Key Points
Whole-exome sequencing reveals the presence of recurrent somatic mutations of ETNK1 in patients with atypical chronic myeloid leukemia.
ETNK1 mutations impair the catalytic activity of the enzyme, causing a decrease in the intracellular levels of phosphoethanolamine.
Abstract
Despite the recent identification of recurrent SETBP1 mutations in atypical chronic myeloid leukemia (aCML), a complete description of the somatic lesions responsible for the onset of this disorder is still lacking. To find additional somatic abnormalities in aCML, we performed whole-exome sequencing on 15 aCML cases. In 2 cases (13.3%), we identified somatic missense mutations in the ETNK1 gene. Targeted resequencing on 515 hematological clonal disorders revealed the presence of ETNK1 variants in 6 (8.8%) of 68 aCML and 2 (2.6%) of 77 chronic myelomonocytic leukemia samples. These mutations clustered in a small region of the kinase domain, encoding for H243Y and N244S (1/8 H243Y; 7/8 N244S). They were all heterozygous and present in the dominant clone. The intracellular phosphoethanolamine/phosphocholine ratio was, on average, 5.2-fold lower in ETNK1-mutated samples (P < .05). Similar results were obtained using myeloid TF1 cells transduced with ETNK1 wild type, ETNK1-N244S, and ETNK1-H243Y, where the intracellular phosphoethanolamine/phosphocholine ratio was significantly lower in ETNK1-N244S (0.76 ± 0.07) and ETNK1-H243Y (0.37 ± 0.02) than in ETNK1-WT (1.37 ± 0.32; P = .01 and P = .0008, respectively), suggesting that ETNK1 mutations may inhibit the catalytic activity of the enzyme. In summary, our study shows for the first time the evidence of recurrent somatic ETNK1 mutations in the context of myeloproliferative/myelodysplastic disorders.
Introduction
Atypical chronic myeloid leukemia (aCML) is a clonal disease belonging to the myeloproliferative/myelodysplastic (MPN/MDS) group of hematological disorders according to the World Health Organization 2008 classification.1,2 aCML closely resembles the classical chronic myeloid leukemia, with the main difference being that aCML is invariably negative for any ABL1 rearrangement. The molecular lesions responsible for the onset of aCML remained unknown since 2013, when, by applying whole-exome sequencing, our group demonstrated the presence of recurrent, somatic mutations of the SETBP1 gene, showing that SETBP1 mutations are associated with an increase in white blood cell count and with poor prognosis.3,4 Despite this finding, a complete description of the somatic lesions responsible for the onset of this disorder is still lacking. To identify additional somatic abnormalities occurring in aCML, we extended our previous study to a larger aCML cohort comprising a total of 15 matched cases. The results are described here.
Methods
Patients
Diagnosis of aCML and related diseases was performed according to the World Health Organization 2008 classification.1,2 All patients provided written informed consent, which was approved by the institutional ethics committee. This study was conducted in accordance with the Declaration of Helsinki. Patient samples were processed as previously described.3
Exome sequencing
Genomic DNA (1 μg) was fragmented (500 bp), using a Diagenode Bioruptor Next Gen sonicator and processed according to the standard Illumina protocol. Genomic libraries were enriched for the exonic regions (Illumina TruSeq Exome Enrichment kit) and sequenced on an Illumina Genome Analyzer IIx with 76-bp paired-end reads using Illumina TruSeq chemistry.
RNA sequencing
All RNA libraries were generated from 2 μg total RNA extracted with TRIzol (Life Technologies) following the standard Illumina protocol with minor modifications. Libraries were sequenced on an Illumina Genome Analyzer IIx with 76-bp paired-end reads, using Illumina TruSeq chemistry.
Bioinformatics
Bioinformatic processing has been performed as previously described.3 Sequences and alignments were quality-tested, using SAM-Profiler.5 Copy number abnormalities were analyzed using CEQer.6 The presence of fusions was assessed using FusionAnalyser,7 and splicing sites mutations using SpliceFinder.8
Validation of mutations and targeted resequencing
All variants were validated by Sanger sequencing. To confirm ETNK1 variants, genomic DNA was polymerase chain reaction-amplified (100 ng per reaction) and sequenced using the following primers: ETNK1-FOR8 CATCAAAGTAAGGGGTTTCTGG and ETNK1-REV8 TCTGCCCCTTGCTGTTGTAG.
Liquid chromatography–mass spectrometry
For liquid chromatography–mass spectrometry experiments, peripheral blood samples (buffy coat) were collected at diagnosis in individuals with aCML. Phenotype was evaluated by fluorescence-activated cell sorting analyses. Only samples with myeloid cells (positive for CD33, CD13, or CD117 staining) greater than 80% of the total were used. As a source of normal cells, we used lymphocytes obtained by culturing patient cells with 2.5 μg/mL phytohemagglutinin-M (PHA-M, Roche) and 200 UI/mL interleukin 2 (Aldesleukin, Novartis) for 3 to 4 days and then incubating cells for 2 to 3 weeks with interleukin 2 only, as previously described.3 Phenotype was evaluated by fluorescence-activated cell sorter analysis. Only samples with lymphoid cells (positive for CD3, CD4, CD5, CD8, or CD19 staining) greater than 80% of the total were used.
Cell lysis and extraction were performed on a total of 5 × 106 cells, as previously described,9 with minor modifications. High-performance liquid chromatography (HPLC)-mass spectrometry quantitation was performed on a Shimadzu-Nexera HPLC chromatograph, interfaced with an AbSciex-3200 QTRAP mass spectrometer (AB SCIEX). HPLC analyses were performed on a Phenomenex Jupiter Proteo 1 × 250 mm. MRM analyses were performed as follows: ion spray voltage, 5500 V; source temperature, 150°C; declustering potential, 35 V; collision energy, 20 eV; GAS1, 15 L/minute; curtain gas, 30 L/minute. Transitions 184.1/86 (phosphocholine) and 142.6/85 (phosphoethanolamine) were used for quantitation purposes. With this experimental setup, the response ratio of phosphocholine/phosphoethanolamine was 15.05.
Methylcellulose colony assay
From a peripheral blood sample (buffy coat; patient CMLPh-019), 150 000 cells were seeded in Methocult H4034 (StemCell Technologies), using the standard protocol. After 2 weeks of incubation at 37°C, 5% CO2, individual colonies were picked, washed with 200 µL phosphate-buffered saline, and lysed in 20 µL of the following buffer: 10 mM Tris⋅HCl, 50 mM NaCl, 6.25 mM MgCl2, 0.045% NP40, and 0.45% Tween-20 at pH 7.6. After adding 1 μL of 20 μg/mL proteinase K, the lysate was incubated at 56°C for 1 hour and at 95°C for 15 minutes. Subsequently, the sample was polymerase chain reaction-amplified by using the following primer pairs: ETNK1-p19-For: CATCAAGAATCTTTGTCAGGAG, ETNK1-p19-Rev: CAAATCCTGTGGGAATGAGAGAG, SETBP1-IntFor: AACTATGCCAAATCTCCAGC, and SETBP1-IntRev: GAAAGTTGTCCACAATGAGATG.
The amplicons were purified on agarose gel, using the QIAquick gel extraction kit (Qiagen), following the standard protocol and eluted in 40 µL H2O. Nine microliters of purified amplicon + 1 µL 25 µM forward primer were used for Sanger sequencing (GATC Biotech).
Mutagenesis
pDONR233 plasmids encoding ETNK1 H243Y and N244S were generated using the following protocol: primers ETNK1_H243Y_For (CCATGCTATTCATGCATACAATGGCTGGATCCCC), ETNK1_H243Y_Rev (GGGGATCCAGCCATTGTATGCATGAATAGCATGG), ETNK1_N244S_ For (CTATTCATGCACACAGTGGCTGGATCCCCAAATC), and ETNK1_N244S_Rev (GATTTGGGGATCCAGCCACTGTGTGCATGAATAG) were used to mutagenize the pDONR223-ETNK1 entry vector (Addgene) with the Pfu Ultra High Fidelity enzyme (Agilent). The product was digested with DpnI (Roche), and 2 µL were used to transform the competent TOP10 bacterial strain (Life Technologies). The presence of the mutations was subsequently confirmed by Sanger sequencing. The coding sequence for ETNK1 variants was then subcloned into the pLX304 vector, using Gateway technology (Life Technologies).
Lentiviral infection
Two hundred ninety-three 293FT packaging cells (Life Technologies) were transfected with 7 µg psPAX2, 1.4 µg pCMV-VSV-G (Addgene), and 7 µg pLX304 (encoding V5-flagged wild type, H243Y, or N244S ETNK1), using jetPRIME (Polyplus-transfection SA). Lentivirus was collected 2 and 3 days after transfection. To generate TF1 cells stably infected with lentiviruses, 5 × 105 cells were transduced by spin infection in lentiviral supernatants supplemented with 4 μg/mL polybrene (Sigma-Aldrich) and 20% RPMI 1640. After 48 hours, the cells expressing wild type and mutated ETNK1 were resuspended in complete medium and selected for 3 weeks in the presence of Blasticidin 10 μg/mL. Western blot was performed using anti-V5 (Abcam) 1:2000 in milk 5% for 2 hours at room temperature (RT) and anti-actin (Sigma) 1:2000 in milk 5% for 2 hours RT; secondary antibodies were anti-mouse (Bio-Rad) 1:2000 incubated for 1 hour RT and anti-rabbit (Bio-Rad) 1:2000 for 1 hour RT, respectively.
Results
To gain insight into the somatic variants responsible for the onset of aCML, we generated whole-exome and transcriptome sequencing data on a cohort of 15 matched case/control aCML samples. A total of 151 nonsynonymous and 42 synonymous single-nucleotide somatic variants were identified. Of these events, 140 were transitions and 53 were transversions. Of the 151 nonsynonymous variants, 141 were missense and 10 were nonsense mutations (supplemental Table 1, available on the Blood Web site). Globally, we identified a total of 6 recurrently mutated genes: SETBP1, NRAS, EZH2, ASXL1, ETNK1, and U2AF1 (Table 1). Surprisingly, no evidence of somatic variants occurring on CSF3R could be found, despite the good sequencing coverage of the whole CSF3R coding region, which suggests CSF3R mutations are significantly more frequent in chronic neutrophilic leukemia than in aCML,10,11 and therefore confirming the different biological basis of the 2 disorders.
Recurrent somatic lesions identified in 15 aCML samples by whole-exome sequencing
| Genes . | Patients . | |||
|---|---|---|---|---|
| SETBP1 | CMLPh-003 | CMLPh-005 | CMLPh-013 | CMLPh-015 |
| NRAS | CMLPh-003 | CMLPh-004 | CMLPh-013 | CMLPh-014 |
| EZH2 | CMLPh-004 | CMLPh-008 | CMLPh-009 | — |
| ASXL1 | CMLPh-005 | CMLPh-013 | CMLPh-014 | — |
| ETNK1 | CMLPh-008 | CMLPh-013 | — | — |
| U2AF1 | CMLPh-007 | CMLPh-011 | — | — |
| Genes . | Patients . | |||
|---|---|---|---|---|
| SETBP1 | CMLPh-003 | CMLPh-005 | CMLPh-013 | CMLPh-015 |
| NRAS | CMLPh-003 | CMLPh-004 | CMLPh-013 | CMLPh-014 |
| EZH2 | CMLPh-004 | CMLPh-008 | CMLPh-009 | — |
| ASXL1 | CMLPh-005 | CMLPh-013 | CMLPh-014 | — |
| ETNK1 | CMLPh-008 | CMLPh-013 | — | — |
| U2AF1 | CMLPh-007 | CMLPh-011 | — | — |
In 2 (13.3%) of 15 samples, we identified the presence of missense, single-nucleotide variants occurring in the ETNK1 gene (supplemental Figure 1A). Both ETNK1 mutations appeared to be present as heterozygous variants in the dominant clone (mutant relative frequency >30%). Interestingly, the mutations affected 2 contiguous residues: H243Y and N244S. Sanger sequencing confirmed the presence and the somatic nature of the 2 variants (supplemental Figure 1B). No fusions or recurrent copy number abnormalities were detected.
The evidence of recurrent, somatic ETNK1 mutations has never been reported in cancer, suggesting these variants could be restricted to aCML and, possibly, to closely related clonal diseases. Targeted resequencing of 515 clonal hematological disorders (Table 2) showed evidence of mutated ETNK1 in 6 of 68 aCML (8.8%; 95% confidence interval, 4%-18%) and in 2 of 77 chronic myelomonocytic leukemia (2.6%; 95% confidence interval, 0.2%-9.5%) samples. In all the cases, ETNK1 variants appeared to be present as a heterozygous, dominant clone. No evidence of ETNK1 mutations was found in the other clonal disorders examined, nor in healthy donors. All variants clustered in the same, highly conserved region12 within the kinase domain (1/8 H243Y and 7/8 N244S) and were heterozygous.
Frequency of ETNK1 mutations in 515 patient samples and 32 healthy donors
| Disease . | Samples . | Mutated samples . | Mutated samples, % . |
|---|---|---|---|
| AML | 64 | 0 | 0.0 |
| ALL | 53 | 0 | 0.0 |
| CLL | 51 | 0 | 0.0 |
| MDS | 77 | 0 | 0.0 |
| MPN | |||
| CML | 38 | 0 | 0.0 |
| PV | 18 | 0 | 0.0 |
| ET | 39 | 0 | 0.0 |
| CNL | 1 | 0 | 0.0 |
| PMF | 14 | 0 | 0.0 |
| MDS/MPN | |||
| aCML | 68 | 6 | 8.8 |
| CMML | 77 | 2 | 2.6 |
| JMML | 5 | 0 | 0.0 |
| MDS/MPN-u | 10 | 0 | 0.0 |
| Healthy donors | 32 | 0 | 0.0 |
| Disease . | Samples . | Mutated samples . | Mutated samples, % . |
|---|---|---|---|
| AML | 64 | 0 | 0.0 |
| ALL | 53 | 0 | 0.0 |
| CLL | 51 | 0 | 0.0 |
| MDS | 77 | 0 | 0.0 |
| MPN | |||
| CML | 38 | 0 | 0.0 |
| PV | 18 | 0 | 0.0 |
| ET | 39 | 0 | 0.0 |
| CNL | 1 | 0 | 0.0 |
| PMF | 14 | 0 | 0.0 |
| MDS/MPN | |||
| aCML | 68 | 6 | 8.8 |
| CMML | 77 | 2 | 2.6 |
| JMML | 5 | 0 | 0.0 |
| MDS/MPN-u | 10 | 0 | 0.0 |
| Healthy donors | 32 | 0 | 0.0 |
aCML, atypical chronic myeloid leukemia; ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; CLL, chronic lymphocytic leukemia; CML, chronic myeloid leukemia; CMML, chronic myelomonocytic leukemia; CNL, chronic neutrophilic leukemia; ET, essential thrombocytosis; JMML, juvenile myelomonocytic leukemia; MDS, myelodysplastic syndromes; MDS/MPN-u=myelodysplastic/myeloproliferative neoplasm-unclassifiable; MPN, myeloproliferative neoplasms; PMF, primary myelofibrosis; PV, polycythemia vera.
In 2 of 6 (33%; 95% confidence interval, 9%-70%) ETNK1-mutated aCML cases, we detected the presence of a coexisting SETBP1 variant. The fraction of SETBP1 mutations within this group was perfectly in line with the overall frequency of SETBP1 mutations in aCML, suggesting that mutations occurring in ETNK1 and SETBP1 are not mutually exclusive.
To assess whether SETBP1 and ETNK1 mutations coexist in the same clone or are present in separate cells, we performed a colony assay in a patient in whom both mutations had been detected (CMLPh-019). Targeted resequencing of both genes on gDNA from 40 individual colonies demonstrated the coexistence of the 2 variants as heterozygous mutations in all the clones tested (supplemental Figure 2).
To further characterize the pattern of ETNK1 mutations in cancer, we tested the presence of somatic ETNK1 variants in leukemias, as well as solid tumors, in a total of 60 paired whole-genome and more than 600 exomes making up 276 paired tumor/germline primary samples and 344 cancer cell lines (http://cancer.sanger.ac.uk/cancergenome/projects/cell_lines/)13-19 by reevaluation of the raw sequencing data. No evidence of recurrent ETNK1 mutations could be found, which suggests that ETNK1 mutations are more frequent in aCML and closely related disorders. Further studies with larger cohorts will be required to thoroughly assess the presence and the frequency of ETNK1 mutations in other clonal disorders. Conservation analysis revealed that the mutated locus is highly conserved across many species (Figure 1A), which indicates it may play a critical, yet unknown, functional role.
ETNK1 mutations in patients with aCML/chronic myelomonocytic leukemia. (A) Outline of the ETNK1 protein. The yellow region highlights the catalytic domain of the protein. The red band corresponds to the mutational hotspot. In the upper part, a conservation analysis of the mutated locus is shown. The red and blue circles highlight the position of individual mutations identified in aCML and chronic myelomonocytic leukemia, respectively. (B) Intracellular phosphoethanolamine/phosphocholine ratio in patients with aCML. The red bars show the intracellular phosphoethanolamine/phosphocholine ratio of leukemic (myeloid) cells in 3 ETNK1 mutated patients (8T, 13T, and 19T, corresponding to patients CMLPh-008, CMLPh-013, and CMLPh-019). The blue bars show the intracellular phosphoethanolamine/phosphocholine ratio of myeloid (3T, 6T) or lymphoid (3H, 6H) cells negative for ETNK1 mutations (patients CMLPh-003 and CMLPh-006). The light red and light blue bars indicate the intracellular phosphoethanolamine/phosphocholine ratio of a matched myeloid/lymphoid sample whose leukemic (myeloid) cells are positive for ETNK1 mutation. The error bars represent the standard deviation of 3 experiments. The asterisks indicate the significance level: *P < .05; **P < .005.
ETNK1 mutations in patients with aCML/chronic myelomonocytic leukemia. (A) Outline of the ETNK1 protein. The yellow region highlights the catalytic domain of the protein. The red band corresponds to the mutational hotspot. In the upper part, a conservation analysis of the mutated locus is shown. The red and blue circles highlight the position of individual mutations identified in aCML and chronic myelomonocytic leukemia, respectively. (B) Intracellular phosphoethanolamine/phosphocholine ratio in patients with aCML. The red bars show the intracellular phosphoethanolamine/phosphocholine ratio of leukemic (myeloid) cells in 3 ETNK1 mutated patients (8T, 13T, and 19T, corresponding to patients CMLPh-008, CMLPh-013, and CMLPh-019). The blue bars show the intracellular phosphoethanolamine/phosphocholine ratio of myeloid (3T, 6T) or lymphoid (3H, 6H) cells negative for ETNK1 mutations (patients CMLPh-003 and CMLPh-006). The light red and light blue bars indicate the intracellular phosphoethanolamine/phosphocholine ratio of a matched myeloid/lymphoid sample whose leukemic (myeloid) cells are positive for ETNK1 mutation. The error bars represent the standard deviation of 3 experiments. The asterisks indicate the significance level: *P < .05; **P < .005.
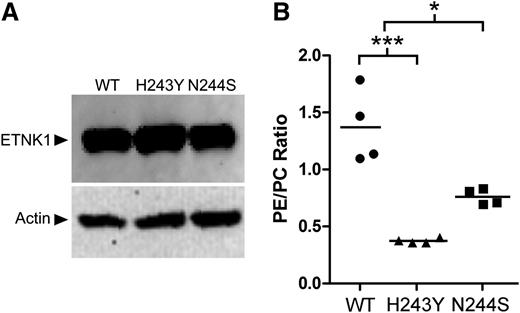
To assess the functional effect of ETNK1 mutations, the intracellular level of phosphoethanolamine, the product of the ETNK1 kinase, was assessed on ETNK1-positive and ETNK1-negative aCML primary samples by using liquid chromatography–mass spectrometry techniques. The analyses were performed on a total of 3 primary peripheral blood myeloid samples carrying ETNK1 mutations (CMLPh-008T, CMLPh-013T, CMLPh-019T), on 4 ETNK1-WT aCML samples, and on ETNK1-WT autologous lymphoid cells from ETNK1-mutated patient 19 (CMLPh-019H). Of the mutated samples, one carried the H243Y and 2 the N244S variant. All the quantifications were performed at least in triplicate. The results showed that the intracellular phosphoethanolamine/phosphocholine ratio was, on average, 5.2-fold lower in ETNK1-mutated samples than in the nonmutated ones (P < .05) and suggested that ETNK1 mutations may damage the catalytic activity of the enzyme (Figure 1B). A similar analysis performed using myeloid TF1 cells transduced with ETNK1-WT, ETNK1-N244S, or ETNK1-H243Y revealed a similar pattern (Figure 2), with an intracellular phosphoethanolamine/phosphocholine ratio significantly lower in ETNK1-N244S (0.76 ± 0.07) and ETNK1-H243Y (0.37 ± 0.02) than in ETNK1-WT (1.37 ± 0.32; P = .01 and P = .0008, respectively).
Phosphoethanolamine/phosphocholine ratio in a TF1-ETNK1 cellular model. (A) Western blot anti-ETNK1 showing the intracellular level of ETNK1 protein in TF1-WT, N244S, and H243Y. (B) Intracellular phosphoethanolamine/phosphocholine ratio as assessed by HPLC–mass Spectrometry in TF1 cells transduced with ETNK1-WT, N244S, and H243Y.
Phosphoethanolamine/phosphocholine ratio in a TF1-ETNK1 cellular model. (A) Western blot anti-ETNK1 showing the intracellular level of ETNK1 protein in TF1-WT, N244S, and H243Y. (B) Intracellular phosphoethanolamine/phosphocholine ratio as assessed by HPLC–mass Spectrometry in TF1 cells transduced with ETNK1-WT, N244S, and H243Y.
Discussion
ETNK1 encodes an ethanolamine kinase, which catalyzes the first step of the de novo phosphatidylethanolamine (PE) biosynthesis pathway (supplemental Figure 3).20 It is responsible for the phosphorylation of ethanolamine to phosphoethanolamine, which is then further processed to PE by a cytidylyltransferase (ECT1) and by the amino alcohol phosphotransferase EPT1.20 PE is involved in many biochemical processes, among them defining membrane architecture,21 regulation of the topology of transmembrane domains of membrane proteins,22 anchoring specific PE-binding proteins to the cell membrane, ensuring the proper progression of cytokinesis during cell division,23 and optimal activity of the respiratory complexes in the inner membrane of mitochondria.23 Given the pleiotropic role of PE, dissecting the biological effects of the ETNK1 mutations will be a complex task. However, the occurrence of all the variants in a highly conserved region and the demonstration that they impair the catalytic activity of ETNK1 suggest these mutations may play a significant functional role.
Within myeloid neoplasms, major differences in disease phenotype can be driven by different combinations of commutated genes.24 Interestingly, aCML and chronic myelomonocytic leukemia share not only clinical and morphological features but also mutant genes.3,25 In this study, targeted resequencing of patients with various myeloid neoplasms revealed somatic ETNK1 mutations only in subjects with aCML or chronic myelomonocytic leukemia, confirming that these disorders have a common genetic basis.
In summary, our study shows for the first time the evidence of recurrent somatic mutations of the ETNK1 gene in the context of MDS/MPN clonal disorders. Further studies will be required to thoroughly dissect the functional effects of these mutations.
The online version of this article contains a data supplement.
There is an Inside Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We gratefully thank Dr Nicholas Cross for providing samples and reagents. We kindly acknowledge the contribution of Michela Viltadi for technical help.
This work was supported by Associazione Italiana Ricerca sul Cancro 2010 (IG-10092 to C.B.G.-P.), 2013 (IG-14249 to C.B.G.-P.), Lombardy Region (ID14546A to C.B.G.-P.), and Leukaemia and Lymphoma Research UK (to J.B.). The studies on myeloid neoplasms conducted at the Department of Hematology Oncology, Fondazione Istituto di ricovero e cura a carattere scientifico Policlinico San Matteo, Pavia, Italy, were supported by grants from Associazione Italiana Ricerca sul Cancro (Special Program Molecular Clinical Oncology 5 per Mille, project no. 1005) and by Fondazione Cariplo (M.C.).
Authorship
Contribution: C.B.G.-P. conceived of research, critically revised data, and wrote the manuscript; C.D., A. Parmianai, and D.F. generated Sanger sequencing data and validated somatic variants; A. Pirola generated next-generation sequencing (NGS) data; S.R. generated Sanger sequencing data and critically revised the manuscript; G. Signore generated and analyzed liquid chromatography–mass spectrometry data; V.P. analyzed liquid chromatography–mass spectrometry data and critically revised the manuscript; L.M. provided vital reagents and critically revised the manuscript; R.S. analyzed NGS data; V.M. and M.P. generated Sanger sequencing data; G.G., A.M., C.P., G. Saglio, E.U., D.-W.K., D.R., K.Z., N.V., A.S., H.B., J.B., L.C., M. Carrabba, E.E., P.J.C., and M. Cazzola provided vita reagents and critically revised the manuscript; M.P. generated Sanger sequencing data; G.R.B. analyzed cell lines and NGS data and revised the manuscript; E.P. provided vital reagents, analyzed NGS data, and critically revised the manuscript; and R.P. conceived research, generated data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Rocco Piazza, University of Milano-Bicocca, Via Cadore 48, Monza, Milan 20900, Italy; e-mail: rocco.piazza@unimib.it.