TO THE EDITOR:
Treatment of splenic marginal zone lymphoma (SMZL) is not standardized due to the lack of prospective randomized trials.1-13 After our initial 2007 paper, we now present updated data on the activity of rituximab as first-line treatment in a much larger series of SMZL patients (n = 108) with a longer follow-up.7 Diagnosis was established according to the World Health Organization and the Splenic Lymphoma Study Group (SLSG) consensus criteria.14,15 The study was approved by the appropriate institutional review boards. The simplified prognostic score as proposed by the SLSG was calculated at the time of diagnosis and before treatment initiation.16-18 Criteria for rituximab initiation were bulky/symptomatic splenomegaly, cytopenias, B symptoms, and autoimmune manifestations. Treatment included an induction phase consisting of 6 weekly rituximab infusions (375 mg/m2). Responding patients either received rituximab maintenance every 2 months for 1 to 2 years or were followed up. Maintenance therapy was decided upon the practice of the treating physician within the 3 participating centers. Response assessment was scheduled at 2 months after the end of induction and was based on the SLSG consensus criteria.15 In addition, the term unconfirmed complete response (CRu) was used to describe a complete response (CR) but without bone marrow reevaluation.
Freedom from progression (FFP) was defined as the time between rituximab initiation and disease progression. Deaths in remission due to unrelated causes were censored. Overall survival (OS) was defined as the time between rituximab initiation and death of any cause. Lymphoma-specific survival (LSS) was defined as the time between rituximab initiation and disease-related death. Maintenance vs no maintenance comparison was restricted to rituximab induction responders.
Patients’ characteristics at diagnosis are provided in Table 1. Briefly, the median age was 65 years (41-91); 48% were men, and the median spleen size was 20 cm (16-25 cm). Six percent had B symptoms; 30% had anemia; and 17% had thrombocytopenia, whereas 43% had elevated LDH. The median time from diagnosis to treatment initiation was 2 months (range, 0-203). The vast majority of the patients (92/108, 85%) fulfilled the criteria for treatment initiation (cytopenias [n = 64], splenomegaly-related symptoms [n = 22], B symptoms [n = 3], autoimmune hemolytic anemia (AIHA) [n = 1], pleural effusion [n = 1], rapid increase in lymphocyte counts [n = 1]). In 16 patients (15%), treatment was administered based on their preference after detailed discussion.
Comparison of patients' characteristics and response to rituximab induction among all patients (n = 108), between those who received maintenance or not (n = 98), and between 1-y or 2-y maintenance (n = 75)
| . | . | No maintenance* . | Maintenance* . | . | Maintenance, 1 y† . | Maintenance, 2 y† . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient characteristics . | All patients, no. (%) . | No. . | % . | No. . | % . | P . | No.† . | % . | No.† . | % . | P . |
| Age, median (range), y | 65 (41-91) | ||||||||||
| Age (≥70 y) | 38/108 (35) | 11/22 | 50 | 24/76 | 32 | .11 | 17/48 | 35 | 7/27 | 26 | .40 |
| Sex (male) | 52/108 (48) | 11/22 | 50 | 36/76 | 47 | .83 | 22/48 | 46 | 13/27 | 48 | .85 |
| B symptoms (yes) | 7/108 (6) | 1/22 | 5 | 5/76 | 7 | .73 | 4/48 | 8 | 1/27 | 4 | .44 |
| LDH (elevated) | 45/106 (43) | 12/22 | 55 | 30/74 | 41 | .25 | 24/47 | 51 | 6/26 | 23 | .02 |
| Hemoglobin (<10 g/dL) | 32/100 (30) | 10/22 | 46 | 21/75 | 28 | .12 | 13/47 | 28 | 8/27 | 30 | .46 |
| Thrombocytopenia (<100 × 109/L) | 18/104 (17) | 6/22 | 27 | 10/75 | 13 | .12 | 3/47 | 6 | 7/27 | 26 | .018 |
| Lymphocytes (≥4 × 109/L) | 45/104 (43) | 7/20 | 35 | 33/75 | 44 | .47 | 20/47 | 43 | 13/27 | 48 | .64 |
| Paraproteinemia | 31/93 (34)‡ | 7/17 | 41 | 23/68 | 34 | .57 | 11/40 | 28 | 12/27 | 44 | .15 |
| Extrahilar lymphadenopathy (yes) | 30/108 (28) | 7/22 | 32 | 18/76 | 24 | .44 | 12/48 | 25 | 5/22 | 19 | .52 |
| PS >0 | 12/108 (11) | 3/22 | 14 | 9/76 | 12 | .82 | 7/48 | 15 | 2/27 | 7 | .36 |
| Spleen size, median (range), cm | 20 (16-25) | ||||||||||
| Spleen size (>20 cm) | 36/105 (34) | 6/20 | 30 | 24/75 | 32 | .86 | 14/47 | 30 | 9/27 | 33 | .75 |
| HPLL/SLSG (group B/C) | 64/104 (62) | 16/22 | 73 | 42/73 | 58 | .20 | 30/46 | 65 | 11/26 | 42 | .059 |
| Response to induction | .48§ | .027§ | |||||||||
| CR | 47/106 (44) | 9/22 | 41 | 38/76 | 50 | NA | 28/48 | 58 | 10/27 | 37 | NA |
| CRu | 22/106 (21) | 7/22 | 32 | 15/76 | 20 | NA | 11/48 | 23 | 4/27 | 15 | NA |
| PR | 29/106 (27) | 6/22 | 27 | 23/76 | 30 | NA | 9/48 | 19 | 13/27 | 48 | NA |
| SD | 7/106 (7) | 0 | 0 | 0 | 0 | NA | 0 | 0 | 0 | 0 | NA |
| PD | 1/106 (1) | 0 | 0 | 0 | 0 | NA | 0 | 0 | 0 | 0 | NA |
| Nonevaluable | 2/108 (—) | 0 | 0 | 0 | 0 | NA | 0 | 0 | 0 | 0 | NA |
| . | . | No maintenance* . | Maintenance* . | . | Maintenance, 1 y† . | Maintenance, 2 y† . | . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient characteristics . | All patients, no. (%) . | No. . | % . | No. . | % . | P . | No.† . | % . | No.† . | % . | P . |
| Age, median (range), y | 65 (41-91) | ||||||||||
| Age (≥70 y) | 38/108 (35) | 11/22 | 50 | 24/76 | 32 | .11 | 17/48 | 35 | 7/27 | 26 | .40 |
| Sex (male) | 52/108 (48) | 11/22 | 50 | 36/76 | 47 | .83 | 22/48 | 46 | 13/27 | 48 | .85 |
| B symptoms (yes) | 7/108 (6) | 1/22 | 5 | 5/76 | 7 | .73 | 4/48 | 8 | 1/27 | 4 | .44 |
| LDH (elevated) | 45/106 (43) | 12/22 | 55 | 30/74 | 41 | .25 | 24/47 | 51 | 6/26 | 23 | .02 |
| Hemoglobin (<10 g/dL) | 32/100 (30) | 10/22 | 46 | 21/75 | 28 | .12 | 13/47 | 28 | 8/27 | 30 | .46 |
| Thrombocytopenia (<100 × 109/L) | 18/104 (17) | 6/22 | 27 | 10/75 | 13 | .12 | 3/47 | 6 | 7/27 | 26 | .018 |
| Lymphocytes (≥4 × 109/L) | 45/104 (43) | 7/20 | 35 | 33/75 | 44 | .47 | 20/47 | 43 | 13/27 | 48 | .64 |
| Paraproteinemia | 31/93 (34)‡ | 7/17 | 41 | 23/68 | 34 | .57 | 11/40 | 28 | 12/27 | 44 | .15 |
| Extrahilar lymphadenopathy (yes) | 30/108 (28) | 7/22 | 32 | 18/76 | 24 | .44 | 12/48 | 25 | 5/22 | 19 | .52 |
| PS >0 | 12/108 (11) | 3/22 | 14 | 9/76 | 12 | .82 | 7/48 | 15 | 2/27 | 7 | .36 |
| Spleen size, median (range), cm | 20 (16-25) | ||||||||||
| Spleen size (>20 cm) | 36/105 (34) | 6/20 | 30 | 24/75 | 32 | .86 | 14/47 | 30 | 9/27 | 33 | .75 |
| HPLL/SLSG (group B/C) | 64/104 (62) | 16/22 | 73 | 42/73 | 58 | .20 | 30/46 | 65 | 11/26 | 42 | .059 |
| Response to induction | .48§ | .027§ | |||||||||
| CR | 47/106 (44) | 9/22 | 41 | 38/76 | 50 | NA | 28/48 | 58 | 10/27 | 37 | NA |
| CRu | 22/106 (21) | 7/22 | 32 | 15/76 | 20 | NA | 11/48 | 23 | 4/27 | 15 | NA |
| PR | 29/106 (27) | 6/22 | 27 | 23/76 | 30 | NA | 9/48 | 19 | 13/27 | 48 | NA |
| SD | 7/106 (7) | 0 | 0 | 0 | 0 | NA | 0 | 0 | 0 | 0 | NA |
| PD | 1/106 (1) | 0 | 0 | 0 | 0 | NA | 0 | 0 | 0 | 0 | NA |
| Nonevaluable | 2/108 (—) | 0 | 0 | 0 | 0 | NA | 0 | 0 | 0 | 0 | NA |
HPLL, hemoglobin, platelets, lactate dehydrogenase (LDH), lymphadenopathy; NA, not applicable; PS, performance status.
The maintenance vs no maintenance comparison includes responders only (n = 98). Two patients with SD after induction also received maintenance, but they are not included in this comparison.
The comparison between 1- vs 2-y maintenance includes 75/76 patients who received maintenance, excluding 1 patient who has not completed maintenance yet.
Immunoglobulin M 20/93 (22%), immunoglobulin G 10/93 (11%), immunoglobulin A 1/93 (1%).
P value reflects the overall comparison across all categories.
Among 106 patients evaluable for response, the overall response rate after the end of induction was 92% (98/106), including 44% (47/106) CR, 21% (22/106) CRu, and 27% (29/106) partial response (PR). Seven patients had stable disease (SD) (7%), and a single patient (1%) did not complete induction due to infusion-related reactions and rapidly developed progressive disease (PD). Clinical resolution of splenomegaly and hematologic response was observed at a median time of 4 (range, 1-48) and 2 (range, 1-32) weeks, respectively.
Although maintenance was scheduled for responders only, it was given in 2 additional patients with SD. Among 78 patients, 77/78, those who had completed maintenance, were evaluable for final response assessment, whereas 50 (65%) and 27 (35%) of them received maintenance for 1 and 2 years, respectively. At the end of maintenance, 54/77 patients (70%) were in CR, 14/77 (18%) were in CRu, and 8/77 (10%) were in PR, whereas 1 patient with PR at the end of induction developed PD (Table 1). Maintenance therapy improved the quality of response in 16/77 patients: 14/22 (64%) PRs achieved either CR (n = 11) or CRu (n = 3), whereas both patients with SD achieved CR and PR. All 38 induction CRs retained their CR status. Furthermore, 4/15 patients with postinduction CRu were reclassified as CR after maintenance by BM examination.
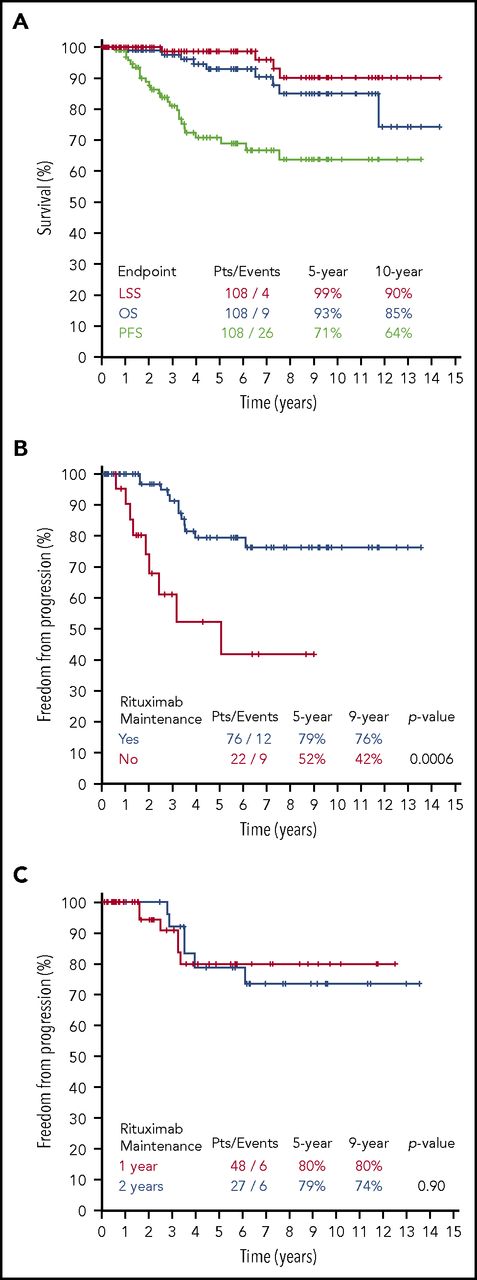
After a median follow-up of 57 months (range, 0.23-172), 26 patients experienced relapse or progression and 9 died, including 4 lymphoma-related deaths. The 5- and 10-year FFP rates were 71% and 64%; the 5- and 10-year OS rates were 93% and 85%, and the 5- and 10-year LSS rates were 99% and 90%, respectively (Figure 1A). The 5- and 10-year FFP rates according to SLSG risk group were 81% and 81% for group A and 61% and 49% for groups B/C, respectively (P = .049) . The corresponding 5- and 10-year OSs were 95% and 89% for group A and 91% and 81% for groups B/C, respectively (P = .79).
Survival outcomes after rituximab monotherapy in SMZL patients. (A) OS, LSS, and FFP for the total population of the 108 SMZL patients. (B) FFP according to Maintenance. (C) FFP according to 1 or 2 years maintenance. PFS, progression-free survival; pts, patients.
Survival outcomes after rituximab monotherapy in SMZL patients. (A) OS, LSS, and FFP for the total population of the 108 SMZL patients. (B) FFP according to Maintenance. (C) FFP according to 1 or 2 years maintenance. PFS, progression-free survival; pts, patients.
Thrombocytopenia <100 × 109/L was the only baseline variable associated with inferior FFP rates (75% vs 49% at 5 years, P = .02). Among responders, the quality of response to induction did not affect FFP rates: the 5-year FFP rates were 75%, 63%, and 61% for patients in CR, CRu, and PR, respectively (P = .46).When the analysis was restricted to responders who received rituximab maintenance, the 5-year FFP was again similar among CR, CRu, and PR patients (77%, 89%, 67%, P = .45).
Among the 98 responders to rituximab induction, 76 received maintenance. Patients’ risk group, baseline characteristics, and response after induction did not differ between those who received maintenance or not (Table 1). Patients who received 1 vs 2 years of maintenance did not differ significantly in their characteristics, except for a higher frequency of thrombocytopenia and PR to induction in those who received 2-year maintenance (Table 1). Maintenance therapy was associated with a significantly better FFP rate: 5- and 9-year FFP rates were 79% and 76% for patients who received maintenance vs 52% and 42% for those who did not (P = .0006; Figure 1B). There was no difference in FFP between those who received maintenance for 1 vs 2 years (P = .90; Figure 1C). In order to further ensure the reliability of the observation that maintenance was associated with a significantly better FFP rate compared with observation only, we performed multivariate analysis, including also thrombocytopenia and sex. These 3 covariates (male sex, absence of thrombocytopenia, and rituximab maintenance) were independent favorable prognostic factors: rituximab maintenance was the most powerful with a hazard ratio (HR) of 0.18 (95% confidence interval [CI], 0.07-0.46; P < .001), followed by platelets >100 × 109/L (HR 0.22, 95% CI, 0.08-0.59; P = .003), and male sex (HR 0.35, 95% CI, 0.13-0.92; P = .033). The addition of age, anemia, and elevated LDH did not modify the 3-variable model. Despite the large difference in FFP rate, there was no difference in OS and LSS rates: 10-year OS was 89% vs 92% (P = .84) and the 10-year LSS was 93% vs 100% (P = .50) for the maintenance vs no maintenance comparison, respectively. A plateau in the FFP rate beyond 6 to 7 years appeared to exist for patients who received maintenance. Indeed, 33% of the patients (25/76) still remained at risk for relapse/progression beyond 74 months with no additional events observed (Figure 1B). When analyzed according to post–maintenance response, only 1 of these patients still had a PR, whereas 3/25 and 21/25 patients had achieved CRu or CR, respectively.
The results presented here confirm that rituximab is a highly effective and splenectomy-sparing therapeutic strategy for SMZL. Responses to rituximab appear to be long lasting with a 10-year FFP exceeding 60%, with minimal toxicity. Maintenance therapy further improved the quality of responses and was associated with better FFP. As this was not a randomized trial, the superiority of maintenance should be interpreted with caution. This study carries the usual potential biases associated with retrospective studies, while the numbers of patients receiving maintenance or not and the numbers of events are not high enough to permit definite conclusions to be drawn. Based on these data, we recommend rituximab monotherapy as the first-line treatment of choice in SMZL. For the small proportion of patients who do not respond to rituximab, splenectomy or the addition of chemotherapy would be reasonable.19-25
Authorship
Contribution: C.K., G.A.P., T.P.V., M.K.A. designed and performed the research, analyzed the data, and wrote and/or critically reviewed the paper; T.P.V. performed statistical analysis; S.S., P. Tsirkinidis, F.N.K., M.M., X.Y., E.K., M.N.D., S.I.K., M.-C.K., M.P.S., G.T., P. Tsaftaridis, E.P., H.A.P., and P.P. enrolled patients and collected data; P.K. and D.R. contributed to the histopathologic diagnosis of the disease; and all authors participated in the editing of the manuscript and approved the final version.
Conflict-of-interest disclosure: C.K. reports honoraria from Roche and Janssen. G.A.P. reports honoraria from Roche, Janssen and Abbvie. S.S. reports honoraria from Roche, Genesis, Takeda, and Gilead. E.K. reports honoraria from Roche and serves as medical advisor at Janssen. M.-C.K. reports honoraria from Genesis and Amgen and research funding from Janssen and Genesis, and serves on speakers bureau/advisory committees from Janssen, Genesis, and Amgen. M.P.S. reports honoraria and advisory fees from Takeda, a research grant from Genesis, and advisory fees from Roche. P.K. reports honoraria from Takeda, Novartis, BMS, and MSD. P. Tsaftaridis reports advisory fees from Shire, Novartis, and Genzyme. H.A.P. reports a research grant from Roche. P.P. reports honoraria, advisory fees, and a research grant from Janssen and Gilead; honoraria from Abbvie; and research grants from Winmedica, Abbvie, and Novartis. M.K.A. reports honoraria, advisory fees, and a research grant from Takeda; honoraria and advisory fees from Novartis, Janssen, Winmedica, Genesis Pharma, Abbvie, and Roche; honoraria from Amgen; and advisory fees from Pfizer. T.P.V. reports honoraria and advisory fees from Takeda, Roche, Bristol, Genesis, Novartis; honoraria from Amgen and Winmedica; and advisory fees from Janssen. The remaining authors declare no competing financial interests.
Correspondence: Christina Kalpadakis, University Hospital of Crete, Hematology Department, Stavrakia Voutes Heraklion, Heraklion, 71500 Greece; e-mail: xkalpadaki@yahoo.gr.
REFERENCES
Author notes
G.A.P., M.K.A., and T.P.V. contributed equally to this study.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal