To the editor:
Atypical hemolytic uremic syndrome (aHUS) is a complement-mediated thrombotic microangiopathy (TMA) characterized by mechanical hemolysis, renal impairment, thrombocytopenia, and preserved ADAM metallopeptidase with thrombospondin type 1 motif 13 (ADAMTS13) function.1,2 Historically, patients with aHUS had poor outcomes, with 5-year end-stage renal disease-free survival of only 36%.3 The use of eculizumab, a monoclonal antibody against the terminal complement component C5, results in improvements in thrombocytopenia, hemolysis, and renal function.4,5
The necessary duration of eculizumab treatment in aHUS is unknown. Before aHUS was distinguished from thrombotic thrombocytopenic purpura, both were treated with plasma therapy, and treatment duration was determined by clinical response.6-8 Emerging evidence suggests aHUS may not require indefinite eculizumab treatment, and cessation may help mitigate sequelae of therapy.9-11 Although the risk for meningococcal infection in immunized patients is low, eculizumab costs $7,696.80/300 mg at our institution, or $800 467 for yearly maintenance; this is in agreement with reports of $723 520 per year by average wholesale price, accounting for the doses used in aHUS.4,12,13 The costs and logistical barriers of prolonged treatment are substantial in resource-rich nations, whereas in other nations, this therapy may not be available because of cost.12,14,15 We examined our institutional experience on eculizumab cessation in adult aHUS to determine benefits and outcomes associated with therapy cessation.
In accordance with institutional review board–approved protocols, adult patients were identified from the Johns Hopkins Complement Associated Disease registry for this single-center, retrospective review.16 Patients were included if they fulfilled aHUS criteria, had negative testing for Shiga toxin when applicable, had ADAMTS13 levels above 10%, and received eculizumab at the discretion of the treating physicians. We report dialysis independence at last follow-up, TMA-event-free status as in Legendre et al,5 and relapse as in Fakhouri et al.10 Detailed methods are reported in the supplemental Appendix, available on the Blood website.
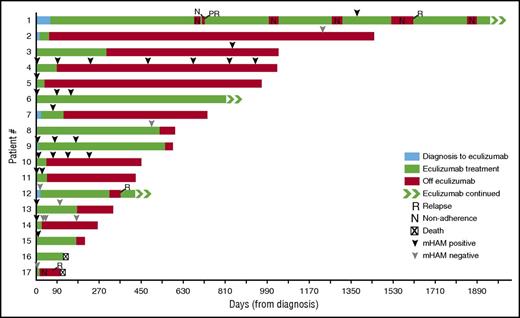
Seventeen patients were treated with eculizumab (Table 1). Patient 14 experienced a prior episode of aHUS at age 7 years and was in remission for 44 years before the event reported here. Median patient age at presentation was 46 years, 76% were female, and 70% were white. Median ADAMTS13 activity was 60% (range, 15%-102%), and admission hemoglobin was 8.3 g/dL (range, 3.3-13.3). Plasma exchange was initiated before eculizumab in 64% of patients, and all patients began eculizumab with active aHUS. Median duration of eculizumab therapy was 90.5 days before physician-directed cessation (range, 14-545 days), and postcessation follow-up was median 308.5 days (range, 33-1390 days). There were no episodes of meningococcal infection. One patient developed bacteremia from an indwelling infusion catheter and was hospitalized. Two patient deaths occurred. Patient 16 died on eculizumab therapy; infected vascular access was suspected, with nonadherence concerns. Patient 17 had eculizumab stopped after 2 induction doses for clinical impression of malignant hypertension-induced TMA, based on severe concentric left ventricular hypertrophy on echocardiogram, history of chronic severe hypertension with antihypertensive nonadherence, and renal biopsy with focal microangiopathic changes consistent with severe hypertension. Patient 17 died of pulseless cardiac arrest during plasmapheresis for relapsed disease after nonadherence to antihypertensive therapy or prearranged medical follow-up. Physician-directed cessation of eculizumab was attempted in patients who achieved complete remission of their TMA and improvement of the putative trigger of their TMA, as outlined in the supplemental Methods. Of the 15 patients who stopped eculizumab with either nonadherence or physician-directed cessation, 3 (20%) experienced relapse (Figure 1). Relapses occurred in the setting of active inflammatory bowel disease, nonadherence to antihypertensives for malignant hypertension, and after liver transplant with medication nonadherence. No patient required resumption of dialysis after cessation. In the 2 patents resuming eculizumab after relapse, platelet count and renal function returned to precessation values. Overall, 94% of all patients achieved TMA-event-free status, and 82% were dialysis-independent at last follow-up.
Clinical remission after eculizumab cessation. Axis origin at aHUS diagnosis. Time from diagnosis to eculizumab therapy indicated in blue, duration of eculizumab therapy indicated in green. Time off eculizumab indicated in red. Nonadherence episode (N), relapse (R), possible relapse (PR), and death (X) indicated. Patients continuing on eculizumab at the time of last follow-up indicated with green arrows. Complement activity as determined by mHam assay is indicated temporally by black arrowheads (positive) and gray arrowheads (negative).
Clinical remission after eculizumab cessation. Axis origin at aHUS diagnosis. Time from diagnosis to eculizumab therapy indicated in blue, duration of eculizumab therapy indicated in green. Time off eculizumab indicated in red. Nonadherence episode (N), relapse (R), possible relapse (PR), and death (X) indicated. Patients continuing on eculizumab at the time of last follow-up indicated with green arrows. Complement activity as determined by mHam assay is indicated temporally by black arrowheads (positive) and gray arrowheads (negative).
Eculizumab cessation obviated 2 induction doses and 422 maintenance doses, with medication savings of $13 038 379 during the study period. Clinician rationale for not attempting cessation included concern for nonadherence with cessation monitoring (patient 6), and liver transplant with prior relapse with medication nonadherence (patient 1). We note that although some patients converted during the course of their illness from positive to negative in the mHam assay of complement activation (patients 13 and 14), others remained persistently positive, despite being in clinical remission off eculizumab (patients 4, 6, 9, and 10). Patients 2 and 8 were negative in the mHAM assay, but samples were obtained distant from the onset of aHUS. Interestingly, both patients 17 and 12 had negative mHAM assays at disease onset, improved with eculizumab, and then experienced relapse after cessation. Because of the small number of relapses and serial mHam assessments, the role of this assay in predicting relapse requires further study; however, ongoing complement activation does not necessarily predict disease relapse.
Mutational and antibody testing did not appear to guide eculizumab cessation. Results of testing were sometimes not available at the time of eculizumab cessation or revealed variants of undetermined significance. In our cohort, 4/17 did not undergo mutational or antibody testing. Two patients had no abnormality identified, and 11/13 had the complement abnormalities shown in Table 1. Although patients with mutations affecting complement components remained in remission after cessation, few harbored aHUS-associated CFH mutations, and none had anti-CFH antibodies.17,18 We observed higher rates of deletions across the CFHR loci (69%) compared with the literature (45%)19 ; however, ADAMTS13 mutations were less frequent in our cohort (23%) than reported previously (80%).20 These mutations are of unclear clinical significance, but may contribute to thrombotic microangiopathy in patients with aHUS.20,21 We highlight that most patients in clinical remission off eculizumab had complement mutations and/or evidence of persistent complement activation. For example, patient 4 has been in clinical remission for 2.6 years, with continued evidence of complement activation in vitro, and harbors homozygous deletion of CFHR3-CFHR1 associated with increased hemolysis in vitro19 and a CFH mutation (Gln950His) previously observed in aHUS22 and predicted to be functionally damaging.23
We show that eculizumab can be safely discontinued in select adult patients with aHUS, despite continued complement activation. Our observed relapse rate (20%) compares favorably to the 31% reported in 2 series,10,24 and 2 of 3 relapses occurred in the setting of nonadherence. Our adult population or the rarity of CFH mutations in our cohort may explain these findings. Although most patients with persistently activated complement and/or complement mutations maintained remission, the adverse outcomes of relapse or death were associated with organ transplantation, active inflammatory conditions, and medical nonadherence. Most patients were amenable to stopping treatment with regular laboratory follow-up, and this approach saved $13 million in drug costs. As delays in eculizumab initiation in aHUS were associated with inferior renal function, a targeted approach of early initiation may minimize long-term renal impairment and maximize independence from dialysis.4 We favor an approach incorporating early eculizumab initiation, continued therapy until patients achieve remission, and then a trial of cessation with regular monitoring. Given the potential risks of eculizumab therapy and its costs, most patients may benefit from a cessation trial when their underlying precipitant illness resolves and/or organ function has improved, but patient adherence is necessary. An alternative approach could be eculizumab frequency reduction based on monitoring complement inhibition.25 Prospective studies will be helpful to identify patients at increased risk for relapse and to elucidate the factors enabling clinical remission despite evidence of continued complement activation in vitro.
The online version of this article contains a data supplement.
Authorship
Acknowledgments: S.A.M. is supported by National Institutes of Health, National Heart, Lung, and Blood Institute hematology fellowship training grant T32 HL007525. This study was supported by National Institutes of Health, National Heart, Lung, and Blood Institute RO1 90069145.
Contribution: S.A.M. designed research, performed research, analyzed data, made figures, and wrote the paper; Z.D.B. and X.Y. performed research; and A.R.M., C.J.S., and R.A.B. designed research and analyzed data.
Conflict-of-interest disclosure: S.A.M. participates on the True North Therapeutics advisory board. C.J.S. receives research funding from Alexion Pharmaceuticals as site principal investigator for the International aHUS registry and is the Chair of the Data Monitoring Committee for the ALXN1210-aHUS-311/312 clinical trial. R.A.B. receives research support from Alexion Pharmaceuticals and Apellis Pharmaceuticals and serves on the advisory boards for Alexion Pharmaceuticals, Achillion Pharmaceuticals, and Apellis Pharmaceuticals. The remaining authors declare no competing financial interests.
Correspondence: Robert A. Brodsky, Division of Hematology, Department of Medicine, Johns Hopkins School of Medicine, 720 Rutland Ave, Ross Room 1025, Baltimore, MD 21205; e-mail: brodsro@jhmi.edu.