Abstract
Acute myeloid leukemia (AML) with isolated trisomy 13 (AML+13) is rare and frequently associated with FAB M0 morphology. The clinical course is not well characterized but according to the ELN classification of intermediate prognosis. Eighty to one-hundred percent of patients (pts) with AML+13 carry mutations in the RUNX1 gene. Over-expression of FLT3 (located on chromosome 13 [chr 13]) due to the additional gene copy on the third chr 13 was proposed as a mechanism of leukemogenesis in AML+13 (gene dosage hypothesis).
We set out to characterize the clinical course of AML+13 pts and elucidate their molecular background using whole exome sequencing, targeted resequencing and gene expression profiling. We identified 23 pts with AML+13 enrolled in a multicenter trial of the German AML Cooperative Group (AMLCG-1999) and compared this group to 386 pts without +13 who were classified in the ELN Intermediate-II genetic category. All pts received intensive induction chemotherapy. There was no significant difference in age, white blood cell or platelet count between the two groups. However, LDH levels were significantly (p=.01) lower in the AML+13 group while bone marrow blast percentage was significantly higher (p=.04). Twelve AML+13 pts (52%) reached complete remission, but all relapsed. Relapse-free and overall survival were inferior in the AML+13 group compared to other ELN Intermediate-II pts (median RFS, 9 vs 15 months, p=.01; median OS, 7 vs. 13 months, p=.03).
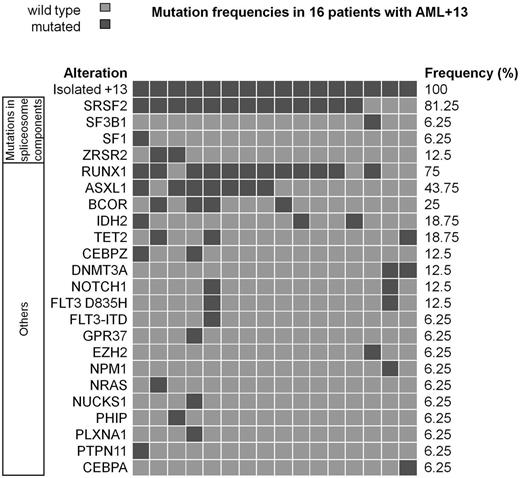
Remission samples from two AML+13 pts were available as normal control for exome sequencing. Using SureSelect human all exon target enrichment (Agilent) followed by 80bp paired-end sequencing on an Illumina GAIIx platform, we were able to identify non-synonymous leukemia-specific mutations affecting, among others, RUNX1, ASXL1, PTPN11 and CEBPZ.
To further characterize this genetically homogenous subgroup, we compared gene expression profiles of 9 pts with AML+13 with 509 AML pts without +13. We identified 678 (up-regulated 492; down-regulated 186) probe sets as significantly deregulated. Only 59 (8.7%) of these probe sets were localized on chr 13, but of those, 55 were up-regulated and only 4 were down-regulated. Up-regulated probe sets on chr 13 included FOXO1, FLT3 and RB1. The strongest down-regulated probe set on chr 13 belonged to the tumor suppressor gene SPRY2, which is a negative regulator of receptor tyrosine kinases. Gene set enrichment analysis showed significant deregulation of gene sets associated with regulation of transcription and nuclear transport.
In summary, our study is the first to show that AML+13 is significantly associated with inferior OS and RFS compared to other intermediate-risk cytogenetic abnormalities in a homogeneously treated cohort. Furthermore, we present evidence that AML+13 leukemias are a genetically quite homogenous subgroup. AML+13 is not only associated with a high rate of RUNX1 mutations but also with mutations in SRFS2, ASXL1 and BCOR. The incidence of mutations in SRSF2 in AML+13 is the highest of any AML subgroup reported so far. In addition, our gene expression data show a homogenous expression profile associated with AML+13. The striking association of a few recurring mutations in AML+13 suggests a biological relationship with synergistic lesions during leukemogenesis. While mutations in RUNX1, ASXL1 and up-regulation of FLT3 were previously reported as markers of poor prognosis in AML, the combination of these lesions might be responsible for the extremely poor outcome of AML+13.
Krebs:Illumina: Honoraria. Greif:Illumina: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal