Abstract
Introduction: MLL-rearranged (MLL-r) acute leukemia in children is characterized by young age at presentation and a poor overall prognosis despite multi-agent chemotherapy. Aberrant fusion proteins involving the MLL histone methyltransferase (HMT) recruit another HMT, DOT1L, to a multi-protein complex leading to aberrant methylation of histone H3 lysine 79 (H3K79) at MLL target genes. This results in enhanced expression of critical genes for hematopoietic differentiation, including HOXA9 and MEIS1, and has been established as a key mechanism for leukemogenesis in MLL-r leukemias (Krivstov, 2007). Pinometostat is a small molecule inhibitor of DOT1L with sub-nanomolar affinity and >37,000 fold selectivity against non-MLL HMTs. Treatment of MLL-rearranged cells and xenograft models with pinometostat led to reduced histone 3 lysine 79 methylation (H3K79me2), decreased MLL target gene expression and selective leukemia cell kill (Daigle, 2013). Here we report the final results of the pinometostat phase 1 trial in children with relapsed/refractory (R/R) MLL-r acute leukemia.
Methods: An open label dose escalation study of pinometostat was performed in patients (pts) aged 3 months to 18 years (yr) with R/R MLL-r leukemia (NCT02141828). Pinometostat was administered via continuous intravenous infusion (CIV) until disease progression or unacceptable toxicity. Pts were assigned to one of two aged-based dose escalation schemas developed from simulations of pediatric exposures using a previously reported physiologically-based PK (PBPK) model (Waters, 2014). All patients underwent serial collection of PK and peripheral blood mononuclear cells (PBMC). Leukemic blasts were isolated from PBMCs using flow cytometry and quantified for H3K79me2 levels by ChIP-Seq.
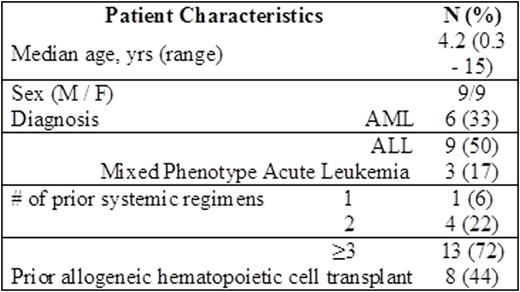
Results: 18 pts were enrolled on study with 9 pts dosed at 70 mg/m2/day and 7 pts at 90 mg/m2/day in the older age cohort (1 to 18 yr) plus 2 pts dosed at 45 mg/m2/day in the younger age cohort (<1 yr).
Grade ≥3 treatment-emergent adverse events (TEAEs) regardless of attribution reported in >20% of pts were: febrile neutropenia; anemia; leukopenia; thrombocytopenia; hypokalemia; respiratory failure; lymphopenia; neutropenia. Drug-related TEAEs reported in >15% of pts were: anemia; thrombocytopenia; leukopenia; rash; lymphopenia; hypocalcemia; hypophosphatemia; neutropenia; ALT elevation; nausea; vomiting.
Dose-limiting toxicities (DLT) were: apnea (70 mg/m2); elevated transaminases (2 at 90 mg/m2) in the >1 year of age cohort, thus defining 70 mg/m2 as the recommended phase 2 dose (RP2D) in older pts. A RP2D was not determined in pts < 1 year of age. Median duration of treatment was 23 days (range 7- 53 days). Pinometostat induced transient decreases in peripheral or marrow leukemic blasts in 7/18 pts, however, these reductions did not meet formal thresholds for objective response.
Adjusted mean plasma pinometostat concentrations during the infusion in children >1 yr at 70 and 90 mg/m2/d doses (1151 ng/mL) was comparable to mean steady-state concentrations observed in adult patients at the 80 mg/m2/d and 90 mg/m2/d doses (1320 ng/mL and 1410 ng/mL, respectively) and was within the range of 1000-1600 ng/mL at 90 mg/m2/d in ≥ 1 yr predicted by earlier PBPK modeling results. CSF concentrations of pinometostat were below the lower limit of quantification of 1 ng/mL (n = 8) or very low (< 12 ng/mL) (n = 4), suggesting negligible CSF exposure. H3K79me2 ChIP-Seq on leukemic blasts demonstrated that pinometostat induced reductions in methylation at MLL-r target genes (e.g. HOXA9 and MEIS1) of ≥ 80 % at all post dose time points (15 and 28 days) and doses (70 & 90 mg/m2) tested consistent with DOT1L inhibition.
Conclusions: In pediatric pts with R/R MLL-r pinometostat has an acceptable safety profile with a RP2D defined as 70 mg/m2 CIV in children > 1 yr. Pinometostat dose/exposure relationships were comparable between adults and children > 1 yr. Pharmacodynamic evidence of DOT1L inhibition was observed in leukemic blasts. Transient reductions in peripheral or bone marrow blasts were detected in ~40 % of pts, however no objective responses were observed. Based on the biological activity observed and evidence of combination benefit of pinometostat with standard of care and novel agents in preclinical MLL-r models (Daigle 2015 and Klaus 2015) further clinical investigation of pinometostat combinations is warranted.
O'Brien:Seattle Genetics: Research Funding; Celgene: Other: travel expenses for required site investigator meeting, October 2015;; steering committee member for pediatric AML trial, Research Funding; Epizyme: Research Funding; Amgen: Other: participated in one pediatric advisory board for blinatumomab in May 2015, paid consultant fee and travel expenses, Research Funding. Blakemore:Epizyme: Employment. Daigle:Epizyme: Employment. Suttle:Epizyme: Employment. Armstrong:Epizyme, Inc: Consultancy; Vitae Pharmaceuticals: Consultancy; Imago Biosciences: Consultancy; Janssen Pharmaceutical: Consultancy. Ho:Epizyme: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal