Abstract
Introduction: AML pts have a poor prognosis with conventional chemotherapy regimens. Early lymphocyte recovery (ELR) following intensive timed sequential therapy (TST) induction is characterized by a dysfunctional immunosuppressive state. Pomalidomide (Pom), a small molecule immunomodulatory agent (IMiD), has direct effects on T cell co-stimulation by promoting the ubiquitination of Aiolos, an IL-2 transcriptional repressor. We hypothesized that the administration of Pom at the time of ELR after induction TST may influence T cell differentiation and enhance an anti-leukemia immune effect.
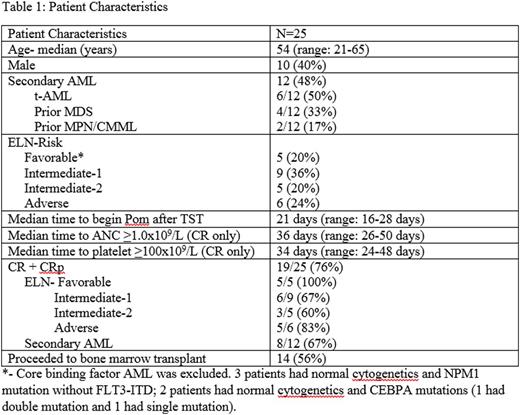
Methods: A multicenter phase 1 dose escalation study was conducted to determine the safety and tolerability of Pom after intensive induction TST in newly diagnosed AML and HR-MDS pts 18-65 years. Core-binding factor AML was excluded. All pts received induction chemotherapy with AcDVP16: cytarabine 667 mg/m2/day IV continuous infusion days 1-3, daunorubicin 45 mg/m2/day IV days 1-3, etoposide 400 mg/m2/day IV days 8-10. Pom was administered at the assigned dose and schedule after day 14 and within 3 days of the total white blood cell count (WBC) reaching >0.2x109/L above nadir, defined as ELR. Three dose levels were planned (2 mg, 4 mg and 8 mg) within 2 cohorts: 10 days of Pom and 21 days of Pom, in a traditional 3+3 dose escalation design.
Results: 25 pts were enrolled on this study January 2014-June 2016 across 3 institutions (Table 1). Pom administration occurred at a median of 21 days after AcDVP16 induction. There were no dose-limiting toxicities (DLTs) in the first cohort of Pom x 10 days within each dose level- 2 mg (n=3), 4 mg (n=3) and 8 mg (n=7). There were no DLTs seen at 4 mg x 21 days (n=7). Two DLTs were seen at Pom 8 mg x 21 days (Grade 3 ALT increase and Grade 3 hypoxia, respectively). Thus, Pom 4 mg x 21 days will be further expanded.
Nine (36%) pts discontinued Pom early (median duration = 5 days) due to: grade 3 rash (n=3), physician discretion (decreased WBC: n=1, fever and increased creatinine: n=1), grade 3 ALT increase (n=1), grade 3 hypoxia (n=1), disease progression (n=1), and pt preference (n=1). Adverse events (AEs) possibly associated with Pom that were seen in >1 pt included fever (n=8), rash (n=7), AST/ALT increase (grade 1: n=4, grade 3: n=1), mucositis (n=2), and fatigue (n=2). All of these AEs were self-limiting with supportive care and/or discontinuation of Pom.
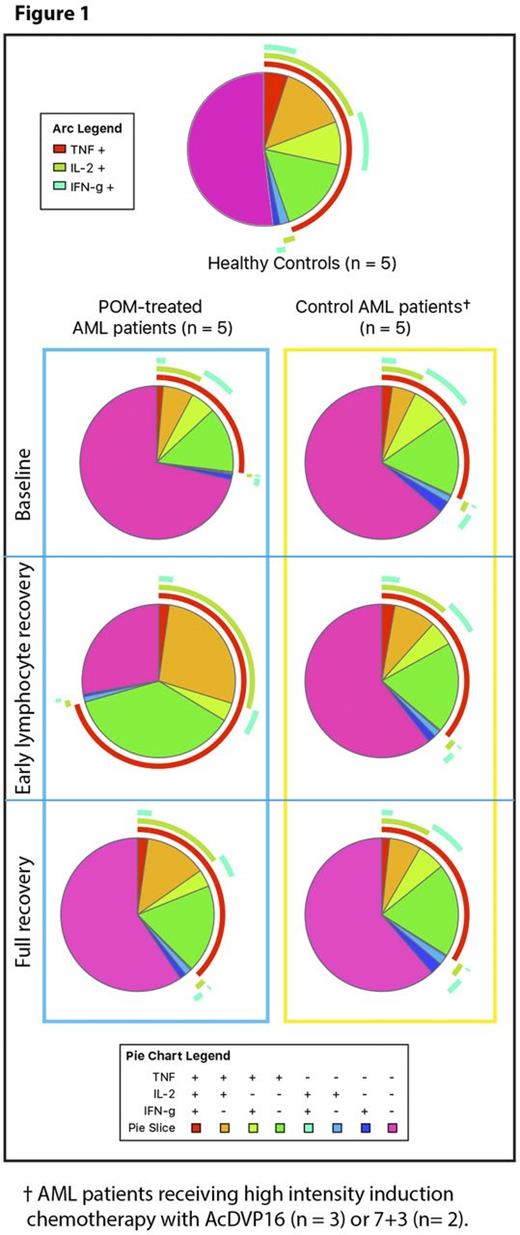
60-day mortality was 0%. A complete remission (CR) was achieved in 18 pts and 1 achieved CR with incomplete platelet recovery (CRp) with a combined CR + CRp = 19/25 (76%). Among pts with adverse-risk AML, 5/6 (83%) achieved CR. One pt achieved a partial remission and 5 pts were refractory to treatment. Of the 19 CRs, 15 had no evidence of minimal residual disease by cytogenetics, FISH, or flow cytometry. Among pts who completed a course of Pom (10 days or 21 days), 14/16 (88%) achieved CR. As previously reported, a dramatic decrease of Aiolos expression via flow cytometry in T cell subsets was observed in vivo for the duration of POM treatment with doses > 2 mg, but the effect was lost after Pom was stopped. Figure 1 displays the pattern of cytokine production of CD4+ T cells visualized with pie charts, and shows a significantly different subset composition at ELR in Pom-treated pts compared to the same pts at full recovery (p=0.02), and compared to control AML pts at the same time point (p=0.004). Furthermore, there was a significant increase in TNF-α production (p=0.009) and the combination of TNF-α and IL-2 production (p=0.03) in stimulated CD4+ T cells during Pom treatment, which was reduced to baseline values after Pom was discontinued at full recovery (Figure 1: data analysis performed with the SPICE software).
Conclusions: Pom can be safely administered at the time of ELR after intensive induction TST. Fever and rash are the most common AEs seen after Pom administration. Inhibition of Aiolos and consequent increase in both IL-2 and TNF-α expression, as measured by flow cytometry, appear to be reliable markers of Pom-induced T cell modulation in vivo. Planned expansion of the cohort of 4 mgx 21 days will allow further evaluation of safety and activity of Pom in AML.
Expression of Cytokines in CD4+ T Cells
Zeidner:Takeda: Research Funding; Merck: Research Funding; Agios: Honoraria; Otsuka: Consultancy; Tolero: Research Funding. Zeidan:Celgene: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Ariad: Consultancy, Honoraria; Incyte: Consultancy, Honoraria. Smith:Celgene: Consultancy, Other: member of DSMB. Levis:Millennium: Consultancy, Research Funding; Daiichi-Sankyo: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Astellas: Consultancy, Honoraria, Research Funding. Foster:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal