Key Points
Platelets, neutrophils, and coagulation factor XII are implicated as important players in experimental venous thrombosis pathophysiology.
We demonstrate that platelets, but not neutrophils, are critical in spontaneous venous thrombosis, whereas low factor XII aggravates thrombosis.
Abstract
Recently, platelets, neutrophils, and factor XII (FXII) have been implicated as important players in the pathophysiology of venous thrombosis. Their role became evident in mouse models in which surgical handling was used to provoke thrombosis. Inhibiting anticoagulation in mice by using small interfering RNA (siRNA) targeting Serpinc1 and Proc also results in a thrombotic phenotype, which is spontaneous (no additional triggers) and reproducibly results in clots in the large veins of the head and fibrin deposition in the liver. This thrombotic phenotype is fatal but can be fully rescued by thrombin inhibition. The mouse model was used in this study to investigate the role of platelets, neutrophils, and FXII. After administration of siRNAs targeting Serpinc1 and Proc, antibody-mediated depletion of platelets fully abrogated the clinical features as well as microscopic aspects in the head. This was corroborated by strongly reduced fibrin deposition in the liver. Whereas neutrophils were abundant in siRNA-triggered thrombotic lesions, antibody-mediated depletion of circulating Ly6G-positive neutrophils did not affect onset, severity, or thrombus morphology. In addition, absence of circulating neutrophils did not affect quantitative liver fibrin deposition. Remarkably, siRNA-mediated depletion of plasma FXII accelerated the onset of the clinical phenotype; mice were affected with more severe thrombotic lesions. To summarize, in this study, onset and severity of the thrombotic phenotype are dependent on the presence of platelets but not circulating neutrophils. Unexpectedly, FXII has a protective effect. This study challenges the proposed roles of neutrophils and FXII in venous thrombosis pathophysiology.
Introduction
Venous thrombosis (VT) is a complex disease, and its pathogenesis is incompletely understood. It has recently been recognized that cellular components of the blood may contribute to the initiation and propagation of VT.1,2 Mouse models have been important tools for studying the pathogenesis of VT. In models based on flow restriction (stasis) induced by partial ligation of the inferior vena cava and in the absence of any vascular and/or endothelial damage, it was shown by von Brühl et al1 and others that blood leukocytes were actively recruited to the inflamed venous vessel wall, resulting in initiation and propagation of VT.1-3 An interplay between these recruited blood cells (mainly platelets and neutrophils) and coagulation factor XII (FXII) appeared to be critical for thrombus formation.1
Although this mouse model for VT proved to be valuable for identifying potential novel players in VT, the role of blood stasis, hypoxia, and endothelial activation may be overestimated compared with VT in humans,1,3 especially in cases in which imbalanced coagulation, as a result of either environmental conditions or genetic background, is the driving risk factor for VT.4,5 It cannot be excluded that in the model used by von Brühl et al, the numerous surgical handlings required to establish stasis in the inferior vena cava contributed to a proinflammatory state. Furthermore, the retrograde formation of thrombi is an important difference between that model and the human situation.
Recently, we described a mouse model with an acute imbalance in coagulation that was achieved by strong inhibition of the hepatic expression of antithrombin (Serpinc1) and protein C (Proc) using synthetic small interfering RNA (siRNA).6 Inhibition of these anticoagulants resulted in a highly reproducible siRNA dose-dependent and thrombin-dependent thrombotic coagulopathy which, without interventions, is fatal. Likely as a result of vascular bed–specific hemostasis and local flow characteristics,7 (fibrin-layered) thrombi were reproducibly formed in large veins in the head (in and around the mandibular area). Moreover, fibrin was deposited in the liver, and plasma fibrinogen was consumed which resulted in prolonged clotting times. Because thrombus initiation and propagation in this model required no additional triggers other than inhibition of anticoagulant gene expression (achieved by intravenous siRNA injection), we used this model to further evaluate the role of platelets, neutrophils, and FXII in the initiation and propagation of VT.
Methods
Animal experiments
C57BL/6J female mice (18-20 g) were purchased from Charles River (Maastricht, The Netherlands). siRNAs targeting mouse antithrombin (siSerpinc1; cat. #S62673; Ambion, Carlsbad, CA), protein C (siProc; cat. #S72192), and a control siNEG (cat. #4404020) were designed and/or used as described previously.6 For siRNA-mediated silencing of coagulation FXII (F12), RNA strand sequences were sense: 5′-CCACAAAUGCAUCCACAAAtt-3′ and antisense: 5′-UUUGUGGAUGCAUUUGUGGtg-3′ (cat. #S81735). For in vivo use, siRNAs were complexed with Invivofectamine 2.0 (Invitrogen, Carlsbad, CA) and injected intravenously (tail vein) at a dose of 5.75 mg/siRNA per kg of body weight. This dose reproducibly results in spontaneous macrovascular VT limited to the head (in the masseter and mandibular area), irrespective of sex and strain. siRNA complexes targeting F12 were injected 24 hours before treatment with siSerpinc1/siProc.
For platelet depletion, a rat monoclonal antibody against mouse GP1b (#R300; Emfret, Würzburg, Germany) was used. Depletion of neutrophils was achieved by using a rat monoclonal antibody targeting mouse Ly6G (clone 1A8; BioLegend, San Diego, CA) and a rat isotype control immunoglobulin G (IgG; clone RTK2758; BioLegend) as a control. Antibodies were injected intravenously (5 milligrams per kilogram of body weight) 6 hours after siSerpinc1/siProc injection, unless otherwise indicated.
Liver and blood analyses
Liver transcript levels of Serpinc1, Proc, and F12 were determined by using quantitative polymerase chain reaction, with Actb as a housekeeping gene.8,9 siRNA-mediated hepatic silencing of Serpinc1 and Proc silencing were routinely confirmed.6 Liver fibrin deposition was determined by immunoblotting using the monoclonal antibody 59D8.10
Blood neutrophil numbers were measured by using flow cytometry (LSR II; BD Biosciences, San Jose, CA) using αLy6G-phycoerythrobilin (clone 1A8; BD Biosciences). Platelet and neutrophil numbers were determined with a hematology analyzer (Sysmex XE-2100). Ex vivo platelet activity (with and without stimulus) was determined as described.11 Plasma FXII activity was determined by using an activated partial thromboplastin time (aPTT)–based assay with FXII-deficient human plasma and C57BL/6J mouse pool plasma for calibration.9 Plasma nucleosome levels and thrombin generation (tissue factor and ellagic acid–induced) were determined as described.12,13
Phenotype assessment
The spontaneous thrombotic phenotype after siSerpinc1/siProc injection has been described extensively,6 and it developed in all mice 2 to 3 days after siRNA injection. Because of the severe nature of the clinical symptoms that accompanied the thrombotic phenotype, animals were euthanized 72 hours after siSerpinc1/siProc injection unless otherwise indicated.
After the mice were euthanized and dissected (not including animal perfusion), formalin-fixed heads were decalcified in 20% formic acid, dehydrated, embedded in paraffin, and sectioned. After analysis of coronal serial sections of the head and neck, 4-μm sections were made starting directly caudal of the eyes, because this area was most clearly and reproducibly affected and because thrombi in large veins were found here (in siSerpinc1/siProc-injected animals). Selected sections were stained by using hematoxylin and eosin or according to Carstairs’ methodology.14 Severity of the phenotype at the microscopic level was scored on the basis of the presence and extent of thrombotic lesions, subcutaneous and intramuscular bleeding, and subcutaneous edema in the entire section (supplemental Figure 4, available on the Blood Web site). Incidence and appearance of thrombotic lesions in the selected sections were categorized and scored (supplemental Figure 6).
Immunohistochemistry
Paraffin-embedded coronal sections of the head area (ie, serial sections of those described above) were stained with a rat monoclonal anti-mouse Ly6G (clone 1A8; BioLegend). A horseradish peroxidase–labeled rabbit anti-rat IgG antibody (Dako, Glostrup, Denmark) was used for detection. Horseradish peroxidase activity was detected by using diaminobenzidine (Dako).
Results
Platelets are crucial for spontaneous thrombosis
In animals treated with siSerpinc1/siProc, platelets (Carstairs’ light blue positive) appeared abundantly present in thrombi and were also co-localized with both leukocytes (dark blue/purple) and fibrin (bright red/pink; supplemental Figure 1A) in the mandibular area of the head. In addition, a reduction in blood platelet counts coincided with increased liver fibrin deposition and development of the clinical features of the thrombotic coagulopathy (supplemental Figure 1B). Flow cytometry analysis showed that the circulating platelets did not display a significant increase in surface activation markers before onset of the thrombotic phenotype (supplemental Figure 1C). To investigate the role of platelets during spontaneous thrombotic coagulopathy after silencing of anticoagulant genes Serpinc1 and Proc, platelets were depleted by using an antibody targeting mouse GP1b 6 hours after injection of siSerpinc1/siProc. Successful platelet depletion (no platelets detectable in whole blood) was confirmed in a dedicated pilot study (data not shown) and in a parallel group that did not receive siSerpinc1/siProc (median, 616 × 109/L [range, 554-642 × 109/L] vs 0 × 109/L [range, 0-7 × 109/L]; P = .036; Figure 1A).
Depletion of platelets prevents thrombotic coagulopathy after siRNA-mediated hepatic knockdown of Serpinc1 and Proc. (A) Blood platelet numbers in mice from a parallel group not receiving siRNA 3 days after injection with saline (open circles) or with a rat monoclonal antibody targeting mouse GP1b (solid circles) (Mann-Whitney rank sum test P = .036). (B) Scoring of the clinical phenotype in mice treated with siRNAs targeting Serpinc1 and Proc. Animals showing characteristic clinical coagulopathy (hatched bar) and animals unaffected (open bars) 3 days after siRNA treatment (end of experiment). One of the mice from the –αGP1b group died as a result of the thrombotic coagulopathy (Fisher’s exact test P = .001). (C) Representative thrombus identified in a vein in the control group (–αGP1b), and (D) a representative vein in the platelet-depleted group (+αGP1b) in hematoxylin and eosin–stained sections. Scale bars represent 100 μm. (E) Scoring for the presence of thrombi: 0, no thrombi found; I and II, thrombi categories based on structure and layering (see “Methods” and supplemental Figure 4). Open bars, –αGP1b (n = 10); solid bar, +αGP1b (n = 16). (F) Levels of fibrin deposition in the liver of the platelet-depleted group (+αGP1b) and the control group (–αGP1b) (Mann-Whitney rank sum test P = .001). Solid and dashed lines indicate fibrin levels found only in siNEG-injected C57BL/6J female mice (median, 4.5 ng/mg; range, 3.1-5.7 ng/mg). mus, striated muscle tissue; n.d., not detected; thr, thrombus with typical fibrin layers; rbc, postmortem clotted blood rich in red blood cells.
Depletion of platelets prevents thrombotic coagulopathy after siRNA-mediated hepatic knockdown of Serpinc1 and Proc. (A) Blood platelet numbers in mice from a parallel group not receiving siRNA 3 days after injection with saline (open circles) or with a rat monoclonal antibody targeting mouse GP1b (solid circles) (Mann-Whitney rank sum test P = .036). (B) Scoring of the clinical phenotype in mice treated with siRNAs targeting Serpinc1 and Proc. Animals showing characteristic clinical coagulopathy (hatched bar) and animals unaffected (open bars) 3 days after siRNA treatment (end of experiment). One of the mice from the –αGP1b group died as a result of the thrombotic coagulopathy (Fisher’s exact test P = .001). (C) Representative thrombus identified in a vein in the control group (–αGP1b), and (D) a representative vein in the platelet-depleted group (+αGP1b) in hematoxylin and eosin–stained sections. Scale bars represent 100 μm. (E) Scoring for the presence of thrombi: 0, no thrombi found; I and II, thrombi categories based on structure and layering (see “Methods” and supplemental Figure 4). Open bars, –αGP1b (n = 10); solid bar, +αGP1b (n = 16). (F) Levels of fibrin deposition in the liver of the platelet-depleted group (+αGP1b) and the control group (–αGP1b) (Mann-Whitney rank sum test P = .001). Solid and dashed lines indicate fibrin levels found only in siNEG-injected C57BL/6J female mice (median, 4.5 ng/mg; range, 3.1-5.7 ng/mg). mus, striated muscle tissue; n.d., not detected; thr, thrombus with typical fibrin layers; rbc, postmortem clotted blood rich in red blood cells.
Fully in line with previous observations,6 animals treated with siRNAs targeting Serpinc1 and Proc and subsequently injected with saline (designated as –αGP1b in Figure 1) developed the typical clinical features of the thrombotic coagulopathy within 3 days. Mice developed unilateral lesions around the eye and swellings in the head. Moreover, they became lethargic, unresponsive to stimuli, and hypothermic and showed a significant loss in body weight. One of the affected mice died before it could be included in further analysis. In contrast, siSerpinc1/siProc +αGP1b mice (+αGP1b in Figure 1) appeared fully healthy (Figure 1B) and did not experience weight loss compared with the siSerpinc1/siProc –αGP1b group, which emphasizes their retained health (−2.05 g [range, –3.05-0.15 g] vs 0.13 g [range, –0.99-0.77 g]; P = .043; supplemental Figure 2A). Strikingly, platelet depletion at a later time point (siSerpinc1/siProc-treated mice received αGP1b when the first 2 mice presented with the clinical features of the thrombotic phenotype) also fully rescued mice from thrombotic coagulopathy. All mice in the reference group became affected as expected (9 of 9 in the –αGP1b group vs 2 of 9 in the +αGP1b group; P = .002).
On a microscopic level, thrombi were found in all mice in the larger and smaller veins of the selected coronal sections of the head in the siSerpinc1/siProc –αGP1b group (Figure 1C; supplemental Figure 3). Moreover, extensive multifocal red blood cell extravasations (hemorrhages) were present especially in the masseter and mandibular area, with associated subcutaneous edema (7 of 7 mice). In contrast, neither thrombi nor notable injuries were observed in the siSerpinc1/siProc +αGP1b mice (Figure 1D; supplemental Figures 3 and 5A). When the presence of thrombi was scored, 2 types of thrombi were defined on the basis of their composition and structure (Figure 1E; supplemental Figure 6). Interestingly, 1 mouse that was not yet clinically affected did appear to have thrombi in a vessel in the investigated coronal section of the head (–αGP1b; Figure 1B). In contrast, no mice in the siSerpinc1/siProc +αGP1b group appeared to have any thrombi. In line with these observations, liver fibrin deposition was strongly and significantly reduced in the siSerpinc1/siProc +αGP1b group (75.7 ng/mg [range, 21.4-143.9 ng/mg] vs 9.5 ng/mg [range, 6.3-21.7 ng/mg]; P = .001; Figure 1F), although liver fibrin levels were above the background level observed in control animals injected only with control siRNA (siNEG, 4.5 ng/mg [range, 3.1-5.7 ng/mg]; P < .001; Figure 1F).
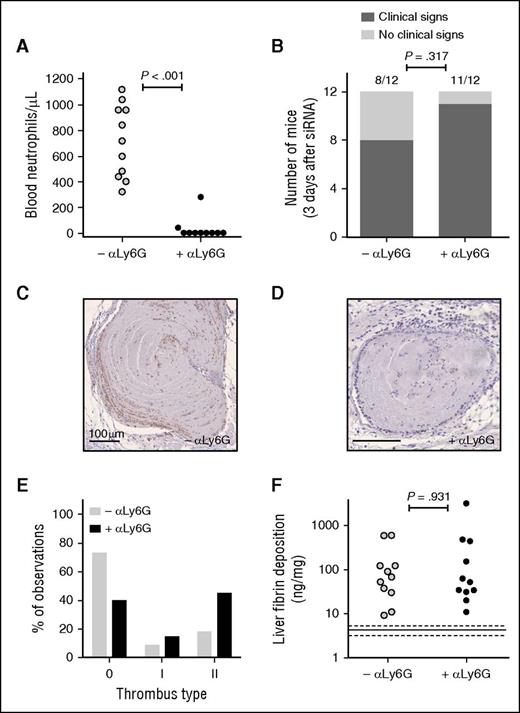
Circulating neutrophils are not a major mediator of spontaneous thrombosis
Mice were depleted of neutrophils 6 hours after siSerpinc1/siProc injection by using an antibody targeting the neutrophil-specific Ly6G membrane protein (+αLy6G; Figure 2). In this experimental setup, an isotype IgG antibody was used in the group not depleted of neutrophils (–αLy6G; Figure 2). Flow cytometry analysis confirmed in a dedicated experiment that the Ly6G-positive (ie, neutrophil population) was fully absent in the circulation up to 4 days after antibody injection (data not shown). By using the same approach, we again did not detect neutrophils in the circulation in the siSerpinc1/siProc +αLy6G group 1 day after antibody injection and 1 day before onset of the phenotype (supplemental Figure 7). In addition, after euthanasia, the absence of neutrophils in the group treated with siSerpinc1/siProc +αLy6G was confirmed (720 neutrophils per μL [range, 320-1120 neutrophils per μL] vs 0 neutrophils per μL [range, 0-280 neutrophils per μL]; P < .001; Figure 2A).
Depletion of neutrophils does not influence progression of thrombotic coagulopathy after siRNA-mediated hepatic knockdown of Serpinc1 and Proc. (A) Blood neutrophil numbers in mice 3 days after injection with a rat monoclonal antibody targeting mouse Ly6G (solid circles) or a rat IgG control (open circles) (Mann-Whitney rank sum test P < .001). (B) Scoring of the clinical phenotype in mice treated with siRNAs targeting Serpinc1 and Proc. Animals showing characteristic clinical signs (hatched bars) and animals unaffected (open bars) 3 days after siRNA treatment (end of experiment). One of the mice in each group (–αLy6G and +αLy6G) died as a result of the thrombotic coagulopathy (Fisher’s exact test P = .317). (C-D) Ly6G staining of thrombi found in sections of the head in (C) the –αLy6G and (D) the +αLy6G group. Hematoxylin was used for counterstaining; Scale bars represent 100 μm. (E) Scoring for the presence of thrombi: 0, no thrombi found; I and II, thrombi categories based on structure and layering. Open bars, –αLy6G (n = 22); solid bars, +αLy6G (n = 20). (F) Levels of fibrin deposition in the liver of the neutrophil-depleted group (+αLy6G) and the control group (–αLy6G) (Mann-Whitney rank sum test P = .931). Solid and dashed lines indicate fibrin levels found only in siNEG-injected C57BL/6J female mice (median, 4.5 ng/mg; range, 3.1-5.7 mg/mg).
Depletion of neutrophils does not influence progression of thrombotic coagulopathy after siRNA-mediated hepatic knockdown of Serpinc1 and Proc. (A) Blood neutrophil numbers in mice 3 days after injection with a rat monoclonal antibody targeting mouse Ly6G (solid circles) or a rat IgG control (open circles) (Mann-Whitney rank sum test P < .001). (B) Scoring of the clinical phenotype in mice treated with siRNAs targeting Serpinc1 and Proc. Animals showing characteristic clinical signs (hatched bars) and animals unaffected (open bars) 3 days after siRNA treatment (end of experiment). One of the mice in each group (–αLy6G and +αLy6G) died as a result of the thrombotic coagulopathy (Fisher’s exact test P = .317). (C-D) Ly6G staining of thrombi found in sections of the head in (C) the –αLy6G and (D) the +αLy6G group. Hematoxylin was used for counterstaining; Scale bars represent 100 μm. (E) Scoring for the presence of thrombi: 0, no thrombi found; I and II, thrombi categories based on structure and layering. Open bars, –αLy6G (n = 22); solid bars, +αLy6G (n = 20). (F) Levels of fibrin deposition in the liver of the neutrophil-depleted group (+αLy6G) and the control group (–αLy6G) (Mann-Whitney rank sum test P = .931). Solid and dashed lines indicate fibrin levels found only in siNEG-injected C57BL/6J female mice (median, 4.5 ng/mg; range, 3.1-5.7 mg/mg).
Mice treated with siSerpinc1/siProc in both the neutrophil-depleted (siSerpinc1/siProc +αLy6G) and the isotype IgG–treated group (siSerpinc1/siProc –αLy6G) developed the typical clinical signs of the thrombotic coagulopathy (Figure 2B). Moreover, body weight was lowered for mice in both groups to a comparable extent (−0.85 g [range, –3.24-0.13 g] vs −2.48 g (range, –3.61 to −0.31 g); P = .132; supplemental Figure 2B). Coronal sections of the head were analyzed on a microscopic level, and thrombi were found in large veins along with hemorrhages and edema in both groups. Severity scoring yielded no differences in severity (supplemental Figure 5B). In the siSerpinc1/siProc –αLy6G group, Ly6G-positive cells were abundantly present in thrombi, they followed the alignment of structures identified as fibrin, and they adhered to the thrombotic venous vessel wall (Figure 2C). Ly6G-positive cells in thrombi were absent in the siSerpinc1/siProc +αLy6G group (although in some animals, strongly reduced Ly6G-positive signal was found in some cells in the thrombus; Figure 2D). Generally, thrombus leukocyte density was affected after neutrophil depletion (compare in Figure 2C-D and supplemental Figure 8). Depletion of neutrophils did not significantly affect the organizational structure and lining of the thrombi (Figure 2E; supplemental Figure 6). In line with these observations, increased liver fibrin deposition compared with an siNEG control group of mice was evident, but no differences between groups treated with siSerpinc1/siProc were observed (67.9 ng/mg [range, 9.3-587.5 ng/mg] vs 51.9 ng/mg [range, 10.9-3126.0 ng/mg]; P = .931; Figure 2F).
To investigate whether the thrombotic coagulopathy after injection of siSerpinc1/siProc coincided with the formation of neutrophil extracellular traps (NETs) and whether neutrophil depletion affects NET formation, we determined plasma levels of extracellular nucleosomes as a NET biomarker.12 Plasma nucleosome levels were moderately but significantly increased (siSerpinc1/siProc –αLy6G [P = .003] and siSerpinc1/siProc +αLy6G [P < .001]) in mice with thrombotic coagulopathy when compared with untreated mice (supplemental Figure 9). However, no differences were found in plasma from mice with or without detectable neutrophils in the circulation (siSerpinc1/siProc –αLy6G: 46 U/mL [range, 7-756 U/mL]; siSerpinc1/siProc +αLy6G: 59 U/mL [range, 10-771 U/mL]; P = .448), suggesting that extracellular nucleosomes detected in plasma of thrombotic animals were not derived from neutrophils.
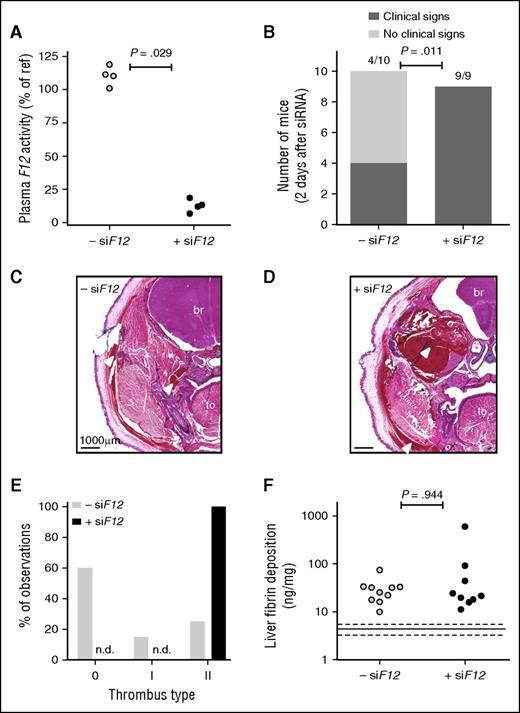
Reduced FXII propagates development of spontaneous venous thrombosis
The role of FXII was studied by using an siRNA approach (siF12). For mice treated with siF12 only (without siSerpinc1/siProc injections), FXII plasma activity was decreased (72 hours after siRNA injection) by 87.3% (range, 93.2%-81.4%; P = .029) compared with pooled plasma, whereas FXII levels in the siNEG-treated group were in the normal range (110.9% [range, 101.0%-118.9%] of pooled plasma; Figure 3A). Moreover, groups treated with siSerpinc1/siProc in combination with siF12 (+siF12) or siNEG (–siF12) (Figure 3) were analyzed for hepatic F12 transcript levels (after euthanasia). A reduction in hepatic F12 transcript of 86.0% (range, 87.9%-84.9%; P < .001) was observed in the siSerpinc1/siProc +siF12 group.
siRNA-mediated hepatic knockdown of F12 worsens thrombotic coagulopathy induced by knockdown of Serpinc1 and Proc. (A) Plasma FXII activity in mice 3 days after injection with an siRNA targeting F12 (solid circles) or siNEG (open circles) (Mann-Whitney rank sum test P = .029). Normal pooled plasma was used as an internal reference. (B) Clinical phenotype in mice treated with siRNAs targeting Serpinc1 and Proc. Animals showing characteristic clinical signs (hatched bars) and unaffected animals (open bars) 2 days after siRNA treatment (end of experiment) (Fisher’s exact test P = .011). (C-D) Representative hematoxylin and eosin–stained coronal head sections from (C) the –siF12 group and (D) the +siF12 group. Scale bars represent 1000 μm. Arrowhead indicates extravasated red blood cells. (E) Scoring for the presence of thrombi: 0, no thrombi found; I and II, thrombi categories based on structure and layering. Open bars, –siF12 (n = 20); solid bars, +siF12 (n = 18). (F) Levels of fibrin deposition in the liver of the FXII deficient group (+siF12) and the control group (–siF12) (Mann-Whitney rank sum test P = .944). Solid and dashed lines indicate fibrin levels found only in siNEG-injected C57BL/6J female mice (median, 7.1 ng/mg; range, 6.1-8.0 mg/mg). br, brain; to, tongue; n.d., not detected.
siRNA-mediated hepatic knockdown of F12 worsens thrombotic coagulopathy induced by knockdown of Serpinc1 and Proc. (A) Plasma FXII activity in mice 3 days after injection with an siRNA targeting F12 (solid circles) or siNEG (open circles) (Mann-Whitney rank sum test P = .029). Normal pooled plasma was used as an internal reference. (B) Clinical phenotype in mice treated with siRNAs targeting Serpinc1 and Proc. Animals showing characteristic clinical signs (hatched bars) and unaffected animals (open bars) 2 days after siRNA treatment (end of experiment) (Fisher’s exact test P = .011). (C-D) Representative hematoxylin and eosin–stained coronal head sections from (C) the –siF12 group and (D) the +siF12 group. Scale bars represent 1000 μm. Arrowhead indicates extravasated red blood cells. (E) Scoring for the presence of thrombi: 0, no thrombi found; I and II, thrombi categories based on structure and layering. Open bars, –siF12 (n = 20); solid bars, +siF12 (n = 18). (F) Levels of fibrin deposition in the liver of the FXII deficient group (+siF12) and the control group (–siF12) (Mann-Whitney rank sum test P = .944). Solid and dashed lines indicate fibrin levels found only in siNEG-injected C57BL/6J female mice (median, 7.1 ng/mg; range, 6.1-8.0 mg/mg). br, brain; to, tongue; n.d., not detected.
To investigate whether thrombin generation (TG) was altered in mice with lower levels of FXII, we performed a TG assay on plasma from mice 48 hours after siF12 treatment (ie, 24 hours after siSerpinc1/siProc injection) with ellagic acid (contact activation initiated) or tissue factor as triggers for TG. At this time point, animals did not show any clinical singularities and were completely healthy. Endogenous thrombin potential values did not differ between siSerpinc1/siProc –siF12 and siSerpinc1/siProc +siF12 groups in both measurements (ellagic acid: 1019 nM/min [range, 518-1810 nM/min] for –siF12 vs 1488 nM/min [range, 552-1689 nM/min) for +siF12; P = .151; tissue factor: 919 nM/min [range, 670-2073 nM/min] for –siF12 vs 807 nM/min [range, 613-949 nM/min] for +siF12; P = .193), and no other differences were observed in TG curves (data not shown). In line with these observations, low FXII did not significantly affect aPTT (as determined in siNEG and siF12-only animals; 38.7 seconds [range, 32.5-38.9 seconds] vs 39.4 seconds [range, 38.3-45.9 seconds]; 1:1 diluted plasma; P = .40).
Remarkably, with lower plasma levels of FXII, mice treated with siRNAs against Serpinc1 and Proc (siSerpinc1/siProc +siF12) developed earlier and more severe clinical symptoms of thrombosis compared with the group treated with siNEG (siSerpinc1/siProc –siF12: 4 of 10 vs 9 of 9; P = .011; Figure 3B). Because the onset of the clinical symptoms was premature (within 48 hours after siSerpinc1/siProc treatment) compared with previous experiments, we stopped the experiment and euthanized animals 2 days after treatment with siSerpinc1/siProc. To emphasize the difference between groups, mice with decreased FXII experienced significantly more body weight loss during the experiment (−0.05 grams [range, –1.60-0.60 grams] vs −2.30 grams [range, –3.10 to −1.60 grams]; P < .001; supplemental Figure 2C). This surprising outcome was confirmed in a second independent experiment with an identical setup; in the siSerpinc1/siProc +siF12 group, onset of the typical coagulopathy was again evident in a large majority of mice 2 days after injection of siSerpinc1/siProc, whereas animals in the siSerpinc1/siProc –siF12 group were healthy at this early time point (0 of 8 and 7 of 8; P = .001; body weight gain: −0.35 grams (range, –0.70-0.50 grams) vs −0.95 grams (range, –1.90 to −0.20 grams]; P = .004).
On a microscopic level, thrombus formation, hemorrhages, and edema were more severe in the siSerpinc1/siProc +siF12 group compared with the siSerpinc1/siProc –siF12 group (Figure 3C-D; supplemental Figure 5C for severity scoring). Blinded analysis of the coronal sections showed that thrombotic lesions characterized by structured fibrin layering were present in the siSerpinc1/siProc –siF12 group but absent in the siSerpinc1/siProc +siF12 group (Figure 3E). Instead, in the siSerpinc1/siProc +siF12 group, lesions were observed mostly in disrupted veins consisting of mixtures of red blood cells and structures identified as eosin-positive fibrin lacking a typical layered structure (type II thrombotic lesions). However, detailed histologic analysis of the thrombi did not provide any suggestions that low FXII levels have a unique impact on clot structure. Despite the more severe clinical phenotype and more severe lesions observed microscopically in the siSerpinc1/siProc +siF12 group, liver fibrin deposition levels were comparable for groups treated with siSerpinc1/siProc (–siF12: 28.7 ng/mg [range, 10.0-74.6 ng/mg]; +siF12: 21.6 ng/mg [range, 11.2-596.1 ng/mg; P = .944; Figure 3F).
Discussion
In this study, we investigated the role of platelets, neutrophils, and FXII in the pathophysiology of VT by using a mouse model that featured spontaneous onset of VT (ie, in a thrombosis model that does not require additional triggers or handling other than silencing expression of 2 liver-derived anticoagulants through simple intravenous injection of synthetic siRNAs). In this model, platelets, but not neutrophils, were found to be rate-limiting in thrombus formation, whereas low plasma FXII was found to aggravate spontaneous thrombosis. The results of this study therefore challenge the proposed roles of neutrophils and FXII in VT pathophysiology.
Platelets, recently identified as major players in experimental VT in a ligation model, are recruited early after flow restriction and are involved in stabilization and accumulation of innate immune cells.1 Thrombus formation does not take place in the absence of platelets. Also in this study, rescue from thrombotic coagulopathy after platelet depletion was complete. These observations provide further evidence for an important role of platelets during experimental VT and are in line with previous studies.1,15
In our model, thrombotic coagulopathy rapidly progresses and transitions within hours from a condition in which animals have no detectable thrombotic lesions in the head and minimal liver fibrin deposition toward a condition in which veins in the head are occluded with thrombi and liver fibrin deposition is evident. We now suggest that platelets are particularly important for the burst of fibrin and thrombus formation but not for initial fibrin formation. This is supported by the fact that thrombi were not detected in platelet-depleted mice, whereas liver fibrin deposition was found to be increased compared with baseline level (Figure 1F). In addition, late platelet depletion just before the expected onset of the thrombotic phenotype fully rescues. Finally, von Willebrand factor (VWF), a protein important for platelet adherence but not for massive fibrin formation, is not involved in siSerpinc1/siProc-induced thrombosis. VWF-deficient animals did not respond differently upon silencing of anticoagulation compared with animals that express VWF (4 of 6 Vwf−/− mice vs 5 of 6 Vwf+/+ control mice macroscopically and microscopically affected within 72 hours after injection of siSerpinc1/siProc). Overall, this study confirms an important but different role for platelets, compared with that proposed previously in VT pathophysiology, and thereby provides further evidence for investigating antiplatelet therapy as prophylactic treatment against (recurrent) VT.16,17
In recent years, neutrophils have been linked to a role in VT via a specialized cell death program in which NETs are released.18,19 During thrombus formation in a mouse model of experimental VT, NETs released upon neutrophil recruitment to the (proinflammatory) vessel wall are indispensable.1 The role of neutrophils became evident by using an antibody-mediated depletion strategy identical to the method used in this study (depletion of Ly6G-positive cells). For the electrolytic inferior vena cava model of VT in which the vena cava is directly activated by an electric current thus causing endothelial damage, it was demonstrated that vein wall neutrophils were the most common cell type present in acute VT.20 Moreover, neutrophils and NETs have also been identified in human VT.21,22
When VT followed silencing of anticoagulant genes, Ly6G-positive neutrophils were abundantly present within the thrombi, seemingly recruited and aligned to the fibrin layers, which is consistent with previous observations.1,2 However, in our model, neutrophils were not rate limiting in thrombus formation. We were unable to detect any phenotypically relevant impact of neutrophil depletion, which is in strong contrast with previous observations. Hence, the proposed role of neutrophils in the thrombosis pathophysiology does not hold true for conditions in which endothelial activation and/or vessel wall inflammation are considered absent (ie, not triggered by surgical handling). Therefore, we expect a less vital role for neutrophils in humans when manifestation of VT is clearly associated with thrombophilia.
The abundance and specific alignment of neutrophils in the spontaneously formed thrombi in the head (Figure 2C) suggest that neutrophils are not innocent bystanders during thrombosis. Neutrophils may have an active role in the inflammatory process associated with thrombosis, possibly once the thrombus is formed. The finding of occasional Ly6G-positive cells in thrombi in the siSerpinc1/siProc +αLy6G group (although undetectable in the circulation) suggests that the formed thrombi are strong triggers for neutrophil recruitment, possibly from sources other than the circulation. Overall, our data indicate that the role of neutrophils in thrombosis may depend on the trigger, which should encourage studies of the role of neutrophils after thrombus formation.
FXII has been a candidate for treatment of VT because it may be involved in thrombus formation but is not essentially involved in hemostasis.2,23,24 In our model of spontaneous VT, strong reduction in plasma FXII was achieved through silencing the hepatic transcript, which resulted in reduced plasma protein activity of 10% to 20% that of controls. At these levels, plasma performs normally in thrombin generation assays after intrinsic and extrinsic stimulation and produces normal aPTTs. Surprisingly, we observed an effect of low plasma FXII on thrombus formation: a faster onset and more severe thrombotic coagulopathy in mice with low levels of FXII.
We were puzzled by this observation and considered 3 potential mechanisms for FXII. First, we considered low FXII-enhanced secondary bleeding tendency as a mechanism underlying the observed more severe coagulopathy. In the experiment that reproduced the exacerbating effect of low FXII in spontaneous thrombosis, microscopic analysis of coronal sections of the head area showed that all animals in the siSerpinc1/siProc –siF12 group had not yet developed the thrombotic phenotype after 2 days, whereas all siSerpinc1/siProc +siF12 animals had. In other words, lowering FXII levels seemed to accelerate the onset of thrombosis, which argues against an effect of low FXII through enhancing the secondary bleeding in the head.
Second, we considered changes in the fibrinolytic pathway as a mechanism by which low FXII modulates spontaneous VT. FXII also contributes to clot structure and fibrinolysis.25-30 FXII can interact with profibrinolytic factors,25 and deficiency of FXII causes less dense or stiff clots.26,27 In line with those observations, activation of FXII with polyphosphates in normal whole blood, but not in FXII-deficient plasma, increased clot firmness.28,29 Detailed histologic analysis of the thrombi formed during our experiments, however, did not yield any information regarding whether low FXII indeed has a unique impact on clot structure. Of note, our thrombosis model was not particularly sensitive to alterations in fibrinolysis, because the antifibrinolytic agent tranexamic acid did not affect the onset or progression of siSerpinc1/siProc-mediated thrombosis (at a dose of 2.5 g/kg/d starting before siRNA injections; data not shown). This argues against an impact of low FXII levels on thrombosis onset and severity through altered clot formation and/or fibrinolysis.
Third, we considered changes in the kinin/kallikrein pathway as a mechanism by which low FXII may modulate spontaneous VT.31 We investigated the impact of low FXII on edema. Edema in the masseter and mandibular area is a clear macroscopically visible feature of spontaneous thrombosis. We hypothesized that low FXII reduces kallikrein formation and consequently the release of bradykinin, which hinders formation of edema (opposite of hereditary angioedema type III, in which a gain of function in FXII induces formation of edema).32 In thrombotic mice with low FXII, impaired edema formation would worsen the phenotypic response through an inability to manage intravenous pressure after thrombotic occlusion. Quantitation of edema in the head (measured by the thickness of the edemic dermis in coronal sections of the head) did not provide any information regarding low FXII-altered edema formation (data not shown). Because antibodies and/or chromogenic substrates for detection of (activity) mouse components of the kinin/kallikrein pathway are lacking, we are not able to provide additional data for further exploring the kinin/kallikrein pathway as a mechanism of low FXII in spontaneous thrombosis.
We conclude that in our VT model, which was based on lowering anticoagulation factors, FXII inhibition does not rescue the thrombotic phenotype. Further studies are needed to clarify the mechanisms of thrombus formation and the role of FXII and related proteins (such as coagulation factor XI) in thrombosis after impaired anticoagulation.
In this article, we challenge the proposed essential roles for platelets, neutrophils, and FXII in VT pathogenesis. Mouse models in which thrombosis is induced by stenosis-induced stasis leading to hypoxia and endothelial activation demonstrate a crucial role for these factors, but our data imply that neutrophils and FXII are not essential in thrombus formation when impaired anticoagulation is the driving force. Thus, targeting neutrophils or FXII for therapeutic purposes is an interesting thought, but it might not be applicable for treatment of every case of VT. Conversely, our study provides further rationale for antiplatelet therapy as prophylactic treatment of (recurrent) VT.
The online version of this article contains a data supplement
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank René van Oerle (Department of Internal Medicine and Biochemistry, Maastricht University, Maastricht, The Netherlands) for his contribution to the analysis of low FXII plasma and Charles Esmon (University of Oklahoma Health Sciences Center, Oklahoma City, OK) for providing the 59D8 antibody.
Authorship
Contribution: M.H., P.H.R., and B.J.M.v.V. designed the experiment; M.H., B.J.M.v.V., S.S.-A., D.S., E.H.L., B.M.L., S.S.Z., H.M.H.S., S.J.K., and G.T.M.W. performed experiments and analyzed data; M.H. and B.J.M.v.V. wrote the paper; and all authors commented on manuscript drafts.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Bart J. M. van Vlijmen, Einthoven Laboratory for Experimental Vascular Medicine, Department of Internal Medicine, Division of Thrombosis and Hemostasis, Leiden University Medical Center, Leiden, The Netherlands; e-mail: b.j.m.van_vlijmen@lumc.nl.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal