reached), more than double the historical control of 30 months (95% CI, 22-38 months); 3-year EFS was 59% (95% CI, 54%-66%). (C) Median DFS was 81.7 months (95% CI, 58.4 months to not reached); 3-year DFS was 66% (95% CI, 60%-72%). (D) In comparison with patients with BMI <30 kg/m2, those with BMI between 30 and 40 kg/m2 and those with BMI >40 kg/m2 had significantly higher risk of death (HR, 1.72 and 3.29, respectively). Estimated 3-year survival for patients with BMI <30 kg/m2 was 79% (95% CI, 73%-85%); for those with BMI from 30 to 40 kg/m2, 3-year survival was 64% (95% CI, 54%-77%); and for those with BMI >40 kg/m2, 3-year survival was 46% (95% CI, 29%-72%; P = .0003). (E) Ph-like signature was associated with worse survival; 3-year OS rate was 63% (95% CI, 50%-81%) for patients with Ph-like signature, in contrast to 81% (95% CI, 73%-89%) for those without Ph-like signature. (F) Detection of MRD using quantitative polymerase chain reaction after induction therapy was strongly associated with worse DFS; 3-year DFS rate for those with undetectable MRD was 85% (95% CI, 74%-98%); in contrast, for those with detectable MRD, DFS was only 54% (95% CI, 41%-71%; P = .001). KM est, Kaplan-Meier estimate.
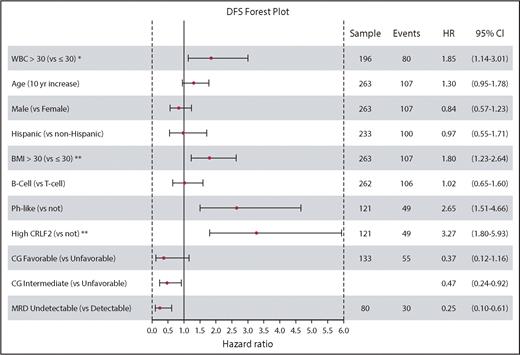
Patient pretreatment characteristics were examined for their impact on treatment outcomes (Figure 4). In univariable models, initial WBC count >30 × 109/L for patients with precursor B-cell ALL, obesity (BMI >30 kg/m2), presence of Ph-like signature, and aberrant CRLF2 expression (present in 68% of Ph-like subset) were strongly associated with worse EFS, DFS, and OS (Figure 3D-E). There were no significant differences in EFS, DFS, or OS between patients with B-cell vs T-cell phenotype or by age subgroup (supplemental Figures 1 and 2, available on the Blood Web site). Although there was a trend toward improved outcomes for the youngest patients (age 16-20 years), the differences were not significant, and outcomes for patients age 20 to 29 and 30 to 39 years were nearly identical. In comparison with patients with unfavorable cytogenetic risk, patients with intermediate-risk cytogenetics had significantly better DFS (HR, 0.47; P = .027), and patients with favorable-risk cytogenetics had even better DFS, although this was not statistically significant, probably because of the limited sample size in the favorable group (HR, 0.37; P = .087). EFS and OS were similar between cytogenetic subsets. Expression of CD20 did not correlate with EFS, DFS, or OS (supplemental Figure 3). An initial elevated WBC was associated with worse EFS (HR, 1.63; P = .03) and DFS (HR, 1.85; P = .02) among B-cell patients only. In multivariable analysis, only obesity (HR, 1.82; P = .04) and aberrant CRLF2 expression (HR, 2.84; P < .001) were associated with significantly worse DFS. In multivariable analysis, none of the pretreatment characteristics achieved statistical significance for EFS or OS.
Forest plot for univariable model of DFS. Impact of pretreatment characteristics on DFS is shown. HR is depicted on the x-axis, and each prognostic variable is listed on the y-axis. Estimates to the right of 1.0 indicate worse DFS. Measurement for initial WBC was found to be prognostic for DFS only in B-cell ALL patients. For multivariable models, variables with P < .2 from the univariable models were included; only obesity (BMI >30 kg/m2; HR, 1.82; P = .04) and aberrant CRLF2 expression (HR, 2.84; P < .001) were associated with significantly worse DFS. CG, cytogenetics.
Forest plot for univariable model of DFS. Impact of pretreatment characteristics on DFS is shown. HR is depicted on the x-axis, and each prognostic variable is listed on the y-axis. Estimates to the right of 1.0 indicate worse DFS. Measurement for initial WBC was found to be prognostic for DFS only in B-cell ALL patients. For multivariable models, variables with P < .2 from the univariable models were included; only obesity (BMI >30 kg/m2; HR, 1.82; P = .04) and aberrant CRLF2 expression (HR, 2.84; P < .001) were associated with significantly worse DFS. CG, cytogenetics.
MRD
Serial samples for MRD evaluation were available for 80 patients. Thirty-five patients (44%) achieved undetectable MRD status at the end of induction, and 3 additional patients achieved low MRD (<10−4). Three-year DFS was significantly better for those who achieved MRD negativity (undetectable) at 85% (95% CI, 74%-98%), compared with those with detectable MRD (>10−4) at 54% (95% CI, 41%-71%; P = .001; Figure 3F). DFS HR for those achieving MRD negativity (undetectable) was 0.25 (95% CI, 0.10-0.60). Patients achieving low MRD (<10−4) had similarly excellent DFS. Of those who had undetectable MRD, 2 (11%) of 19 had Ph-like signature, compared with 17 (46%) of 35 without (Fisher's exact P = .02).
Toxicities
There were a total of 8 (3%) treatment-related deaths, 6 of which occurred during the induction course. During induction therapy, grade 3 to 4 nonhematological toxicities, which occurred in >10% of patients, included hypofibrinogenemia (42%) with 1 serious hemorrhage (in the CNS), elevated transaminases (28%), elevated bilirubin (18%), hyperglycemia (30%), febrile neutropenia (22%), and documented infections (18%; Table 3). Fifteen patients (5%) had a thrombotic event; half of these were related to a venous catheter device. Frequency of events decreased markedly during postremission treatment. Overall, 29 patients (10%) had grade 3 to 4 hypersensitivity reactions to pegylated asparaginase throughout protocol treatment. Occurrence of these events decreased to 4% after an amendment that mandated premedication with acetaminophen, hydrocortisone, and diphenhydramine before each dose of pegylated asparaginase. Thirty-three patients (11%) developed grade 3 to 4 hypertriglyceridemia, but these were mostly asymptomatic; grade 3 to 4 pancreatitis occurred in 14 patients (5%). Grade 3 to 4 sensory or motor neuropathy occurred in 45 (16%) and 17 patients (6%), respectively; grade 3 to 4 osteonecrosis was reported in 11 patients (4%); grade 3 to 4 mucositis occurred in 19 (6%) patients, primarily during interim maintenance treatment. Four second malignancies (all myeloid neoplasms) were reported.
Maximum severity of select grade 3+ adverse events
| Adverse event* . | N (%) . | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Induction (n = 295) . | Postremission consolidation therapy† (n = 237) . | Maintenance (n = 173) . | Overall (n = 295) . | |||||||||
| Grade 3 . | Grade 4 . | Grade 5 . | Grade 3 . | Grade 4 . | Grade 5 . | Grade 3 . | Grade 4 . | Grade 5 . | Grade 3 . | Grade 4 . | Grade 5 . | |
| Allergic reaction/hypersensitivity | 2 (1) | 0 | 0 | 17 (7) | 10 (4) | 0 | 0 | 0 | 0 | 19 (7) | 10 (3) | 0 |
| ALT | 72 (26) | 7 (3) | 0 | 93 (39) | 6 (3) | 0 | 69 (40) | 2 (1) | 0 | 145 (50) | 13 (4) | 0 |
| AST | 31 (11) | 4 (1) | 0 | 55 (23) | 4 (2) | 0 | 26 (15) | 1 (1) | 0 | 89 (31) | 9 (3) | 0 |
| Bilirubin (hyperbilirubinemia) | 34 (12) | 17 (6) | 0 | 19 (8) | 4 (2) | 0 | 16 (9) | 1 (1) | 0 | 56 (19) | 21 (7) | 0 |
| Death NOS | 0 | 0 | 1 (<1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 (<1) |
| Fatigue | 14 (5) | 2 (1) | 0 | 29 (12) | 0 | 0 | 6 (3) | 0 | 0 | 38 (13) | 2 (1) | 0 |
| Febrile neutropenia | 53 (19) | 8 (3) | 0 | 93 (39) | 13 (5) | 0 | 25 (15) | 4 (2) | 0 | 128 (44) | 24 (8) | 0 |
| Glucose serum high (hyperglycemia) | 63 (23) | 22 (8) | 0 | 19 (8) | 7 (3) | 0 | 19 (11) | 2 (1) | 0 | 73 (25) | 30 (10) | 0 |
| Hemorrhage CNS | 1 (<1) | 2 (1) | 0 | 0 (0) | 0 | 0 | 1 (1) | 0 | 0 | 2 (1) | 2 (1) | 0 |
| Infection | 36 (13) | 15 (5) | 2 (1) | 53 (22) | 6 (3) | 2 (1) | 24 (14) | 3 (2) | 0 | 60 (21) | 14 (5) | 4 (1) |
| Liver dysfunction/failure | 2 (1) | 1 (<1) | 2 (1) | 0 | 0 | 0 | 0 | 0 | 0 | 2 (1) | 1 (<1) | 2 (1) |
| Mucositis/stomatitis/esophagitis | 4 (1) | 1 (<1) | 0 | 19 (8) | 3 (1) | 0 | 4 (2) | 1 (1) | 0 | 14 (5) | 4 (1) | 0 |
| Neuropathy: motor | 3 (1) | 2 (1) | 0 | 10 (4) | 1 (0) | 0 | 4 (2) | 0 | 0 | 15 (5) | 2 (1) | 0 |
| Neuropathy: sensory | 5 (2) | 2 (1) | 0 | 36 (15) | 1 (0) | 0 | 16 (9) | 0 | 0 | 42 (15) | 3 (1) | 0 |
| Osteonecrosis (avascular necrosis) | 1 (<1) | 0 | 0 | 1 (<1) | 0 | 0 | 10 (6) | 1 (1) | 0 | 11 (4) | 1 (0) | 0 |
| Pancreatitis | 2 (1) | 2 (1) | 0 | 10 (4) | 0 | 0 | 1 (1) | 0 | 0 | 12 (4) | 2 (1) | 0 |
| Thrombosis/thrombus/embolism | 8 (3) | 7 (3) | 0 | 14 (6) | 7 (3) | 0 | 0) | 1 (1) | 0 | 20 (7) | 13 () | 0 |
| Triglyceride serum high (hypertriglyceridemia) | 4 (1) | 4 (1) | 0 | 8 (3) | 21 (9) | 0 | 2 (1) | 1 (1) | 0 | 10 (3) | 23 (8) | 0 |
| Tumor lysis syndrome | 15 (5) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 15 (5) | 0 | 0 |
| Ventricular arrhythmia | 0 | 1 (<1) | 1 (<1) | 0 | 0 | 0 | 1 (<1) | 0 | 0 | 1 (0) | 1 (0) | 1 (<1) |
| Adverse event* . | N (%) . | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Induction (n = 295) . | Postremission consolidation therapy† (n = 237) . | Maintenance (n = 173) . | Overall (n = 295) . | |||||||||
| Grade 3 . | Grade 4 . | Grade 5 . | Grade 3 . | Grade 4 . | Grade 5 . | Grade 3 . | Grade 4 . | Grade 5 . | Grade 3 . | Grade 4 . | Grade 5 . | |
| Allergic reaction/hypersensitivity | 2 (1) | 0 | 0 | 17 (7) | 10 (4) | 0 | 0 | 0 | 0 | 19 (7) | 10 (3) | 0 |
| ALT | 72 (26) | 7 (3) | 0 | 93 (39) | 6 (3) | 0 | 69 (40) | 2 (1) | 0 | 145 (50) | 13 (4) | 0 |
| AST | 31 (11) | 4 (1) | 0 | 55 (23) | 4 (2) | 0 | 26 (15) | 1 (1) | 0 | 89 (31) | 9 (3) | 0 |
| Bilirubin (hyperbilirubinemia) | 34 (12) | 17 (6) | 0 | 19 (8) | 4 (2) | 0 | 16 (9) | 1 (1) | 0 | 56 (19) | 21 (7) | 0 |
| Death NOS | 0 | 0 | 1 (<1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 (<1) |
| Fatigue | 14 (5) | 2 (1) | 0 | 29 (12) | 0 | 0 | 6 (3) | 0 | 0 | 38 (13) | 2 (1) | 0 |
| Febrile neutropenia | 53 (19) | 8 (3) | 0 | 93 (39) | 13 (5) | 0 | 25 (15) | 4 (2) | 0 | 128 (44) | 24 (8) | 0 |
| Glucose serum high (hyperglycemia) | 63 (23) | 22 (8) | 0 | 19 (8) | 7 (3) | 0 | 19 (11) | 2 (1) | 0 | 73 (25) | 30 (10) | 0 |
| Hemorrhage CNS | 1 (<1) | 2 (1) | 0 | 0 (0) | 0 | 0 | 1 (1) | 0 | 0 | 2 (1) | 2 (1) | 0 |
| Infection | 36 (13) | 15 (5) | 2 (1) | 53 (22) | 6 (3) | 2 (1) | 24 (14) | 3 (2) | 0 | 60 (21) | 14 (5) | 4 (1) |
| Liver dysfunction/failure | 2 (1) | 1 (<1) | 2 (1) | 0 | 0 | 0 | 0 | 0 | 0 | 2 (1) | 1 (<1) | 2 (1) |
| Mucositis/stomatitis/esophagitis | 4 (1) | 1 (<1) | 0 | 19 (8) | 3 (1) | 0 | 4 (2) | 1 (1) | 0 | 14 (5) | 4 (1) | 0 |
| Neuropathy: motor | 3 (1) | 2 (1) | 0 | 10 (4) | 1 (0) | 0 | 4 (2) | 0 | 0 | 15 (5) | 2 (1) | 0 |
| Neuropathy: sensory | 5 (2) | 2 (1) | 0 | 36 (15) | 1 (0) | 0 | 16 (9) | 0 | 0 | 42 (15) | 3 (1) | 0 |
| Osteonecrosis (avascular necrosis) | 1 (<1) | 0 | 0 | 1 (<1) | 0 | 0 | 10 (6) | 1 (1) | 0 | 11 (4) | 1 (0) | 0 |
| Pancreatitis | 2 (1) | 2 (1) | 0 | 10 (4) | 0 | 0 | 1 (1) | 0 | 0 | 12 (4) | 2 (1) | 0 |
| Thrombosis/thrombus/embolism | 8 (3) | 7 (3) | 0 | 14 (6) | 7 (3) | 0 | 0) | 1 (1) | 0 | 20 (7) | 13 () | 0 |
| Triglyceride serum high (hypertriglyceridemia) | 4 (1) | 4 (1) | 0 | 8 (3) | 21 (9) | 0 | 2 (1) | 1 (1) | 0 | 10 (3) | 23 (8) | 0 |
| Tumor lysis syndrome | 15 (5) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 15 (5) | 0 | 0 |
| Ventricular arrhythmia | 0 | 1 (<1) | 1 (<1) | 0 | 0 | 0 | 1 (<1) | 0 | 0 | 1 (0) | 1 (0) | 1 (<1) |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; NOS, not otherwise specified.
At least possibly related, per National Cancer Institute Common Terminology Criteria for Adverse Events (version 3.0); overall, 289 patients were evaluated for adverse events: 284 during induction, 232 during consolidation, 192 during interim maintenance, 184 during delayed intensification, and 173 during maintenance.
Consolidation, interim maintenance, and delayed intensification.
Outcomes after relapse
Limited data were available on subsequent therapies for the 90 patients who relapsed during or after CALGB 10403 treatment, because detailed follow-up was not required. Of the patients who relapsed, 22 were alive and 68 had died, with median survival after relapse of 10 months (95% CI, 7.0-14 months). For relapsed patients, 3-year rate of survival was 23% (95% CI, 15.2%-35%; supplemental Figure 4). Significant predictors of poor outcome after relapse included BMI >30 kg/m2 and T-cell immunophenotype.
Discussion
In CALGB 10403, a large prospective clinical trial performed by the 3 National Cancer Institute–sponsored cooperative groups in North America (Alliance, SWOG, and ECOG), we demonstrated that it is feasible to treat AYAs up to the age of 40 years with an intensive pediatric regimen, identical to that developed by COG, with low treatment-related mortality and marked improvement in outcomes. OS at 3 years was 73%, compared with earlier CALGB studies, where OS for this age group was 55% at 3 years. These results provide prospective evidence from a large multicenter study that more extensive use of glucocorticoids, vincristine, and pegylated asparaginase with intensive and prolonged CNS prophylaxis results in survival benefit for AYA patients with ALL.
Overall treatment-related mortality of 3% in CALGB 10403 was low and similar to rates reported in pediatric trials of ALL. However, there was higher incidence of hepatic and thrombotic complications during induction therapy compared with that previously reported in younger patients with ALL enrolled in the AALL0232 study.11 Obesity was a risk factor for worse outcomes in our study; nearly one-third of the enrolled patients had a BMI ≥30 kg/m2. Obesity was previously linked to worse outcomes in a retrospective analysis of children with ALL.16 The reasons for these poor outcomes in obese patients may be multifactorial, including some evidence that adipocytes attract leukemia cells and may shelter lymphoblasts during chemotherapy, leading to resistance; inadequate or, alternatively, excessive drug exposure; or other aspects of disease biology.17-20 As noted, obesity also predicted for worse survival after relapse. Hepatic, hyperglycemic, and thrombotic toxicities occurred more frequently during induction therapy in CALGB 10403, when the combination of high initial leukemia burden and obesity may have heightened proinflammatory and procoagulant states.21,22 In contrast, we found that treatment toxicities during postremission cycles in our AYA population were similar to those reported for adolescents treated in the pediatric AALL0232 study.11
CALGB 10403 survival rates were similar to those in other recently published studies23-28 that also employed intensified pediatric-inspired regimens for adults with ALL; of these, only our study focused exclusively on the AYA population as defined by the National Cancer Institute and included patients up to the age of 40 years. We faithfully replicated a regimen identical to that employed by the counterpart pediatric group, in our case COG AALL0232, which focused on intensive induction, postremission therapy, and long-term maintenance without recommendation for allogeneic transplantation in first remission, with the exception of a few high-risk subsets. The arm of the randomized AALL0232 trial that was replicated in CALGB 10403 was the treatment arm that employed interim maintenance with escalating doses of methotrexate (without leucovorin rescue) followed by asparaginase (Capizzi methotrexate) and not the alternative experimental arm of that study, which employed high-dose methotrexate with leucovorin rescue.11 Although COG AALL0232 data showed improved overall outcomes for patients with precursor B-cell ALL who received high-dose methotrexate, in subset analyses of this reported regimen, there was not a statistically significant improvement with this approach in the oldest group of patients enrolled in that study, who were age 20 to 30 years. In addition, in the recent report on the COG AALL0434 regimen for patients with precursor T-cell ALL that included patients up to age 30 years, the Capizzi methotrexate arm had significantly improved outcomes compared with the arm receiving high-dose methotrexate interim maintenance.11 CALGB 10403 included patients with both precursor B- and T-cell ALL.
Up to what age can an intensive pediatric regimen be safely administered? The upper age limit in all of these studies varied (from 40-59 years), but in both the Dana-Farber Cancer Institute28 and GRAALL-200524 studies, concerns were raised about an increase in chemotherapy-related toxicity; in the Dana-Farber Cancer Institute study, asparaginase-related toxicities occurred more frequently in patients older than age 45 to 50 years, and there was an inability to comply with treatment in the GRALL-2005 study for patients age >55 years, resulting in significantly worse treatment outcomes for these older patients. In contrast, the recently published Nordic Society of Paediatric Hematology and Oncology ALL2008 study, a single biologically risk-stratified protocol treatment was successfully administered to all patients with both B- and T-cell ALL from age 1 to 45 years.27 In this study, 221 of the 1022 patients were between the ages of 18 and 45 years; despite an increased risk of thrombosis, pancreatitis, and osteonecrosis in this older age group, treatment was feasible, and 5-year EFS was 74% ± 4% in this age subset. Although all of these studies vary in the pediatric backbone that was tested, it seems that the upper age limit for tolerability of an intensive pediatric regimen is between 45 and 55 years.
A number of disease-related factors also affected treatment outcomes. The common occurrence (31%) of the recently described Ph-like subset in our CALGB 10403 population emerged as an important predictor of adverse outcome.29-31 Frequency of Ph-like fusions, particularly those resulting in JAK pathway activation, increases in late adolescence and occurs in 25% to 35% of adults with ALL, with a higher frequency reported among Hispanic patients in the United States.32,33 Indeed, in our study, 31% of evaluable patients tested had Ph-like fusion, and these patients had significantly worse outcomes, with estimated 3-year EFS of only 42% (95% CI, 29%-61%), in contrast to 69% (95% CI, 60%-80%) for those without these fusions (HR, 2.06; log-rank P = .008). As has been previously described, a majority of patients with Ph-like ALL in CALGB 10403 had aberrant CRLF2 expression, resulting in activation of the JAK-STAT pathway, and particularly poor outcomes, with nearly a threefold increased risk of death (HR, 2.97; P = .001).32,33 The high frequency of CRLF2 overexpression in AYA ALL highlights important biological differences in precursor B-cell ALL between children and AYAs with ALL and helps to explain, in part, the worse treatment outcomes for AYA patients. Furthermore, specific identification of the signaling pathways activated by these novel gene fusions provides a direction for therapeutic targeting with directed kinase inhibitors or novel immunotherapeutic approaches. Interestingly, unlike other studies of adult ALL, where CD20 expression has been associated with inferior survival, we found equivalent EFS, DFS, and OS for all patients, regardless of CD20 expression levels.34
As in other studies of pediatric and adult ALL, detection of MRD after induction chemotherapy in CALGB 10403 seemed to be the most important predictor of DFS and OS. In the subset of patients with samples available and evaluable for MRD measurement, 44% had absence of detectable disease using a DNA-based polymerase chain reaction method with a sensitivity of detection of 1 in 104 to 105 after 4 weeks of treatment. These patients had excellent 3-year DFS of 85% (95% CI, 74%-98%). In contrast, 3-year DFS was only 54% (95% CI, 41%-71%) for those with detectable MRD (P = .001). Presence of MRD after induction therapy and its persistence after 10 to 16 weeks of treatment in many pediatric and adult studies have become validated predictors of outcome and may help to identify patients who need alternative therapy or who may benefit from undergoing allogeneic hematopoietic cell transplantation in CR1.35 Only 44% of our patients became MRD negative after induction, a rate lower than that typically reported in pediatric studies, where a large majority of patients have undetectable MRD after induction. This difference in end-of-induction MRD likely highlights the higher-risk, more resistant disease biology present in the AYA population, including a much higher incidence of Ph-like signature, and emphasizes the need to consider the addition of new agents that might overcome treatment resistance. In contrast to the design of many adult ALL studies, early allogeneic transplantation was not a goal of our trial. Only 20 patients enrolled in CALGB 10403 underwent allogeneic transplantation in CR1, and this was usually undertaken because of high-risk cytogenetics, such as t(4;11)(q21;q23), as specified by the protocol. Median 3-year DFS and OS for these patients was 50 months. A recent retrospective comparative analysis found that use of a pediatric-based treatment regimen for younger adults age 18 to 50 years afforded significantly improved survival compared with allogeneic transplantation in first remission.36 However, no attempts were made to adapt treatment based on risk, and no MRD assessments were available in either cohort of that study. In a recent analysis from French investigators, allogeneic transplantation in CR1 provided a survival benefit only for patients with persistence of MRD at levels of ≥10−3 after induction therapy; in contrast, there was no transplantation survival benefit for patients with very low or undetectable MRD.37 Because excellent survival rates are observed in patients who achieve early MRD-negative status, 1 goal of future trials in AYA ALL will be to add novel agents (eg, targeted antibodies) to an intensive pediatric chemotherapy backbone to increase the percentage of patients who achieve early MRD negativity. This is now being evaluated with inotuzumab ozogamicin added to the CALGB 10403 backbone in Alliance trial A041501.
In conclusion, significant improvements in survival of AYA patients with ALL have been achieved with use of a pediatric regimen administered by adult cooperative group medical teams in North America. Recently published data suggest that improved outcomes in AYA ALL require a high level of familiarity with and expertise in these intensive regimens by treatment centers.7,38 During the conduct of CALGB 10403, cooperative group investigators participated in ongoing twice monthly calls to provide educational support, discuss toxicity management, and optimize compliance.
Taken together, these results support the use of an intensive pediatric approach as a standard of care for AYAs with ALL and as the platform for future therapeutic development. The recent demonstration of improvements in survival with the addition of the anti-CD20 monoclonal antibody rituximab to intensive chemotherapy regimens in adult ALL39,40 and the development of highly active new antibody conjugates, bispecific antibodies, and genetically engineered T cells that recognize ALL epitopes provide an exciting opportunity to improve outcomes further for these patients.41-43 The next generation of studies in AYAs with ALL will determine whether novel immunotherapies and/or targeted kinase inhibitors for patients with Ph-like ALL can be safely added to this pediatric regimen to overcome treatment resistance, eradicate MRD, and further improve survival.
Acknowledgments
The authors acknowledge Michael Kelly, director of protocol operations for the Alliance for Clinical Trials, for his outstanding contributions to protocol coordination and CALGB 10403 trial conduct. The authors thank the following institutional networks for participation in this study: Dartmouth College Norris Cotton Cancer Center Lead Academic Participating Site (LAPS), Delaware/Christiana Care National Cancer Institute Community Oncology Research Program (NCORP), Mount Sinai Hospital, NCORP of the Carolinas (Greenville Health System NCORP), Northwell Health NCORP, The Ohio State University Comprehensive Cancer Center LAPS, Roswell Park Cancer Institute LAPS, University of California San Diego Moores Cancer Center, University of North Carolina Lineberger Comprehensive Cancer Center LAPS, University of Chicago Comprehensive Cancer Center LAPS, University of Iowa/Holden Comprehensive Cancer Center, University of Maryland/Greenebaum Cancer Center, University of Missouri Ellis Fischel Cancer Center, University of Vermont College of Medicine, Virginia Commonwealth University, Massey Cancer Center Minority Underserved NCORP, Wake Forest University Health Sciences, Washington University Siteman Cancer Center LAPS, Weill Medical College of Cornell University, East Carolina University, North Shore University Hospital, Long Island Jewish Medical Center, Naval Medical Center-San Diego, University of Minnesota Medical Center-Fairview, Christiana Care Health System-Christiana Hospital, University of North Carolina at Chapel Hill, Greenville Health System Cancer Institute/Greenville CCOP, Fort Wayne Medical Oncology and Hematology Inc-State Boulevard, Genesys Regional Medical Center-West Flint Campus, University of California Irvine, Loyola/Hines VA-UCOP, University of Utah–UCOP, City of Hope Med Center, Stanford University, University of Kentucky, Wayne State University, University of New Mexico, Cleveland Clinic, Cleveland Clin-UCOP, University of Kansas, Wichita CCOP, University of Michigan, Wesley Medical Center, University of Washington, Karmanos Cancer Institute, University of Rochester, Medical University of South Carolina, Thomas Jefferson University, Johns Hopkins University, Mayo Clinic, Geisinger Medical Center, Scottsdale CCOP, University of Pennsylvania, Northwestern University, Regions Hospital, McFarland Clinic, Medical College of Wisconsin, Rush Presby St Luke's Med Center, Penrose-St Francis HealthCare, Columbia-Presby-St Luke's Hospital, Aurora Presbyterian Hospital, Penn State Geisinger Cancer Center, St Rita's Medical Center, Inst. De Enfermedades Neoplasicas, University of Texas Southwestern Medical Center, Jewish Hospital, Mayo Clinic-Scottsdale-Phoenix, Penn State Cancer Institute, Avera Cancer Institute, John H. Stroger Hospital of Cook County, and Rocky Mountain Cancer Centers-Littleton.
This work was supported by the National Cancer Institute of the National Institutes of Health under awards U10CA180821 and U10CA180882 (to the Alliance for Clinical Trials in Oncology), P30CA033572, U10CA180790, U10CA180791, U10CA180820, U10CA180836, U10CA180838, U10CA180850, U10CA180867, U10CA180888, and U10CA189859 and in part by funds from Leadiant Biosciences, Inc.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Authorship
Contribution: W.S. designed the study, led the study, conducted correlative analysis (minimal residual disease [MRD]), analyzed the data, and wrote the manuscript; S.M.L. and A.S.A. were study principal investigators, analyzed data, and edited the manuscript; J.Y. and K.M.L. analyzed the data, created the study report, and edited the manuscript; R.C.H., C.G.M., C.L.W., N.F., G. Malnassy, and E. Paietta provided correlative study analysis (Philadelphia-like signature and MRD analysis) and edited the manuscript; K.M.L., S.G., and B.S. provided the statistical design and edited the manuscript; E. Parker coordinated the study; K.M. and C.D.B. analyzed the cytogenetics and edited the manuscript; G. Marcucci, M.L., D.F.C., M.C.F., F.R.A., H.E., M.R.L., M.S.T., and R.M.S. conducted the study and edited the manuscript; J.A.B. and J.C.G. contributed to the design of the study and edited the manuscript; and R.A.L. designed the study and edited the manuscript.
Conflict-of-interest disclosure: W.S. served on advisory boards for Pfizer, Amgen, and Jazz Pharmaceuticals; S.M.L. received clinical trial support from Onconova, Celgene, Cyclacel, Hoffman-La Roche, Onconova, Incyte, Biosight, and Kura and served on an advisory board for Pfizer; A.S.A. received honoraria from Pfizer, Sigma Tau, and Jazz Pharmaceuticals; C.G.M. received honoraria from Amgen and Pfizer; E. Parker owns stock in Teva Pharmaceuticals and Johnson & Johnson; M.S.T. received research funding from AbbVie, AROG, Cellerant, Orsenix, ADC Therapeutics, and Biosight and served on advisory boards for Daiicho-Sankyo, Orsenix, KAHR, Rigel, Abbvie, and Nohla. The remaining authors declare no competing financial interests.
Wendy Stock, University of Chicago Medicine and University of Chicago Comprehensive Cancer Center, Knapp Center for Biological Discovery, Room 8112, 900 E 57th St, Chicago, IL 60637; email: wstock@medicine.bsd.uchicago.edu.
REFERENCES
Author notes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Dombret

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal