Key Points
An increase in the classical monocyte subset to >94% of total monocytes discriminates CMML from other monocytoses with high specificity.
This characteristic increase in classical monocytes disappears in CMML patients who respond to hypomethylating agents.
Abstract
Chronic myelomonocytic leukemia (CMML) is a myelodysplastic syndrome/ myeloproliferative neoplasm whose diagnosis is currently based on the elevation of peripheral blood monocytes to >1 × 109/L, measured for ≥3 months. Diagnosis can be ambiguous; for example, with prefibrotic myelofibrosis or reactive monocytosis. We set up a multiparameter flow cytometry assay to distinguish CD14+/CD16− classical from CD14+/CD16+ intermediate and CD14low/CD16+ nonclassical monocyte subsets in peripheral blood mononucleated cells and in total blood samples. Compared with healthy donors and patients with reactive monocytosis or another hematologic malignancy, CMML patients demonstrate a characteristic increase in the fraction of CD14+/CD16− cells (cutoff value, 94.0%). The associated specificity and sensitivity values were 95.1% and 90.6% in the learning cohort (175 samples) and 94.1% and 91.9% in the validation cohort (307 samples), respectively. The accumulation of classical monocytes, which demonstrate a distinct gene expression pattern, is independent of the mutational background. Importantly, this increase disappears in patients who respond to hypomethylating agents. We conclude that an increase in the fraction of classical monocytes to >94.0% of total monocytes is a highly sensitive and specific diagnostic marker that rapidly and accurately distinguishes CMML from confounding diagnoses.
Introduction
According to the World Health Organization (WHO) classification, the diagnosis of chronic myelomonocytic leukemia (CMML), the most frequent myelodysplastic syndrome (MDS)/myeloproliferative neoplasm (MPN), is based on the elevation of peripheral blood monocytes to >1 × 109/L, measured for ≥3 months.1,2 Bone marrow cell dysplasia, which enforces the diagnosis when present, is not an absolute requirement.1 Some patients with reactive monocytosis can fulfill this criterion, whereas patients with MDS and a low white blood cell count (but as high as 80% of monocytes) do not.
The Nomenclature Committee of the International Union of Immunological Societies has approved a nomenclature that subdivides monocytes into 3 subsets.3 This subdivision was validated by gene expression profiling.4-6 Specifically, the expression of CD14, a receptor for bacterial lipopolysaccharides, and CD16, which is the low-affinity receptor for immunoglobulin G (Fcγ-III receptor), distinguishes CD14+/CD16− (classical) from CD14+/CD16+ (intermediate) and CD14low/CD16+ (nonclassical) human monocytes.3 CD14+/CD16− monocytes constitute the major population of human monocytes (∼85%) in healthy conditions.3 These subsets differ in their chemokine receptor expression and phagocytic activity3,5,7 ; that is, CD14+/CD16− monocytes express high levels of CCR2 and low levels of CX3CR1, whereas CD16+ monocytes express high levels of CX3CR1 and low levels of CCR2.8-10 Akin to lymphocytes, these subsets may be endowed with specific functions.4-6,11,12
Here, we demonstrate that an increase in the fraction of classical CD14+/CD16− monocytes at the expense of intermediate and nonclassical fractions is a highly specific marker that rapidly, accurately, and simply distinguishes CMML from confounding diagnoses. Interestingly, the monocyte subset repartition is normalized in patients who respond to hypomethylating agents.
Materials and methods
Patients and samples
Peripheral blood samples were collected on EDTA after informed consent according to the Declaration of Helsinki. A learning cohort included patients with a CMML diagnosis according to the WHO classification criteria (n = 53); age-matched healthy donors (n = 39); young healthy blood donors (n = 26); patients with reactive monocytosis (n = 33); and patients with non-CMML hematologic malignancies (n = 24), including MPNs (n = 12), MDS (n = 7), juvenile myelomonocytic leukemia (n = 1), and lymphoid malignancies (n = 4). CMML patients were enrolled between 2012 and 2013 in a noninterventional study initiated by the Groupe Francophone des Myélodysplasies and approved by the ethical committee of Cochin Hospital, according to current regulations and ethical concerns. A validation cohort included CMML patients enrolled between 2013 and 2015 (n = 86); age-matched healthy donors (n = 68); patients with reactive monocytosis (n = 74); and patients with a diagnosis of MDS (n = 65), MPN (n = 12), or MPN/MDS (1 atypical chronic myelogenous leukemia, 1 juvenile myelomonocytic leukemia), referred to as non-CMML. Detailed characteristics of these groups are in Table 1. Cytogenetic risk was classified according to the Spanish CMML classification.13 Gene mutations were screened as described previously.14
Baseline characteristics of the subjects in the learning and validation cohorts
| . | Learning cohort* . | Validation cohort . | ||||||
|---|---|---|---|---|---|---|---|---|
| CMML† (n = 53) . | Aged-Co (n = 39) . | Non-CMML (n = 24) . | Reactive (n = 33) . | CMML† (n = 86) . | Aged-Co (n = 68) . | Non-CMML (n = 79) . | Reactive (n = 74) . | |
| Age, median y (range) | 78 (53-91) | 79 (62-94) | 74 (2-94) | 63.5 (36-87) | 77 (46-97) | 79.5 (50-92) | 73 (0.5-92) | 65 (37-91) |
| Gender, n (%) | ||||||||
| Male | 37 (70) | 13 (33) | 13 (54) | 20 (61) | 59 (69) | 16 (24) | 43 (55) | 40 (54) |
| Female | 16 (30) | 26 (67) | 11 (46) | 13 (39) | 27 (31) | 52 (76) | 36 (45) | 34 (46) |
| White blood cell count, median n × 109/L (range) | 9.25 (3.7-84.7) | 6.8 (4.9-16.4) | 7.4 (2.3-79.9) | 11.8 (4.7-33.4) | 9.3 (3.2-122.3) | 6.6 (4.6-9.9) | 5.7 (0.89-112.3) | 10.2 (4.2-658) |
| Hemoglobin, median g/dL (range) | 12.10 (7.5-14.9) | 12.8 (11.1-16.7) | 13.15 (8-26.8) | 10.6 (8-14.3) | 11.7 (6.1-16.9) | 13 (11.6-15.9) | 10.6 (5-18.2) | 10.7 (7.9-19) |
| Platelet count, median n × 109/L (range) | 86.5 (13-457) | 229 (156-406) | 207.5 (37-1045) | 298.5 (57-1143) | 132.5 (13-529) | 244 (129-443) | 151 (17-869) | 259 (7-1037) |
| Monocyte count, median n × 109/L (range) | 2.51 (1-28.8) | 0.62 (0.31-0.96) | 0.72 (0.2-2) | 1.3 (1.1-7) | 1.85 (1-60) | 0.6 (0.4-0.6) | 0.63 (0.11-21.98) | 1.4 (1-5.9) |
| CMML type 1/CMML type 2 | 48/5 | 63/11 | ||||||
| Low/intermediate/high cytogenetic risk, n | 41/5/1 | 45/5/6 | ||||||
| . | Learning cohort* . | Validation cohort . | ||||||
|---|---|---|---|---|---|---|---|---|
| CMML† (n = 53) . | Aged-Co (n = 39) . | Non-CMML (n = 24) . | Reactive (n = 33) . | CMML† (n = 86) . | Aged-Co (n = 68) . | Non-CMML (n = 79) . | Reactive (n = 74) . | |
| Age, median y (range) | 78 (53-91) | 79 (62-94) | 74 (2-94) | 63.5 (36-87) | 77 (46-97) | 79.5 (50-92) | 73 (0.5-92) | 65 (37-91) |
| Gender, n (%) | ||||||||
| Male | 37 (70) | 13 (33) | 13 (54) | 20 (61) | 59 (69) | 16 (24) | 43 (55) | 40 (54) |
| Female | 16 (30) | 26 (67) | 11 (46) | 13 (39) | 27 (31) | 52 (76) | 36 (45) | 34 (46) |
| White blood cell count, median n × 109/L (range) | 9.25 (3.7-84.7) | 6.8 (4.9-16.4) | 7.4 (2.3-79.9) | 11.8 (4.7-33.4) | 9.3 (3.2-122.3) | 6.6 (4.6-9.9) | 5.7 (0.89-112.3) | 10.2 (4.2-658) |
| Hemoglobin, median g/dL (range) | 12.10 (7.5-14.9) | 12.8 (11.1-16.7) | 13.15 (8-26.8) | 10.6 (8-14.3) | 11.7 (6.1-16.9) | 13 (11.6-15.9) | 10.6 (5-18.2) | 10.7 (7.9-19) |
| Platelet count, median n × 109/L (range) | 86.5 (13-457) | 229 (156-406) | 207.5 (37-1045) | 298.5 (57-1143) | 132.5 (13-529) | 244 (129-443) | 151 (17-869) | 259 (7-1037) |
| Monocyte count, median n × 109/L (range) | 2.51 (1-28.8) | 0.62 (0.31-0.96) | 0.72 (0.2-2) | 1.3 (1.1-7) | 1.85 (1-60) | 0.6 (0.4-0.6) | 0.63 (0.11-21.98) | 1.4 (1-5.9) |
| CMML type 1/CMML type 2 | 48/5 | 63/11 | ||||||
| Low/intermediate/high cytogenetic risk, n | 41/5/1 | 45/5/6 | ||||||
Age-Co, age-matched healthy donors; non-CMML, patients with diverse hematologic malignancies; Reactive, patients with reactive monocytosis.
The characteristics of young healthy donors (n = 26), who are voluntary blood donors, are unknown.
In these series, CMML patients were studied before any treatment.
Multifluorochrome staining and analysis of monocyte subsets
Flow cytometry analysis of monocyte subsets was performed following consensus recommendations.15,16 Peripheral blood mononuclear cells (PBMCs) were sorted17 and labeled with antibodies (supplemental Table 1, available on the Blood Web site). At least 60 000 events in the CD14+/CD16− gate (supplemental Figure 1) were analyzed by flow cytometry (LSR II, BD Biosciences). Whole peripheral blood (200 μL) cells were labeled with antibodies (supplemental Table 1) following a lyse/no wash procedure (VersaLyse, Beckman Coulter). At least 50 000 events in the CD14+/CD16− gate (supplemental Figure 2) were analyzed (Navios, Beckman Coulter). The settings were harmonized between instruments.15,16 Flow cytometry standard listmode data were analyzed centrally in a blind fashion using Kaluza software (Beckman Coulter). The monocyte subsets were identified following an exclusion gating strategy (supplemental Figures 1 and 2). Repeatability and reproducibility of the analytic strategy was validated on 20 randomly chosen samples, as described in supplemental Data.
Cell sorting, cytologic analysis, and RNA sequencing
PBMCs were stained with CD45, CD24, CD14, CD16, CD2, and CD56 antibodies, and monocytes subsets were sorted (Influx cytometer, BD Biosciences), centrifuged on microscope slides, dried for 1 hour at room temperature, and stained with May-Grünwald-Giemsa stain. RNA sequencing was performed on sorted CD14+/CD16− monocytes from healthy donors (n = 4) and from patients with reactive monocytosis (n = 4) or CMML (n = 6). After having checked RNA integrity on an Agilent 2100 Bioanalyzer (Agilent Technologies; score ≥7.0), poly-A messenger RNA was fragmented, converted into double-stranded DNA, and used for library preparation using SureSelect Automated Strand-Specific RNA Library Preparation Kit. The libraries were bar-coded, purified, pooled in equal concentrations, and subjected to paired-end sequencing on a HiSeq 2000 sequencer (Illumina). Bioinformatic analysis is described in supplemental Data.
Statistical analysis
Principal component analysis was performed using the SPADE (spanning-tree progression analysis of density-normalized events) algorithm (Cytobank software).18 The nonparametric Kruskal-Wallis test was used to compare distributions between groups. Receiver operator characteristic curves (ROCs) representing the relationship between sensitivity and specificity were compared to a nonparameteric approach.19 A cutoff was estimated in the learning cohort by maximizing the Youden index (J = sensitivity + specificity − 1). The classification performance of the estimated cutoff was assessed in the validation cohort and compared to the classical CD14+/CD16− monocyte count cutoff of 1 × 109/L. The performance of using both the CD14+/CD16− monocyte percentage and monocyte counts for the classification of patients with CMML or non-CMML in the validation cohort was further assessed with a multivariate logistic regression model. Analyses were done with SAS v.9.3 (SAS Institute, Cary, NC) and P values <.05 were considered significant.
Results
Flow cytometry identification of monocytes subsets
The repartition of monocyte subsets in PBMCs from healthy donors was analyzed by flow cytometry. We used an exclusion gating strategy (supplemental Figure 1) to identify monocytes and to separate the CD14+/CD16− classical monocytes (herein called MO1s) from the CD14+/CD16+ intermediate monocytes (MO2s) and the CD14low/CD16+ nonclassical monocytes (MO3s) (Figure 1A).5 Cytologic examination showed that each sorted population consisted almost exclusively of monocytes, which were absent from the double-negative cell population (Figure 1B). Variations in the expression of monocyte subset–specific markers5 were validated by real-time quantitative polymerase chain reaction or flow cytometry (supplemental Figure 3). We used a computational approach to objectively organize our cytometry data into a hierarchy of related phenotypes in an unsupervised and unbiased manner. The SPADE algorithm automatically formed a “tree” in which monocytes were separated from other blood cells and clustered as 3 subsets with distinct expression of CD14, CD16, CCR2, and CX3CR1 (Figure 1C). All these results confirmed the relevance of our gating strategy. Lastly, the flow cytometry assay was adapted to eliminate the mononuclear cell–sorting step and measure the monocyte subset fractions on whole blood samples (supplemental Figure 2).
Monocyte subsets in PBMCs were explored. (A) PBMCs from a representative healthy blood donor were labeled with anti-CD45, -CD24, -CD14, -CD16, -CD56, -CD115, -CD62L, -CD64, -CCR2, and -CX3CR1 antibodies. Monocytes were identified using an exclusion gating strategy (described in supplemental Figure 1), and subsets were separated on CD14 and CD16 expression. The percentage of each subset is indicated. (B) May-Grünwald-Giemsa staining of sorted MO1s, MO2s, MO3s, and DN (remaining double-negative CD14−/CD16−) cells. (C) Multiparametric analysis of single cells monitored with 10 surface markers (supplemental Table 1) using the SPADE algorithm, which organizes cells in a hierarchy of related phenotypes. Flow cytometry data from 19 healthy donor PBMCs were gated on morphology, then on CD45+/SSC intermediate, and used to construct the SPADE tree that automatically separates, on the basis of the hierarchy of related phenotypes, MO1s (CD14+/CD16−), MO2s (CD14+/CD16+), MO3s (CD14low/CD16+), natural killer cells (NK; CD56+), B lymphocytes (CD24+), and residual granulocytes (Gran; CD24+/CD16+). The percentage of each subset in the monocyte population is indicated. Circles indicate the size of cell populations, and colors are based on CD14 expression. (D) Color representation of CD16, CX3CR1, and CCR2 expression in the monocyte subsets delineated in the SPADE tree.
Monocyte subsets in PBMCs were explored. (A) PBMCs from a representative healthy blood donor were labeled with anti-CD45, -CD24, -CD14, -CD16, -CD56, -CD115, -CD62L, -CD64, -CCR2, and -CX3CR1 antibodies. Monocytes were identified using an exclusion gating strategy (described in supplemental Figure 1), and subsets were separated on CD14 and CD16 expression. The percentage of each subset is indicated. (B) May-Grünwald-Giemsa staining of sorted MO1s, MO2s, MO3s, and DN (remaining double-negative CD14−/CD16−) cells. (C) Multiparametric analysis of single cells monitored with 10 surface markers (supplemental Table 1) using the SPADE algorithm, which organizes cells in a hierarchy of related phenotypes. Flow cytometry data from 19 healthy donor PBMCs were gated on morphology, then on CD45+/SSC intermediate, and used to construct the SPADE tree that automatically separates, on the basis of the hierarchy of related phenotypes, MO1s (CD14+/CD16−), MO2s (CD14+/CD16+), MO3s (CD14low/CD16+), natural killer cells (NK; CD56+), B lymphocytes (CD24+), and residual granulocytes (Gran; CD24+/CD16+). The percentage of each subset in the monocyte population is indicated. Circles indicate the size of cell populations, and colors are based on CD14 expression. (D) Color representation of CD16, CX3CR1, and CCR2 expression in the monocyte subsets delineated in the SPADE tree.
A CMML signature defined by monocyte subsets
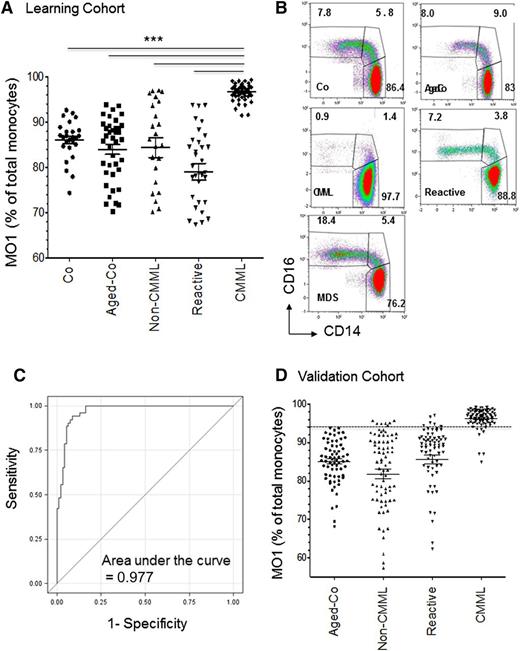
The percentage of MO1s in the peripheral blood monocyte population was 86.1% (standard deviation [SD], 4.3%; 95% confidence interval [CI], 78.0-92.0) in young healthy blood donors and 84.0% (SD, 6.9%; 95% CI, 71.8-93.6) in age-matched healthy subjects (Figure 2A-B). No significant difference was observed between these 2 groups. Compared with control subjects, CMML patients demonstrated an increased percentage of MO1s and a decreased fraction of MO2 and MO3 subsets (Figure 2B). The percentage of MO1s, assessed in a learning cohort of 53 CMML patients, was significantly higher than in healthy control subjects, reaching 96.6% (SD, 1.7%; 95% CI, 92.9-99.1; Figure 2A). The use of the SPADE algorithm independently showed an amplification of MO1s at the expense of the MO2 and MO3 subsets (supplemental Figure 4A-B).
Abnormal repartition of monocyte subsets in CMML. (A) Percentage of MO1s in a learning cohort of CMML patients as compared to healthy blood donors (Co), age-matched healthy donors (Aged-Co), patients with diverse hematologic malignancies (Non-CMML), and those with reactive monocytosis (Reactive). Data are presented as the mean ± SEM; ***P < .0001; Kruskal-Wallis test. (B) Multicolor representation of monocyte subset repartition in PBMCs collected from the distinct groups of the learning cohort. The percentage of each monocyte subset is indicated. (C) ROC curve analysis of diagnostic sensitivity and specificity of MO1 percentage in peripheral blood monocytes established on the learning cohort (young and age-matched healthy donors, other hematologic malignancies, reactive monocytosis, and CMML) defined in panel A. (D) Percentage of MO1s in a validation cohort of CMML as compared to age-matched healthy donors (Aged-Co), patients with MDS or MPN (Non-CMML), and those with reactive monocytosis (Reactive). Data are presented as the mean ± SEM. SEM, standard error of the mean.
Abnormal repartition of monocyte subsets in CMML. (A) Percentage of MO1s in a learning cohort of CMML patients as compared to healthy blood donors (Co), age-matched healthy donors (Aged-Co), patients with diverse hematologic malignancies (Non-CMML), and those with reactive monocytosis (Reactive). Data are presented as the mean ± SEM; ***P < .0001; Kruskal-Wallis test. (B) Multicolor representation of monocyte subset repartition in PBMCs collected from the distinct groups of the learning cohort. The percentage of each monocyte subset is indicated. (C) ROC curve analysis of diagnostic sensitivity and specificity of MO1 percentage in peripheral blood monocytes established on the learning cohort (young and age-matched healthy donors, other hematologic malignancies, reactive monocytosis, and CMML) defined in panel A. (D) Percentage of MO1s in a validation cohort of CMML as compared to age-matched healthy donors (Aged-Co), patients with MDS or MPN (Non-CMML), and those with reactive monocytosis (Reactive). Data are presented as the mean ± SEM. SEM, standard error of the mean.
To determine whether this abnormal percentage of MO1s was specific to CMML, we measured the percentage of MO1s in the peripheral blood of patients with either reactive monocytosis (MO1s, 79.1%; SD, 10.5%; 95% CI, 67.4-93.7) or another hematologic malignancy, regardless of the monocyte count (MO1s, 84.4%; SD, 10.62%; 95% CI, 70.2-96.9) (Figure 2A-B and supplemental Figure 5). The proportion of MO1s in the monocyte compartment was significantly higher in CMML patients than in any other studied group (P < .0001, Kruskal-Wallis test). Differences between groups of the learning cohort (other than the CMML patient group) were not significant.
The combination of CCR2 (CD192) and CX3CR1 expression also distinguishes 3 monocyte subsets in healthy donors, namely CCR2+/CX3CR1−, CCR2+/CX3CR1+, and CCR2low/CX3CR1+ subsets.8 A strong overlap between populations identified by the CD14/CD16 and the CCR2/CX3CR1 surface marker combinations was observed. CMML patients demonstrated an increased fraction of CCR2+/CX3CR1− cells and a decreased fraction of CCR2+/CX3CR1+ and CCR2low/CX3CR1+ cells (supplemental Figure 4C), suggesting that the increase in MO1 fraction was not the consequence of a CMML-associated decrease in CD16 expression.
MO1 percentage as a sensitive and specific tool for CMML diagnosis
To further explore whether the increased MO1 subset could be helpful to diagnose CMML, we performed a ROC analysis using data from the learning cohort. The area under the ROC curve (AUC) was 0.977 (95% CI, 0.96-0.995; Figure 2C), indicating that the percentage of MO1s could be used to distinguish CMML from any other situation. The Youden index was defined for all points of the ROC curve in the learning population. The maximum value of the index was used as a criterion for selecting the optimum cutoff point of MO1 percentage to identify CMML. A cutoff value of 94.0% was calculated with a specificity of 95.1% and a sensitivity of 90.6%. We validated the cutoff value in the independent cohort (Figure 2D). In this validation cohort, the specificity and sensitivity values of the “MO1 percentage >94.0%” criterion were 94.1% and 91.9%, respectively. The MO1 percentage was 96.4% (SD, 2.5%; 95% CI, 87.1-99.1) in CMML patients; 85.1% (SD, 5.6%; 95% CI, 69.5-93.8) in age-matched healthy control subjects; 85.8% (SD, 9.9%; 95% CI, 52.5-96.6) in patients with reactive monocytosis; and 81.9% (SD, 11.5%; 95% CI, 49.3-95.7) in non-CMML patients. Of note, we also tested the MO1/MO3 ratio in the learning and validation cohorts; this ratio was not statistically more efficient than MO1 percentage in identifying CMML patients.
CMML diagnosis is currently based on the elevation of peripheral blood monocytes to >1 × 109/L. We performed an ROC analysis on the subset of patients with a monocyte count >1 × 109/L in the learning cohort. The AUC of the ROC curve drawn in a monocytosis context was 0.995 (95% CI: 0.988-1.00) (supplemental Figure 6). The specificity and the sensitivity were 100% and 90.4%, respectively, for an MO1 percentage cutoff point of 94.0%. Validation of this cutoff for patients in the validation cohort with a monocyte count >1 × 109/L was 94.5% for specificity and 91.7% for sensitivity. These data indicate that the MO1 percentage could be used to improve CMML diagnosis in this specific subset of patients with an elevated monocyte count.
CMML patients accumulate abnormal MO1s
The MO1 percentage for CMML patients was observed to be independent of the absolute number of circulating monocytes (Figure 3A); the gene mutation pattern (Table 2; additional data not shown); the proliferative vs dysplastic status of the disease according to the French-American-British classification criteria (leukocyte count cutoff value 13 × 109/L; data not shown); and the disease subtype (CMML type 1 vs type 2) according to WHO criteria (data not shown).20 The characteristic repartition of monocyte subsets in the peripheral blood of CMML patients reflects an increase in the absolute number of MO1s and a decrease in the absolute number of MO3s compared to monocyte subsets in healthy donor peripheral blood. Conversely, patients with reactive monocytosis show a significant increase in the number of cells in the MO1 and MO3 subsets (Figure 3B). In 18 CMML patients, the increased percentage of MO1s identified in the peripheral blood was also observed in the bone marrow (data not shown). Therefore, the decrease in MO3s observed in the blood of CMML patients may not be related to their bone marrow retention.
CMML patients accumulate abnormal MO1s at the expense of MO3s. (A) Lack of significant correlation between the percentage of MO1s and peripheral blood monocyte count in reactive monocytosis (black circles) and in CMML (red circles). Reactive monocytoses and CMML samples from the learning and validation cohorts were pooled. (B) Absolute number of MO1s and MO3s in the peripheral blood of CMML patients as compared to age-matched healthy donors (Aged-Co), non-CMML patients, and patients with reactive monocytosis. The learning and validation cohorts were pooled (***P < .0001; Student t test). (C) Component principal analysis of gene expression after RNA sequencing (DESSeq2 analysis) in MO1s sorted from the blood of healthy donors (green) and patients with reactive monocytosis (blue) or CMML (red). (D) Heatmap established by using Cytobank software to summarize the flow cytometry analysis of 8 markers at the surface of MO1s from 6 age-matched healthy donors and 17 CMML patients.
CMML patients accumulate abnormal MO1s at the expense of MO3s. (A) Lack of significant correlation between the percentage of MO1s and peripheral blood monocyte count in reactive monocytosis (black circles) and in CMML (red circles). Reactive monocytoses and CMML samples from the learning and validation cohorts were pooled. (B) Absolute number of MO1s and MO3s in the peripheral blood of CMML patients as compared to age-matched healthy donors (Aged-Co), non-CMML patients, and patients with reactive monocytosis. The learning and validation cohorts were pooled (***P < .0001; Student t test). (C) Component principal analysis of gene expression after RNA sequencing (DESSeq2 analysis) in MO1s sorted from the blood of healthy donors (green) and patients with reactive monocytosis (blue) or CMML (red). (D) Heatmap established by using Cytobank software to summarize the flow cytometry analysis of 8 markers at the surface of MO1s from 6 age-matched healthy donors and 17 CMML patients.
CMML patient mutations in learning and validation cohorts
| Mutations . | Learning cohort (48 CMML)* . | Validation cohort (26 CMML)* . |
|---|---|---|
| TET2 (mutated/studied) | 36/48 | 14/26 |
| SRSF2 (mutated/studied) | 21/48 | 7/24 |
| ASXL1 (mutated/studied) | 13/48 | 5/26 |
| RAS Path (CBL+NRAS+KRAS) (mutated/studied) | 12/48 | 7/26 |
| AML1 (mutated/studied) | 6/48 | 3/26 |
| JAK2 (mutated/studied) | 1/48 | 1/26 |
| IDH1/IDH2 (mutated/studied) | 1/48 | 0/26 |
| ZRSR2 (mutated/studied) | 4/48 | 1/26 |
| DNMT3A (mutated/studied) | 3/48 | 2/25 |
| EZH2 (mutated/studied) | 1/48 | 2/25 |
| SF3B1 (mutated/studied) | 1/48 | 5/25 |
| FLT3 (mutated/studied) | 0/48 | 1/26 |
| NPM1, c-KIT, U2AF35 (mutated/studied) | 0/48 | 0/26 |
| Mutations . | Learning cohort (48 CMML)* . | Validation cohort (26 CMML)* . |
|---|---|---|
| TET2 (mutated/studied) | 36/48 | 14/26 |
| SRSF2 (mutated/studied) | 21/48 | 7/24 |
| ASXL1 (mutated/studied) | 13/48 | 5/26 |
| RAS Path (CBL+NRAS+KRAS) (mutated/studied) | 12/48 | 7/26 |
| AML1 (mutated/studied) | 6/48 | 3/26 |
| JAK2 (mutated/studied) | 1/48 | 1/26 |
| IDH1/IDH2 (mutated/studied) | 1/48 | 0/26 |
| ZRSR2 (mutated/studied) | 4/48 | 1/26 |
| DNMT3A (mutated/studied) | 3/48 | 2/25 |
| EZH2 (mutated/studied) | 1/48 | 2/25 |
| SF3B1 (mutated/studied) | 1/48 | 5/25 |
| FLT3 (mutated/studied) | 0/48 | 1/26 |
| NPM1, c-KIT, U2AF35 (mutated/studied) | 0/48 | 0/26 |
In these series, CMML patients were studied before any treatment.
CMML MO1s did not show major cytologic alteration compared to healthy donor MO1s, although the monocytes’ nuclei look more undifferentiated in CMML patients (supplemental Figure 7A). RNA sequencing analysis of the MO1 subset sorted from healthy donors, patients with reactive monocytosis, and CMML patients showed a distinct pattern of gene expression in the 3 situations (Figure 3C and supplemental Figure 7B). Moreover, the expression of CD56, CD115, and CD62L was significantly higher at the surface of CMML MO1s compared to healthy donor MO1s (Figure 3D).
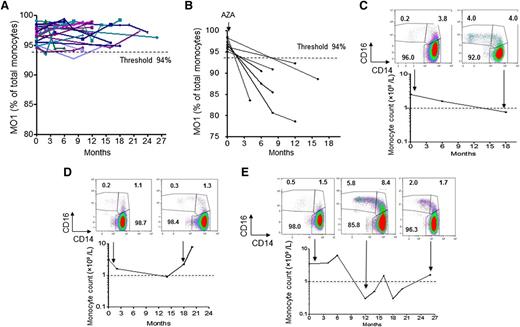
Monocyte subset profile is a biomarker of CMML response to demethylating agents
The increased percentage of MO1s remained at >94.0% in 21 untreated CMML patients repeatedly analyzed for up to 26 months (Figure 4A). We also observed a normalization of monocyte subset repartition, together with a decrease in the monocyte count <1 × 109/L, in 7 CMML patients who responded to azacytidine therapy (Figure 4B-C and supplemental Figure 8A), whereas monocyte repartition remained unchanged in nonresponding patients (Figure 4D) and a characteristic phenotype reappeared in a patient who relapsed after initial response (Figure 4E). Lastly, in a CMML patient who relapsed on azacytidine therapy, we observed a normalization of monocyte count and MO1 fraction in response to decitabine (supplemental Figure 8B). Together, these results indicate that the monocyte subset repartition could be used as a biomarker of demethylating-agent activity in CMML patients.
Monocyte subset profile as a biomarker of disease evolution. (A) Repeated evaluation of MO1 fraction in 21 untreated CMML patients followed from 6 to 26 months. (B) Evaluation of MO1 fraction in 7 CMML patients before and after treatment with azacytidine (AZA); all 7 patients responded to treatment.11 (C-E) Evolution of monocyte subset repartition and monocyte count in CMML patients during treatment with a demethylating agent. (C) Patient who responded to azacytidine. (D) Patient who only transiently responded to azacytidine. (E) Patient who relapsed after initial response.
Monocyte subset profile as a biomarker of disease evolution. (A) Repeated evaluation of MO1 fraction in 21 untreated CMML patients followed from 6 to 26 months. (B) Evaluation of MO1 fraction in 7 CMML patients before and after treatment with azacytidine (AZA); all 7 patients responded to treatment.11 (C-E) Evolution of monocyte subset repartition and monocyte count in CMML patients during treatment with a demethylating agent. (C) Patient who responded to azacytidine. (D) Patient who only transiently responded to azacytidine. (E) Patient who relapsed after initial response.
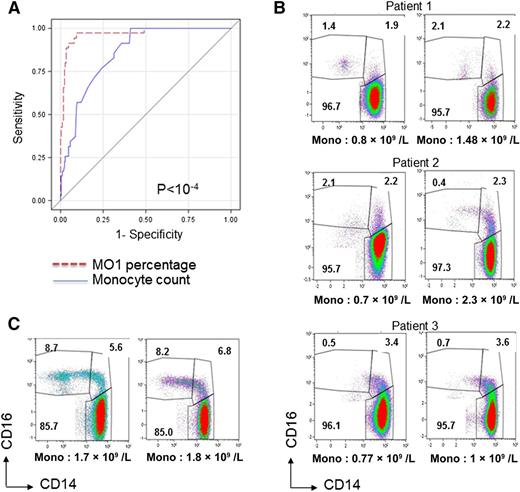
Monocyte subset profile is more efficient than monocyte count in diagnosing CMML
Lastly, we compared the criteria “MO1 percentage >94.0%” and “monocyte count >1 × 109/L” to identify CMML at initial workup, always using the WHO criteria to validate CMML diagnosis. For that purpose, we used the entire validation cohort (including 65 MDS patients). The AUCs of the ROC curves were 0.968 with percentage of MO1s (95% CI, 0.946-0.99) and 0.836 with monocyte count (95% CI, 0.792-0.88) (Figure 5A). The difference between the ROC curves was highly significant (P < 10−4, χ2 test). The specificity and sensitivity values of MO1 percentage were 94.1% and 91.9%, respectively, whereas the specificity and sensitivity values of the monocyte count were 95.3% and 62.0%, respectively. These results demonstrate that the MO1 percentage is a better parameter than the monocyte count to diagnose CMML at initial workup. In a multivariate logistic regression model, in which both MO1 percentage and monocyte count were entered, only the MO1 percentage was retained to classify the patients in the CMML group.
Comparison between monocyte subset profile and monocyte count diagnosis. (A) ROC curves of the “MO1 percentage >94.0%” and “monocyte count >1 × 109/L” criteria to identify CMML at initial workup in the validation cohort. The difference between the 2 curves was highly significant (P < .0001, χ2 test). (B) Monocyte subset repartition analyzed in 2 independent samples obtained from 3 patients classified as having MDS and showing a fluctuating monocyte count of ∼1 × 109/L that precludes their classification as CMML according to the WHO criteria. (C) Monocyte subset repartition analyzed in 2 independent samples obtained from a patient who could be classified as having CMML according to the WHO criteria but who, based on cytologic and molecular analyses, demonstrates sideroblastic anemia with monocytosis.
Comparison between monocyte subset profile and monocyte count diagnosis. (A) ROC curves of the “MO1 percentage >94.0%” and “monocyte count >1 × 109/L” criteria to identify CMML at initial workup in the validation cohort. The difference between the 2 curves was highly significant (P < .0001, χ2 test). (B) Monocyte subset repartition analyzed in 2 independent samples obtained from 3 patients classified as having MDS and showing a fluctuating monocyte count of ∼1 × 109/L that precludes their classification as CMML according to the WHO criteria. (C) Monocyte subset repartition analyzed in 2 independent samples obtained from a patient who could be classified as having CMML according to the WHO criteria but who, based on cytologic and molecular analyses, demonstrates sideroblastic anemia with monocytosis.
Further analysis of the 11 MDS patients who had an MO1 percentage >94.0% revealed that all had a fluctuating monocyte count of ∼1 × 109/L, precluding the diagnosis of CMML according to the WHO criteria (Figure 5B). These observations suggest that the flow cytometry assay identifies CMML in situations in which the WHO criteria are (still) not fulfilled. Conversely, in a patient classified as CMML type 1 according to the WHO criteria whom we serially explored over a 2-year period (Figure 5C), we never detected the characteristic MO1 accumulation, and bone marrow examination revealed a sideroblastic anemia with mutations in SF3B1 and DNMT3A genes. Further investigation may distinguish a CMML with an unusual phenotype (eg, due to a specific background of genetic alterations) from a sideroblastic anemia with monocytosis.21,22
Discussion
We show that CMML is characterized by an increase in the fraction of classical CD14+/CD16− cells (MO1s) among circulating monocytes, whatever the genetic background of the disease. This increase can be rapidly identified using a robust multiparameter flow cytometry assay performed on peripheral blood, and distinguishes CMML from reactive monocytosis and myeloid malignancies in patients with a borderline monocyte count. Importantly, normalization of the monocyte subset repartition could be used as a biomarker of treatment efficacy in this disease.
Both the development and biological significance of monocyte subsets remain a matter of active investigation.9,23-28 Whatever their respective functions and their developmental relationships, CD16+ monocyte subsets expand in a variety of clinical situations,29 including autoimmune diseases,30 bacterial and viral infections,31-33 asthma,34 stroke, and coronary artery disease.35 Conversely, a reduction in MO1s was observed after treatment with intravenous immunoglobulins36 or blockade of the macrophage colony-stimulating factor receptor pathway.37 Nevertheless, an increase in the MO1 subset had never been associated with a human disease. MO1s express high levels of CCR2, the receptor of the cytokine MCP-1, whereas CD16+ monocytes express high levels of the fractalkine receptor CX3CR1.9 The expression of these 2 surface markers distinguishes the 3 monocyte subsets in a manner similar to CD14 and CD16. A loss of CD16 expression was described in paroxysmal nocturnal hemoglobinuria38 and in patients with a genetic polymorphism.39 Because the increased fraction of MO1s in CMML patients was detected with the CCR2/CX3CR1 combination, it may not be related to an altered regulation of CD16 expression in the context of monocyte dysplasia.40 This accumulation of MO1s could indicate the abnormal differentiation of specific monocyte subsets, as observed in Nr4a1−/− mice.41
CMML-associated monocyte dysplasia can be difficult to assess morphologically. We have shown previously that CMML cells identified morphologically as monocytes could include a variable fraction of immature granulocytes endowed with immunosuppressive properties.17 The aberrant expression of CD56 was shown to be a characteristic feature of monocyte dysplasia in a fraction of CMML patients, together with the decreased expression of HLA-DR and the aberrant expression of CD2.42-49 We observed an aberrant expression of CD56, CD62L, and CD115 on MO1s that accumulate in CMML patients. The dysplastic features of these cells were further indicated by the principal component analysis of gene expression that separated CMML from healthy donor cells. Interestingly, MO1s sorted from reactive monocytosis blood samples demonstrated a pattern of gene expression that was distinct from both healthy and CMML MO1s.
Mutations in epigenetic modifying enzymes such as TET2 and ASXL1 are highly prevalent in CMML20,50 and associated with DNA hypermethylation,51,52 whereas epigenetic extinction of specific genes such as TRIM33 might play a role in disease occurrence or progression.53 We have shown that re-expression of TRIM33 could be used as a biomarker of response to the nucleoside analog decitabine.53 Here, we show that normalization of the monocyte subset repartition in the peripheral blood is another biomarker of response to demethylating drugs. Flow cytometry analysis of monocyte subsets might be useful to monitor the efficacy of other therapeutic approaches tested in CMML.
Although the diagnostic hallmark of CMML is blood monocytosis for ≥3 months, the reliable identification of CMML can become challenging when dysplasia is not prominent. Identification of clonal genetic abnormalities can support CMML diagnosis in these confounding situations, but none is specific. Given its simplicity and robustness, the flow cytometry demonstration of an increased fraction of MO1s may become an essential argument for CMML diagnosis and replace the 3-month delay currently recommended by the WHO to diagnose this disease.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors are indebted to Claude Gardin (Bobigny), Didier Bouscary (Cochin, Paris), Andrea Toma (Créteil), Gérard Tertian (Le Kremlin-Bicêtre), Agnès Guerci (Nancy), Aspasia Stamatoullas (Rouen), and Stéphane de Botton (Villejuif), who provided patient samples; and Marc Deloger, who analyzed gene expression data generated by A-sequencing.
This work was supported by the Ligue Nationale Contre le Cancer (Equipe labellisée) and by grants from the French National Cancer Institute and the Hospital Clinical Research Program (MAD06 and MONOMAC) (E.S. team). D.S.-B. received a postdoctoral fellowship from the Fondation de France.
Authorship
Contribution: D.S-B. designed and performed the experiments, analyzed the results, and wrote the manuscript; O.W-B. designed and performed the experiments and wrote the manuscript; V.S., V.B., L.B., C.D., and E.B. performed the experiments; M.M. performed the sample collection; E.M. collected patient information; R.I., A-M.N., P.F., T.B., C.W., B.Q., L.A., and M.F. provided samples; P.R. performed the cell sorting and analyzed the results; N.D. designed and performed the experiments and supervised the genotyping and RNA sequencing analysis; S.K. performed the statistical analysis, analyzed the results, and wrote the manuscript; and E.S. provided samples, analyzed the results, supervised the work, and wrote the manuscript. All authors approved the final manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Eric Solary, INSERM UMR 1009, Gustave Roussy, 114, Rue Edouard Vaillant, 94805 Villejuif, France; e-mail: eric.solary@gustaveroussy.fr.