Abstract
To elucidate the role of retinoic acid (RA) in anti-CD40 + interleukin-4 (IL-4)–mediated B-cell activation, the effect of 10−12 to 10−6 mol/L RA was studied in anti-CD40 (1 μg/mL) + IL-4 (5 ng/mL)-mediated proliferation and Ig synthesis by human peripheral blood mononuclear cells (PBMC) and B cells in healthy donors. Anti-CD40 + IL-4–mediated proliferation of PBMC and B cells was inhibited by RA in a dose-dependent manner, with maximal inhibition of 62% ± 5% in PBMC and 55% ± 4.4% in B cells by all-trans RA, and 58% ± 6.7% and 51% ± 4.7%, respectively by 13-cis RA. IgE synthesis was even more markedly inhibited by RA starting at concentrations of >10−14mol/L for B cells and >10−10 mol/L for PBMC. Maximal inhibition of IgE production for B cells was at 10−8mol/L for all-trans RA (94% ± 1.8%) and 96% ± 3.2% for 13-cis RA. Low concentrations of RA inhibiting IgE synthesis (10−10 mol/L) affected neither B-cell proliferation nor the production of IgA, IgG, and IgM. Elucidation of the mechanism involved in this inhibition of IgE production shows that epsilon germline transcription is decreased by RA, whereas production of interferon-γ (IFN-γ) was not enhanced in the presence of RA. To differentiate whether the RA effect was mediated by RA receptors , β, and γ, the expression of the retinoic acid receptors (RAR) was examined by reverse transcriptase-polymerase chain reaction (RT-PCR). The data show that unstimulated human peripheral B cells express mRNA of the RA receptor , β, and γ. Using retinoids with different receptor binding specificity (CD336, CD437, CD2019, CD367), dose-dependent inhibition of IgE synthesis was shown by all four derivates, but was most marked by an RA binding the receptor with high specificity. Taken together, this study shows that RA inhibits IgE production of anti-CD40 + IL-4–stimulated B cells in vitro.
© 1998 by The American Society of Hematology.
RETINOIDS ARE DERIVED from vitamin A and are widely used in the treatment of dermatologic disorders such as acne and psoriasis.1 Their biologic effects include the regulation of growth and differentiation in a number of cell types primarily of epithelial bone marrow origin. Recently, retinol and retinoic acid (RA) have also been shown to inhibit proliferation of isolated mature and precursor B cells from normal donors after mitogenic stimulation.2 The role of RA on CD40 + interleukin-4 (IL-4)–mediated IgE synthesis has, however, not yet been studied.
Stimulation of human B cells by anti-CD40 + IL-4 results in proliferation and IgE production.3,4 Class switching factors such as IL-4 induce expression of the germline transcript of the Cε gene, which maintains an open chromatin structure in this region. The activation of CD40 results in the induction of the class switching machinery for S-S recombination.5 Interaction between CD40 on B cells and CD40L on T cells is critical for T-cell–dependent isotype switching, because it has been shown that disruption of the CD40L gene causes X-chromosome-linked immune deficiency, characterized by decreased serum IgA, IgG and IgE levels.6 Anti-CD40 monoclonal antibody (MoAb) mimic the effect of CD40L and anti-CD40 MoAb plus IL-4 induce IgE production in vitro. CD40 + IL-4–mediated IgE production can be inhibited by various cytokines including interferon-γ (IFN-γ), IL-8, IL-10, and IL-12 and by various other factors such as hormones.7-9
In search of molecules that might induce a therapeutic downregulation of IgE synthesis, which is considered to be a basic effect in atopic diseases, we have chosen here to study the effects of RA on CD40 + IL-4–mediated B-cell activation including IgE production. The present data show for the first time that RA induces a dose-dependent, selective inhibition of CD40 + IL-4–mediated proliferation and even more reduction of IgE production by human peripheral B lymphocytes, with the latter acting at the level of epsilon germline transcription most likely via retinoic acid receptor (RAR)α.
MATERIALS AND METHODS
Cells.
Peripheral blood mononuclear cells (PBMC) were isolated from buffy coats of nonallergic healthy donors by ficoll hypaque separation (1,400 rpm, 30 minutes, room temperature). B cells were purified using anti-CD19–coupled magnetic beads (Dianova, Hamburg, Germany). Briefly, cells and antibody-conjugated beads (1:5 ratio) were incubated for 1 hour on ice, then CD19-positive B cells were selected by magnetic separation and after several washings the cells were resuspended in medium and cultured overnight at 37°C. The next morning, cells were separated from the beads by several washings and counted. The purified cell population contained more than 95% B cells, as assessed by immunofluorescence with anti-CD20 antibody. In previous studies, this procedure has been shown not to activate B cells.10CD19/IgM double-positive PBMC were sorted according to the instructions of the manufacturer (Miltenyi Biotec, Bergisch-Gladbach, Germany) by magnetic cell sorting (MACS) with the CD19 Multi Sort Kit. Briefly, PBMC were enriched using anti-CD19 magnetic beads in combination with a VS separation column. After release of the magnetic label, CD19 positive cells were sorted according to the expression of IgM (VS separation column). All reagents were obtained from Miltenyi Biotec. For fluorescent staining 105 cells were suspended in 90 μL staining buffer (2% bovine serum albumin [BSA] in phosphate-buffered saline [PBS], pH 7.4, 0.1% sodium azide) with 10 μL of the appropiate antibody and incubated for 30 minutes on ice. After several washings, cells were fixed in 2% paraformaldehyde, when the biotinylated MoAb was used, cells were incubated for another 30 minutes with streptavidin-conjugated phycoerythrin (PE) before fixation.
Cells (105 cells/well) were cultured for 3 days for proliferation and 10 days for IgE assays. The culture medium RPMI 1640 was supplemented with L-glutamine (2 mmol/L), penicillin (100 U/mL), streptomycin (100 mg/mL) and 10% heat inactivated fetal calf serum (all from Biochrom KG, Berlin, Germany). All cell cultures were performed at 37°C in humidified air and 5% CO2atmosphere.
Reagents.
IL-4 was purchased from Pharmingen (Hamburg, Germany), purified anti-CD40 MoAb (clone 626.1) was a kind gift from R. Geha (Children’s Hospital, Boston, MA), and RA (all-trans and 13-cis) were from Sigma (St Louis, MO). Stock solutions (10−3mol/L) of retinoids were prepared in dimethyl sulfoxide (DMSO). Receptor-specific retinoids were kindly provided by U. Reichert (CIRD Galderma, France). The conjugated anti-CD19-PE, anti-IgM–fluorescein isothiocyanate (FITC), the conjugated isotype controls, and streptavidin-PE were from Pharmingen (Hamburg, Germany).
Proliferation assay.
For proliferation assay, radioactive thymidine (0.5 μCi per well) was added during the last 16 hours of culture. Cells were harvested on filter paper and thymidine incorporation was measured using liquid scintillation spectroscopy. All experiments were performed in triplicate and data expressed as arithmetric means.
Ig production.
Cells were cultured for 10 days, and Igs were measured in the supernatants of stimulated cells by enzyme-linked immunosorbent assay (ELISA). The MoAb for IgE detection (clones HP 6061 and HP 6029) were kindly provided by Bob Hamilton (Asthma and Allergy Center, Johns Hopkins University, Baltimore, MD). The antibodies for IgA, IgG, and IgM ELISA (anti-IgA, anti-IgG, and anti-IgM) were purchased from Dianova (Hamburg, Germany).
Briefly, for the Ig assays, immunoplates (Nunc, Wiesbaden, Germany) were coated overnight at 4°C with anti-human Ig-Fc antibodies diluted in 0.1 mol/L bicarbonate buffer. The wells were then blocked for 1 hour with 2% BSA-Tris buffer. After several washings, supernatants and internal standards were incubated in duplicates overnight. The next morning, after several washes, the second alkaline phosphatase (AP)-conjugated anti-Ig (A; G; M) antibody was added. Because the second anti-IgE MoAb was biotinylated, cells were incubated for another hour with alkaline phosphatase-conjugated streptavidin. After the final reaction with phosphatase substrate (Sigma, Dreieich, Germany), plates were read in a microplate ELISA reader at 410 nm, and the amount of Ig was calculated according to the standard curve. The variations of readings in duplicate cultures never exceeded 15%.
Polymerase chain reaction (PCR).
Semiquantitative reverse transcriptase (RT)-PCR was used for detection of RAR-α-β-γ) and epsilon germline transcription. Total cellular RNA was extracted from purified B cells with an RNA preparation kit (Quiagen, Hilden, Germany). The mRNA was quantified and reverse-transcribed into cDNA by RT (Boehringer, Mannheim, Germany). PCR amplification was performed with RAR-specific11 and epsilon germline specific primers.12 Primers used for detection of RAR α were tgg gtg gac tct ccc cgc ca for sense and ccc acc tcc ggc gtc agc gtg for antisense resulting in a 438-bp fragment, for RAR beta 5′ cac tgg ctt gac cat cgc aga cc and 3′ gag agg tgg cat tga tcc agg resulting in an 435-bp fragment and for RAR gamma sense ggc ctg ggc cag cct gac ctc and antisense cag ccc cag atc cag ctg cac g resulting in a 515-bp fragment. PCR was performed using the following program: 30 cycles (1 minute at each 94°C, 65°C, and 74°C).
Epsilon germline specific primers were sense (GACGGGCCACACCAT CCACAGGCACCAAATGGACGAC) of the I epsilon exon and antisense (CAGGACGACTGTAAGATCTTCACG) of the Cε 2 exon resulting in a 409-bp band. As a control, a 250-bp band corresponding to glyceraldehyde-3-phosphate dehydrogenase (GAPDH) transcripts was amplified using GATGACATCAAGAAGGTGGTG for sense and GCTGTAGCCAAATTCGTTGTC for antisense. PCR was performed with a Perkin Elmer (Branchburg, NJ) thermocycler using the following program: 35 cycles (1 minute at each 94°C, 65°C, and 74°C) for epsilon germline transcripts and for 25 cycles (1 minute each at 94°C, 57°C, and 74°C) for the GAPDH control.
RESULTS
RA inhibits CD40 + IL-4–mediated cell proliferation.
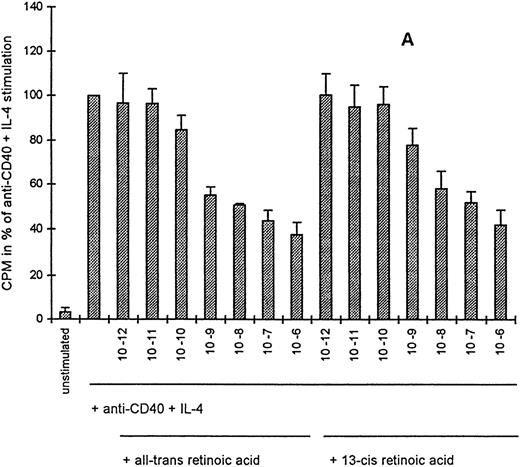
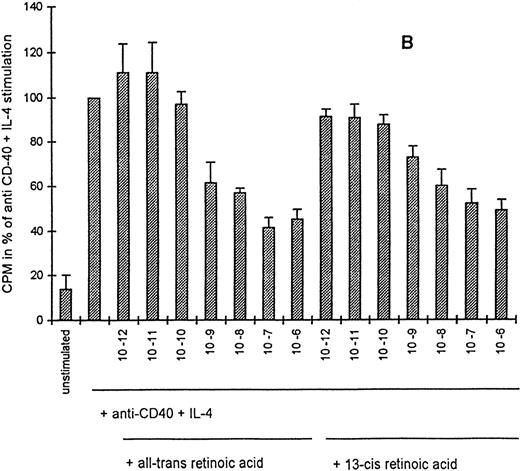
To study the role of RA in CD40 + IL-4–mediated cell activation, we used different concentrations of all-trans RA and its 13-cis isomer (10−12 to 10−6 mol/L) in the presence of anti-CD40 + IL-4. A dose-dependent inhibition with both RA derivates of CD40 + IL-4–mediated PBMC proliferation was observed. For quantification of the antiproliferative effect on CD40 + IL-4–stimulated cells, mean values of stimulated cells were set at 100%. A 62% ± 5.2% maximal inhibition of PBMC proliferation was observed at 10−6 mol/L by all trans retinoic acid and a 58% ± 6.3% maximal inhibition by 10-6 mol/L 13-cisretinoic acid (Fig 1A).
Inhibition of CD40 + IL-4–mediated cell proliferation by all-trans and 13-cis RA. Proliferation of PBMC (A) and purified peripheral B cells (B) induced by anti-CD40 + IL-4 (1 μg/mL and 5 ng/mL) and anti-CD40 + IL-4 + all-trans RA or 13-cis RA (10−12 to 10−6 mol/L). Cells (106/mL) were incubated for 3 days, and thymidine (0.5 μCi) was added for the last 16 hours of culture to each well. Each experiment was done in triplicate, the cpm values of unstimulated cells were <500 cpm and ranged after anti-CD40 + IL-4 stimulation from 20,000 to 30,000 cpm for PBMC and 10,000 to 20,000 for the B cells. Anti-CD40 + IL-4 stimulation was set at 100% and mean values of four experiments + standard error of mean (SEM) are shown.
Inhibition of CD40 + IL-4–mediated cell proliferation by all-trans and 13-cis RA. Proliferation of PBMC (A) and purified peripheral B cells (B) induced by anti-CD40 + IL-4 (1 μg/mL and 5 ng/mL) and anti-CD40 + IL-4 + all-trans RA or 13-cis RA (10−12 to 10−6 mol/L). Cells (106/mL) were incubated for 3 days, and thymidine (0.5 μCi) was added for the last 16 hours of culture to each well. Each experiment was done in triplicate, the cpm values of unstimulated cells were <500 cpm and ranged after anti-CD40 + IL-4 stimulation from 20,000 to 30,000 cpm for PBMC and 10,000 to 20,000 for the B cells. Anti-CD40 + IL-4 stimulation was set at 100% and mean values of four experiments + standard error of mean (SEM) are shown.
Because the inhibition of CD40 + IL-4–mediated cell proliferation might be mediated either through direct effects on B cells or through indirect effects, eg, via increased cytokine production by cells other than B cells, we examined next the effects of all-trans and 13-cis RA on CD40 + IL-4–mediated B-cell proliferation. The pattern of inhibition with B cells was comparable to that observed with PBMC, with a 55% ± 4.4% maximal inhibition of CD40 + IL-4–mediated B-cell proliferation for all-trans RA and 51 ± 4.7 for 13-cis RA, both at 10−6 mol/L (Fig 1B). Incubation of the cells with RA alone caused, on the other hand, no proliferative effects on PBMC or B cells (data not shown).
RA inhibits CD40 + IL-4–mediated IgE production.
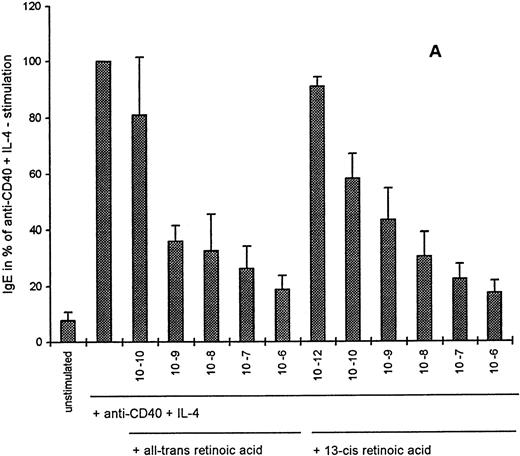
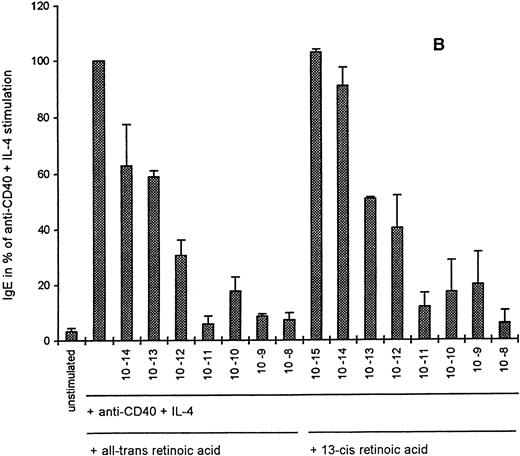
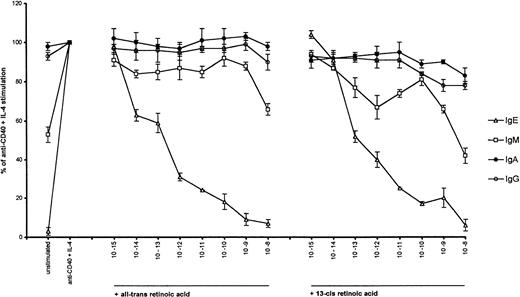
Because stimulation of B cells with anti-CD40 + IL-4 results not only in proliferation, but also in IgE production, we examined the effects of RA on CD40 + IL-4–mediated IgE-synthesis. Figure 2 shows that in the presence of all-trans and 13-cis RA, CD40 + IL-4–mediated IgE production was inhibited in a dose-dependent manner in both PBMC and CD19+ B cells. In PBMC, maximal inhibition of IgE was 81% ± 8% for all-trans RA and 82% ± 11.4% for 13-cis RA, both at 10-6 mol/L (Fig 2A), and with B cells, inhibition of IgE production even reached control levels of 94% ± 1.8% and 96% ± 3.2%, respectively, at 10−8 mol/L (Fig 2B). Interestingly, inhibition of IgE production in the B cells was observed already at very low concentrations of RA (10−14 mol/L), indicating a specific effect on IgE production rather than on inhibition of cell proliferation. To provide further evidence that RA is not just affecting the synthesis of IgE from previously switched B cells, we used double separated CD19-IgM+ cells (Fig 3). The data show (Table 1) that inhibition of IgE synthesis after anti-CD40 + IL-4 stimulation by all-trans and 13-cis RA was also observed in double-purified CD19-IgM+ B cells.
Retinoids inhibit the IgE-production of anti-CD40 + IL-4–stimulated human PBMC (A) and B cells (B) from normal donors. PBMC and B cells (106/mL) were incubated for 10 days in the presence of CD40 + IL-4 (1 μg/mL and 5 ng/mL) alone or in combination with all-trans RA (10−10 to 10−6 mol/L for PBMC and 10−14 to 10−8 mol/L for B cells) or 13-cis RA (10−12 to 10−6 mol/L for PBMC and 10−15 to 10−8 mol/L for B cells). IgE (pg/mL) was detected in the supernatants by ELISA, IgE in unstimulated PBMC and B cells was below 200 pg/mL and ranged after anti-CD40 + IL-4 stimulation from 2,204 to 12,846 pg/mL in PBMC and from 2,250 to 2,951 pg/mL in B cells. Values are expressed as percent of anti-CD40 + IL-4 stimulation and mean values of four experiments + SEM are shown.
Retinoids inhibit the IgE-production of anti-CD40 + IL-4–stimulated human PBMC (A) and B cells (B) from normal donors. PBMC and B cells (106/mL) were incubated for 10 days in the presence of CD40 + IL-4 (1 μg/mL and 5 ng/mL) alone or in combination with all-trans RA (10−10 to 10−6 mol/L for PBMC and 10−14 to 10−8 mol/L for B cells) or 13-cis RA (10−12 to 10−6 mol/L for PBMC and 10−15 to 10−8 mol/L for B cells). IgE (pg/mL) was detected in the supernatants by ELISA, IgE in unstimulated PBMC and B cells was below 200 pg/mL and ranged after anti-CD40 + IL-4 stimulation from 2,204 to 12,846 pg/mL in PBMC and from 2,250 to 2,951 pg/mL in B cells. Values are expressed as percent of anti-CD40 + IL-4 stimulation and mean values of four experiments + SEM are shown.
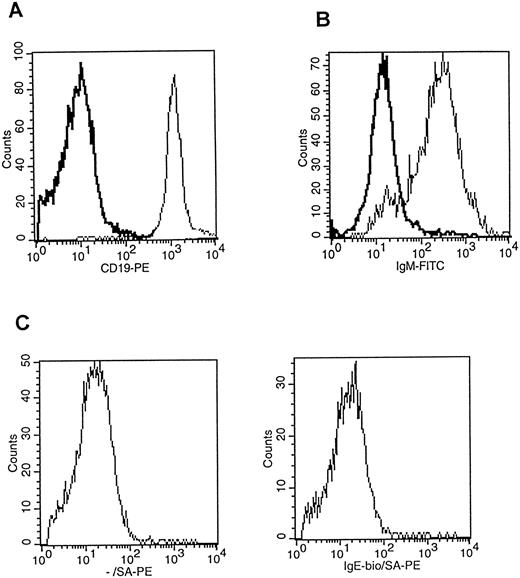
Flow cytometric analysis of purified peripheral B cells from a nonallergic donor. (A) 105 B cells stained with anti-CD19-PE (light black line) and its isotype control-PE (bold black line) after anti-CD19 separation. The percentage of purified CD19+ cells was 96.5%. (B) CD19+ cells after anti-IgM–selection staining with fluorescein conjugated anti-IgM (light black line) and its fluorescein-conjugated isotype control (bold black line). The percentage of purified IgM+ cells was 86%. (C) Shows staining of CD19 IgM-selected B cells with a biotinylated anti-IgE (2 μg/mL, HP6029) and its appropiate biotinylated isotype control in the same concentration by using streptavidin-conjugated PE as a secondary reagent. IgE+cells were not detectable. As a positive control, cells from an allergic donor were stained (data not shown).
Flow cytometric analysis of purified peripheral B cells from a nonallergic donor. (A) 105 B cells stained with anti-CD19-PE (light black line) and its isotype control-PE (bold black line) after anti-CD19 separation. The percentage of purified CD19+ cells was 96.5%. (B) CD19+ cells after anti-IgM–selection staining with fluorescein conjugated anti-IgM (light black line) and its fluorescein-conjugated isotype control (bold black line). The percentage of purified IgM+ cells was 86%. (C) Shows staining of CD19 IgM-selected B cells with a biotinylated anti-IgE (2 μg/mL, HP6029) and its appropiate biotinylated isotype control in the same concentration by using streptavidin-conjugated PE as a secondary reagent. IgE+cells were not detectable. As a positive control, cells from an allergic donor were stained (data not shown).
RA does not affect IgA and IgG production.
To determine whether the inhibition of IgE production was accompanied by inhibition of the production of other Igs, we measured the production of IgA, IgG, and IgM in the supernatants of CD40 + IL-4–stimulated CD19+ cells. As shown in Fig 4, all-trans and 13-cisRA had hardly any effect on IgA or IgG production. RA concentrations with greater than 50% inhibition of IgE production failed to affect IgA or IgG production indicating a more selective effect of RA on IgE production. This finding was further confirmed by using CD19-IgM+ B cells in which induction of IgA and IgG production after stimulation with anti-CD40 + IL-4 was detected and, which was not inhibitd in the presence of all-trans or 13-cis RA (Table 1). Because stimulation of B cells with anti-CD40 + IL-4 results not only in IgE, but also IgM production, we also examined the effects of all-trans and 13-cis RA on anti-CD40 + IL-4–induced IgM production. All-trans RA caused a modest inhibition of IgM production in CD40 + IL-4–stimulated B cells, whereas 13-cis RA resulted in a more marked dose-dependent inhibition of IgM production (Fig 4), but only at higher RA concentrations (10−9 and 10−8). However, the maximal inhibition of IgM production was significantly lower compared with the inhibition of IgE production.
Effect of all-trans and 13-cis retinoic acid on Ig production by human B cells. Experiments were performed as described in Fig 2. Igs (IgA, IgG, and IgM) were detected in the supernatants by ELISA using the appropriate MoAb. Values are shown as means percent of CD40 + IL-4 stimulation (n = 3).
Effect of all-trans and 13-cis retinoic acid on Ig production by human B cells. Experiments were performed as described in Fig 2. Igs (IgA, IgG, and IgM) were detected in the supernatants by ELISA using the appropriate MoAb. Values are shown as means percent of CD40 + IL-4 stimulation (n = 3).
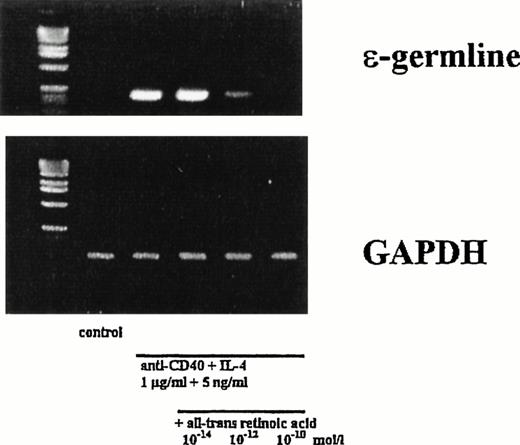
RA inhibits epsilon germline transcription.
Production of epsilon germline transcription is a prerequisite for the isotype switching to IgE.13 To examine whether RA-mediated inhibition of IgE production occurs directly at this level, we studied the expression of germline Cε transcripts semiquantitatively by RT-PCR. The specificity of the germline transcripts was confirmed by obtaining PCR products of the expected molecular size, by its expression pattern, and by direct partial sequencing. A representative result of three experiments is shown in Fig5. As a control, GAPDH expression was assessed for equal amounts of cDNA. Levels of epsilon germline transcription were increased after stimulation with anti-CD40 + IL4 for 4 days. In the presence of both RA derivates (all-trans and 13-cis RA), a dose-dependent inhibition of epsilon germline transcription was observed (shown for all-trans-RA in Fig 5). In agreement with the inhibition of IgE levels at RA concentrations tested (Fig 2), there was a marked inhibition of epsilon germline transcription at 10−10mol/L of all-trans RA, as assessed by semiquantitative evaluation. This indicates that RA inhibits IgE production affecting epsilon germline transcription in CD40 + IL-4–stimulated B cells.
Retinoic acid downregulates CD40 + IL-4–mediated epsilon germline transcription. Human peripheral B cells were stimulated for 4 days in the presence of anti-CD40 + IL-4 (1 μg/mL and 5 ng/mL), respectively, alone or in combination with all-trans RA (10−14, 10−12, 10−10 mol/L). Thereafter, mRNA was extracted. C germline and GAPDH transcripts were assessed by semiquantitative RT-PCR.
Retinoic acid downregulates CD40 + IL-4–mediated epsilon germline transcription. Human peripheral B cells were stimulated for 4 days in the presence of anti-CD40 + IL-4 (1 μg/mL and 5 ng/mL), respectively, alone or in combination with all-trans RA (10−14, 10−12, 10−10 mol/L). Thereafter, mRNA was extracted. C germline and GAPDH transcripts were assessed by semiquantitative RT-PCR.
Inhibition of IgE production is IFN-γ independent.
To explore possible mechanisms involved in RA-induced inhibition of epsilon germline transcription and because IFN-γ is known to inhibit IgE production,14 we examined next whether the production of this cytokine is increased in the presence of RA. PBMC and B cells from normal donors were stimulated with anti-CD40 + IL-4 alone or in the presence of RA. As shown in Table 2, baseline IFN-γ production of unstimulated cells is low and highly variable. In the presence of both RA, the amounts of IFN-γ were rather decreased in the supernatants of CD40 + IL-4–stimulated PBMC and B cells. However, neither all-trans nor 13-cis RA significantly enhanced the production of IFN-γ, indicating that inhibition of IgE synthesis by both RA derivatives involves mechanisms other than IFN-γ.
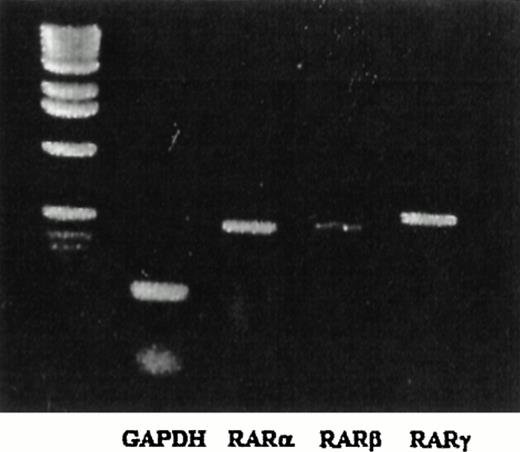
Expression of retinoic acid receptors on human B cells.
The biological effects of RA are exerted through binding the RARα, β, and γ. To determine the expression of the different RAR in unstimulated peripheral B cells, semiquantitative PCR analysis was performed by using RARα, β, and γ specific primers. Transcripts for the RARα, β, and γ, were detectable in unstimulated peripheral human B cells by RT-PCR (Fig 6). As a positive control, primers for RARα, β, and γ were used in a monocytic cell line (THP-1), which has been shown to express all three RAR (M. Babina, personal communication, November 1997).
Expression of RAR in peripheral human B cells. Human peripheral B cells were isolated and mRNA was extracted. RAR-specific (, β, and γ) and GADPH transcripts were assessed by semiquantitative RT-PCR. The DNA ladder is shown in the left lane.
Expression of RAR in peripheral human B cells. Human peripheral B cells were isolated and mRNA was extracted. RAR-specific (, β, and γ) and GADPH transcripts were assessed by semiquantitative RT-PCR. The DNA ladder is shown in the left lane.
Effects of receptor-specific retinoids on CD40 + IL-4–mediated IgE production.
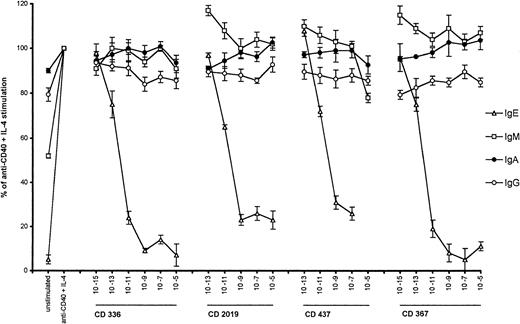
The role of the different RAR during IgE production was determined next by using derivates of RA with different affinity toward the RARα, β, and γ. The molecular weights, their receptor specificity and their transcriptional activation values after binding the particular receptor indicating the intracellular activity of the four retinoids studied are summarized in Table 3. As shown in Table 4, all compounds were inhibitory, but those binding RARα with high-affinity did so by greater than 80% at concentrations of >10−11mol/L. These findings were further confirmed by the observation that ε germline transcription of CD40 + IL-4–stimulated cells was only inhibited at concentrations above 10−12 mol/L in the presence of CD336 and CD367, derivates of RA with high affinity toward the RARα (data not shown). Analysis of IgA, IgG, and IgM production in the presence of the RAR-specific compounds showed that the production of these Igs was not altered (Table 1, Fig 7), confirming the specificity by which RA inhibits CD40 + IL-4–mediated IgE production.
Effect of different RAR-specific retinoids on Ig production by human B cells. Experiments were performed as described in Fig 2. Igs (IgA, IgG, and IgM) were detected in the supernatants by ELISA using the appropriate MoAb. Values are shown as means percent of CD40 + IL-4 stimulation (n = 3).
Effect of different RAR-specific retinoids on Ig production by human B cells. Experiments were performed as described in Fig 2. Igs (IgA, IgG, and IgM) were detected in the supernatants by ELISA using the appropriate MoAb. Values are shown as means percent of CD40 + IL-4 stimulation (n = 3).
DISCUSSION
In the present report, we demonstrate that all-trans and 13-cis RA affects CD40 + IL-4–mediated B-cell activation by inhibition of B-cell proliferation and IgE synthesis. Using RAR-specific RA derivates, we elucidated that these effects are primarily mediated via the nuclear RARα. Because the physiologic level of all-trans RA in serum is about 10 nmol/L15and because the inhibition of DNA synthesis elicited by all-trans-RA at this concentration was 50% in PBMC and 58% in B cells after CD40 + IL-4 stimulation and because IgE synthesis was even affected at a concentration of 10−14 mol/L in B cells and 10−10 mol/L in PBMC, marked inhibition of B-cell proliferation and of IgE production must be assumed to be achievable during oral treatment with RA.16
Presumably due to the importance of retinoids in the treatment of hematologic and dermatologic disorders such as leukemia, acne, or psoriasis, the focus of past studies has been on the role of retinoids in the growth and differentiation of myeloid cells and keratinocytes.17,18 However, vitamin A has been shown to be a key regulator for cell growth, cytokine production, and differentiation in normal B cells.19,20 The growth inhibiting effects of retinoids on B lymphoid cells have been noticed previously using cell lines at different stages of maturation.2 Despite the dramatic effects of vitamin A deficiency on the immune system in vivo,21 and the role of RA on B-cell growth and differentiation in vitro,19 20 no information about the effects of RA on CD40 + IL-4–mediated isotype switching and Ig synthesis in human B cells is available.
The majority of in vivo experiments dealing with vitamin A and the immune system have concluded that vitamin A has a stimulatory role on cells of the immune system.21 This assumption is based on deficiency studies in animal models, epidemiologic data from humans, as well as data on supplementation of retinoids showing reduced infections in humans. In vitro experiments using isolated lymphocytes have shown divergent effects. Both stimulatory and inhibitory effects of retinoids on B lymphocytes have been observed.19,22 However, more recent studies have clearly shown that RA inhibits mitogenic activation of human and murine B cells,2 in line with the present results.
Induction of IgE synthesis requires two signals and has been shown to be induced by the cytokine IL-4 and engagement of the B-cell antigen CD40.4 No data about the role of RA in CD40 + IL-4–mediated IgE production are available to date. However, in a previous study using an in vivo mouse model, an increased IgE response after ovalbumin (OvA) sensitization has been demonstrated in RA-pretreated mice.23 In contrast to these findings, we show here that CD40 + IL-4–mediated IgE production is strongly inhibited by RA in a dose-dependent manner. Inhibition of IgE synthesis occurs at very low concentrations (down to 10−12mol/L), which are easily achieved in the serum during retinoid treatment. The observation that while, in cultures of purified B cells, the concentration of RA required for inhibition of IgE synthesis is substantially lower than for proliferation is not the case in PBMC, suggests that additional factors, eg, cytokines other than IFN-γ, may prevent the RA susceptibility of IgE synthesis.
Inhibition of in vitro IgE production has also been reported with all-trans RA by Tokuyama et al24 in the murine system. These investigators used IL-4 + hydrocortisone-stimulated splenic B cells from mice and detected a dose-dependent inhibition of IgE production in the presence of RA. We show here for the first time an inhibition of CD40 + IL-4–induced IgE production in human peripheral B cells. Furthermore, we demonstrate inhibition of epsilon germline transcription by RA suggesting thus a molecular mechanism of RA dependent inhibition of IgE production. Epsilon germline transcription is a prerequisite for the induction of IgE isotype switching, because deletion of the I exon in mice results in significant impairment of IgE production.25 Therefore, inhibition of epsilon germline transcription by RA may play an important role in the regulation of IgE production after CD40 + IL-4 stimulation in vivo.
That RA is capable of affecting Ig production in mice has been shown in other studies. The effects of RA on B cells seems to depend on the model or the type of stimulation used since in lipopolysaccharide (LPS)-stimulated splenic B cells, enhancement of germline C α transcripts was determined, while on the other hand, IL-4–induced I γ expression was completely abolished in the presence of RA.26 Taken together, the currently available data strongly support the concept that RA is capable of modulating Ig production significantly even at the level of isotype switching. However, this does not exclude the possibility that other mechanisms are operative in addition, possibly via the action of cytokines.
A variety of cytokines including tumor necrosis factor-α (TNF-α), IL-5, IL-6, IL-8, IL-10, IL-12, and transforming growth factor-β (TGF-β) have been shown to modulate IgE production.27Because IFN-γ has been shown to inhibit IgE production,28we studied the production of IFN-γ in the presence of RA. The lack of any enhancing effects of RA on the production of IFN-γ suggests that inhibition of IgE production is IFN-γ independent. The observation that IgE synthesis in B cells was more inhibited than in PBMC where IFN-γ production is produced by monocytes or TH1 cells also speaks against a role of IFN-γ in the in vitro data observed with RA. Another cytokine that may be involved in the inhibition of IgE-production by RA is TGF-β. This cytokine has been shown to be induced by RA in keratinocytes.29 TGF-β is a potent immunosuppressive cytokine and has also been shown to inhibit IgE and epsilon germline transcription in vitro.30 Whether TGF-β production is increased in the presence of RA in PBMC or B cells is currently under investigation. However, a study by Tokuyama et al31 has shown a TGF-β independent modulation of germline transcription in LPS/IL-4–stimulated mouse B cells. At the molecular level, retinoids bind to and activate specific nuclear receptors, the RARs and retinoic X receptors (RXRs). These recognize specific DNA sequences as homo- or heterodimers, which in turn, bind specific DNA sequences regulating gene expression.32 Whether RA binding proteins can directly interact with the epsilon germline promoter region is an interesting possibility that will have to be explored in future studies.
ACKNOWLEDGMENT
We thank R. Geha (Department of Immunology, Children’s Hospital, Boston, MA) for providing the purified anti-CD40 MoAb and Dr R. Hamillton (Asthma and Allergy Center, Baltimore, MD) for providing the anti-IgE MoAb, Dr M. Babina for help with the RAR PCR, and K. Ebermayer for technical assistance. We also thank Prof A. Radbruch (Deutsches Rheuma-Forschungszentrum, Berlin, Germany) for cooperation and support in IgM- B cell purification.
Supported by grants from the German Research Foundation (DFG, Wo 541/2-1) and Hofmann La Roche, Basel, Switzerland.
Address reprint requests to M. Worm, MD, Charité-Virchow Klinikum, Hautklinik, Schumannstr. 20-21, 10117 Berlin, Germany; e-mail: mworm@rz.charite.hu-berlin.de.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.