Key Points
Dominant unit infused viable CD34+ cell dose determines engraftment after double-unit CBT.
Postthaw CD34+ cell recovery and viability are strongly associated with differences in CB banking practices.
Abstract
We investigated the unit characteristics associated with engraftment after double-unit cord blood (CB) transplantation (dCBT) and whether these could be reliably identified during unit selection. Cumulative incidence of neutrophil engraftment in 129 myeloablative dCBT recipients was 95% (95% confidence interval: 90-98%). When precryopreservation characteristics were analyzed, the dominant unit CD34+ cell dose was the only characteristic independently associated with engraftment (hazard ratio, 1.43; P = .002). When postthaw characteristics were also included, only dominant unit infused viable CD34+ cell dose independently predicted engraftment (hazard ratio, 1.95; P < .001). We then examined the determinants of infused viable CD34+ cell dose (precryopreservation count, postthaw recovery, and postthaw viability) in 402 units thawed at our center. This revealed close correlation between precryopreservation and postthaw CD34+ cell counts (r2 = 0.73). Median CD34+ cell recovery was 101%, although it ranged from 12% to 1480%. Notably, units from non–Netcord Foundation for the Accreditation of Cellular Therapy (Netcord-FACT)–accredited banks were more likely to have low recovery (P < .001). Furthermore, although median postthaw CD34+ cell viability was 92%, 33 (8%) units had <75% viable CD34+ cells. Units from non–Netcord-FACT–accredited banks and units with cryovolumes other than 24.5 to 26.0 mL were more likely to have poor postthaw viability. Precryopreservation CD34+ cell dose and banking practices should be incorporated into CB unit selection.
Introduction
Unrelated donor cord blood (CB) is an established source of hematopoietic stem cells for allogeneic transplantation. Disease-free survival after CB transplantation (CBT) is now comparable to other alternative adult donor allograft sources.1-5 However, impaired engraftment remains a significant problem after single-unit CBT.6,7 Double-unit CBT has extended application to adult patients,8,9 although graft failure and delayed engraftment have not been eliminated and contribute to transplant-related mortality (TRM).1 In the absence of widely applicable strategies to enhance CBT engraftment (by ex vivo expansion,10,11 promotion of homing,12 or addition of third party CD34+ cells,13,14 for example), the ability to accurately predict the engraftment potential or potency of CB units from the information provided by CB banks is vital to successful CBT.
CB banks report unit precryopreservation (prefreeze) total nucleated cell (TNC) counts and precryopreservation progenitor cell counts as measured by CD34+ cells and/or colony-forming units (CFUs). In single-unit CBT, multiple studies have demonstrated associations between prefreeze TNC dose and engraftment.7,15-17 Some have observed that prefreeze CFUs18 or CD34+ cell dose19 is superior to TNC in predicting engraftment. Transplant center analyses of single-unit CBT have shown that postthaw CFU20 and CD34+ cell dose6,21 measurements may be superior to postthaw TNC dose measurements in predicting engraftment. However, postthaw doses are only available at the time of unit infusion and cannot be used for unit selection. Furthermore, CFU and CD34+ cell assays are thought to be subject to significant interlaboratory variation.22,23 In double-unit CBT, postthaw CD34+ cell viability has been associated with unit dominance and engraftment,24,25 although this measurement is also not available at the time of unit selection. Testing of thawed cells from segments attached to the cryopreserved CB unit may be informative but has yet to be standardized.26
Thus, the prethaw TNC count is currently the only standardized, reproducible, and widely accepted measurement of CB unit cell dose that is available at the time of graft selection, and for this reason, it is currently the only cell dose measurement used by the US Food and Drug Administration to define CB potency. However, this measurement may not the best predictor of CB engraftment potential. With the aim of optimizing unit selection, we first sought to identify which laboratory measurements of CB unit cell content and quality are most closely associated with neutrophil engraftment in a cohort of myeloablative double-unit CBT recipients at our institution. Having identified the best surrogate for CB potency in this cohort, we then determined whether this measurement was associated with CB unit information provided by CB banks at the time of unit selection in a subsequent analysis of all CB units thawed at our center.
Methods
Patients and engraftment
During the study period, all patients with hematologic malignancies undergoing CBT received double-unit grafts. Consecutive patients who underwent myeloablative double-unit CBT as their first allograft for the treatment of acute leukemia in morphologic remission (or aplasia), myelodysplasia, myeloproliferative diseases, or high-risk lymphoid malignancies between October 2005 and June 2013 were eligible for the analysis of engraftment (n = 129). Patients signed informed consent for the collection and analysis of CBT outcomes in accordance with the Declaration of Helsinki. Permission to use clinical and laboratory information was obtained from the Memorial Sloan-Kettering Cancer Center (MSKCC) Institutional Review/Privacy Board. Sixty-one of the patients have been reported on previously.25 Conditioning was predominantly fludarabine and total body irradiation based as previously described,25,27-29 although a small cohort of pediatric patients received chemotherapy-only preparative regimens. A calcineurin inhibitor and mycophenolate mofetil were used for graft-versus-host disease prophylaxis.27,29 Granulocyte-colony-stimulating factor (5 μg/kg/day rounded to vial size) was given after transplant to promote neutrophil recovery.
The cumulative incidence of sustained neutrophil engraftment was our clinical study end point. The day of sustained neutrophil engraftment was defined as the first of 3 consecutive days with absolute neutrophil count ≥0.5 × 109/L without secondary graft failure and with total donor chimerism >90%. Donor chimerism was determined on marrow and blood after transplantation as previously described.30 The dominant unit was the only one detected or the CB unit that was dominant in serial testing. This could be assigned based on bone marrow analysis even if the patient had clinical graft failure (lack of sustained neutrophil recovery ≥ 0.5 × 109/L).
CB unit selection
The primary criteria used in unit selection were cryopreserved TNC dose and donor-recipient HLA-A, -B antigen, and -DRB1 allele match as previously described.31 Units that were red blood cell (RBC) depleted were given priority, and units cryopreserved in vials instead of bags were not considered. High-resolution HLA allele match was considered in unit selection from July 2012. CD34+ cell dose reported by the bank was not considered in unit selection.
CB unit thaw and postthaw cell counts
All CB units included in this analysis (n = 402) were shipped frozen to MSKCC in liquid nitrogen vapor phase shippers and arrived in satisfactory condition with documentation that no increase in temperature to >−150°C had occurred during transit. Units were kept at ≤−180°C until thawing and were then thawed and diluted with albumin-dextran (n = 355) or were washed (n = 47) prior to infusion according to MSKCC-validated procedures.28 Patients with body weight ≤20 kg only received washed CB units. Units frozen in multiple bags were combined after thawing into a single product for infusion. Cell counts and viability were performed in duplicate on aliquots of the final thawed CB product.
Assays for enumeration of CB cell populations and determination of postthaw viability have been previously described in detail.24 Briefly, total nucleated cells were enumerated on an automated hematology analyzer (Advia 2120i; Siemens, Washington, DC) and CD34+ cells and CD3+ cells were enumerated by flow cytometry (FACSCalibur; Becton Dickinson, Franklin Lakes, NJ). Duplicate aliquots containing 0.5 × 106 CB cells were incubated with anti-CD45 fluorescein isothiocyanate (#340664; Becton Dickinson), anti-CD34 phycoerythrin (#IM1871; Beckman Coulter, Brea, CA), and anti-CD3 Ag-presenting cells (#340661; Becton Dickinson) at room temperature in the dark for 20 minutes. RBCs were lysed with fixative-free ammonium chloride. 7-amino-actinomycin D (7AAD) (#IM3422; Beckman Coulter) was then added. Samples were vortexed, kept at room temperature in the dark for 15 minutes, and then stored for <1 hour on wet ice in the dark until acquisition. As most units underwent albumin-dextran dilution and cells were not washed during the staining, dead cells were not removed at any step during sample preparation.
Flow cytometric evaluation was performed using the International Society of Hematotherapy and Graft Engineering gating strategy with several modifications that allowed the acquisition of both dead (7AAD-positive) and viable (7AAD-negative) cells as previously described24 (see supplemental Methods, available on the Blood Web site). Thus, the CD34+ cell viability was determined from the total debris-free population. Absolute viable CD34+ cell numbers were determined using the following equation: TNC × percentage of CD45+ cells that are viable × percentage of CD34+ cells in the sample. Viable CD3+ cell numbers were determined using a similar equation. Total CD34+ cell numbers were calculated using the following equation: viable CD34+ cell number ÷ percent CD34+ cell viability.
Statistical analysis
In a cohort of 129 myeloablative dCBT recipients, engraftment was analyzed as cumulative incidence with death prior to engraftment as the competing risk. The variables analyzed for a potential association with neutrophil engraftment included the following: recipient age, diagnosis, recipient cytomegalovirus serology, conditioning regimen intensity, dominant unit-recipient HLA allele match, dominant unit precryopreservation TNC and CD34+ cell doses, dominant unit postthaw TNC, infused viable CD34+ cell, infused viable CD3+ cell, and CFU doses. Univariate and multivariate associations were assessed using cause-specific Cox proportional hazards regression. All variables that reached P ≤ .05 on univariate analysis were included in the multivariate analysis. The nondominant unit was not considered in the engraftment analysis as a previous MSKCC study did not show that this unit’s characteristics influenced neutrophil recovery.25 In addition, determinants of unit dominance were not analyzed as this has been extensively investigated by our center24,25,32 and others8,33,34 and was not the purpose of this study.
For the comparisons of precryopreservation (bank) and postthaw (MSKCC) unit cell counts, all 402 units thawed at our center between October 2005 and June 2013 were analyzed. This included units thawed for the engraftment study described above (n = 258), as well as units thawed for other patients (predominantly recipients of nonmyeloablative conditioning, n = 144). Information on bank of origin, date of unit cryopreservation, processing method for RBC and/or plasma depletion, precryopreservation TNC and CD34+ cell counts, number of freezing bags per unit, and the total frozen volume of the cryopreserved units were extracted from bank reports. No analysis of bank precryopreservation CD34+ cell viability testing was possible as this information was not routinely provided in bank reports. For units cryopreserved in >1 bag, the average volume per bag was used for analysis. Postthaw parameters (TNC count, total CD34+, viable CD34+ and viable CD3+ cell counts, CD34+ cell viability, and CFUs) were obtained from MSKCC laboratory records. For washed units, only those with postthaw but prewash cell counts were included in comparisons with bank-reported counts. Total postthaw CD34+ cell counts were used for all comparisons with precryopreservation CD34+ cell counts.
To compare precryopreservation and postthaw measurements, correlations were assessed using Spearman’s rank correlation coefficient. Cell recoveries were calculated as the postthaw total count divided by the bank-reported precryopreservation cell count. A CD34+ cell recovery threshold of 65% was chosen to define units with low recovery for statistical analysis. Although any such threshold is arbitrary, 65% was chosen as it identified the lowest decile (10%) of CB units in this analysis. Postthaw CD34+ cell viability was analyzed by grouping units as ≥75% vs <75% viability because this threshold was associated with unit dominance and graft failure in previous MSKCC analyses.24,25 The significance of associations between prethaw unit characteristics and postthaw CD34+ cell recovery and viability were estimated using binary logistic regression. Significance for 2 × 2 contingency tables of categorical variables used Fisher’s exact test (2-tailed).
Results
Determinants of engraftment in myeloablative double-unit CBT recipients
The cumulative incidence of neutrophil engraftment by day 45 after CBT was 95% for the 129 myeloablative double-unit CBT recipients (95% confidence interval [CI]: 90-98%] at a median of 24 days (range, 12-43 days). One patient who died early after transplant was excluded from subsequent analysis because chimerism was not evaluated. In 128 evaluable patients (Table 1), a single dominant unit was identified after transplant. The characteristics of these dominant units are shown in Table 2. Recipient age and dominant unit precyropreservation TNC and CD34+ cell doses and infused TNC, infused viable CD34+ cell, CFUs, and viable CD3+ cell doses were all significantly associated with neutrophil engraftment in univariate analysis (Table 3). Disease category, recipient pretransplant cytomegalovirus serostatus, conditioning regimen, and dominant unit-recipient HLA allele match were not significantly associated.
Patient and graft characteristics of 128 recipients of myeloablative double-unit CBT (n = 256 units)
| Characteristics . | Value . |
|---|---|
| Median age, years (range) | 35 (0.9-69) |
| Children younger than 16 years | 31 (24%) |
| Median weight, kg (range) | 68 (8-116) |
| N (%) AML* | 60 (47%) |
| N (%) ALL† | 33 (26%) |
| N (%) MDS/MPD | 10 (8%) |
| N (%) NHL/CLL/HL | 25 (19%) |
| N (%) CMV serostatus of recipient | |
| Negative | 58 (45%) |
| Positive | 70 (55%) |
| N (%) conditioning intensity | |
| High-dose myeloablative‡ | 65 (51%) |
| Reduced intensity§ | 63 (49%) |
| Median infused TNC × 107/kg (range) | |
| Larger unit (n = 128) | 2.85 (1.46-12.79) |
| Smaller unit (n = 128) | 2.01 (0.91-7.09) |
| Median infused viable CD34+ cells × 105/kg (range) | |
| Larger unit (n = 128) | 1.30 (0.26-6.97) |
| Smaller unit (n = 128) | 0.68 (0.08-2.12) |
| N (%) cord unit-recipient HLA-A, -B, antigen, -DRB1 allele match¶ | |
| 6/6 | 12 (5%) |
| 5/6 | 118 (46%) |
| 4/6 | 126 (49%) |
| N (%) donor-recipient HLA-A, -B, -C, -DRB1, -DQB1 allele match¶ | |
| 8-10/10 | 46 (18%) |
| 6-7/10 | 102 (40%) |
| 2-5/10 | 108 (42%) |
| Characteristics . | Value . |
|---|---|
| Median age, years (range) | 35 (0.9-69) |
| Children younger than 16 years | 31 (24%) |
| Median weight, kg (range) | 68 (8-116) |
| N (%) AML* | 60 (47%) |
| N (%) ALL† | 33 (26%) |
| N (%) MDS/MPD | 10 (8%) |
| N (%) NHL/CLL/HL | 25 (19%) |
| N (%) CMV serostatus of recipient | |
| Negative | 58 (45%) |
| Positive | 70 (55%) |
| N (%) conditioning intensity | |
| High-dose myeloablative‡ | 65 (51%) |
| Reduced intensity§ | 63 (49%) |
| Median infused TNC × 107/kg (range) | |
| Larger unit (n = 128) | 2.85 (1.46-12.79) |
| Smaller unit (n = 128) | 2.01 (0.91-7.09) |
| Median infused viable CD34+ cells × 105/kg (range) | |
| Larger unit (n = 128) | 1.30 (0.26-6.97) |
| Smaller unit (n = 128) | 0.68 (0.08-2.12) |
| N (%) cord unit-recipient HLA-A, -B, antigen, -DRB1 allele match¶ | |
| 6/6 | 12 (5%) |
| 5/6 | 118 (46%) |
| 4/6 | 126 (49%) |
| N (%) donor-recipient HLA-A, -B, -C, -DRB1, -DQB1 allele match¶ | |
| 8-10/10 | 46 (18%) |
| 6-7/10 | 102 (40%) |
| 2-5/10 | 108 (42%) |
Of the 129 patient cohort, 1 died early without identification of a dominant unit and was excluded from further analysis. AML, acute myeloid leukemia; ALL, acute lymphoblastic leukemia; CLL, chronic lymphocytic leukemia; CMV, cytomegalovirus; HL, Hodgkin lymphoma; MDS, myelodysplastic syndrome; MPD, myeloproliferative disorder; NHL, non-Hodgkin lymphoma.
Includes 33 patients in first complete remission (CR1), 24 in CR2, 2 in CR3, and 1 in aplasia after chemotherapy.
Includes 19 patients in CR1, 8 in CR2, 5 in CR3, and 1 in CR4.
Includes 48 patients who received cyclophosphamide 120/fludarabine 75/total body irradiation 1320 to 1375; 11 patients who received clofarabine/melphalan/thiotepa, and 6 who received other regimens.
Regimens that were reduced intensity but functionally myeloablative including 55 patients who received cyclophosphamide 50/fludarabine 150/thiotepa 10/total body irradiation 400, and 8 heavily pretreated patients who received fludarabine 150/melphalan 140.
Reflects all 256 CB units infused.
HLA match and cell doses for the 128 dominant CB units
| Characteristics . | Value . |
|---|---|
| Donor-recipient HLA-A, -B, -C, -DRB1, -DQB1 allele match | |
| 8-9/10 | 29 (23%) |
| 6-7/10 | 54 (42%) |
| 2-5/10 | 45 (35%) |
| Cell dose, median (range) | |
| Prefreeze TNC × 107/kg | 2.78 (1.56-16.49) |
| Prefreeze CD34+ cells × 105/kg | 0.94 (0.07-8.95) |
| Infused TNC × 107/kg | 2.18 (0.91-12.79) |
| Infused total CD34+ cells × 105/kg | 1.00 (0.1-5.68) |
| Infused viable CD34+ cells × 105/kg | 0.92 (0.08-4.77) |
| Infused CFU × 104/kg | 2.60 (0.17-18.43) |
| Infused viable CD3+ cells × 106/kg | 4.27 (0.8-15.3) |
| Characteristics . | Value . |
|---|---|
| Donor-recipient HLA-A, -B, -C, -DRB1, -DQB1 allele match | |
| 8-9/10 | 29 (23%) |
| 6-7/10 | 54 (42%) |
| 2-5/10 | 45 (35%) |
| Cell dose, median (range) | |
| Prefreeze TNC × 107/kg | 2.78 (1.56-16.49) |
| Prefreeze CD34+ cells × 105/kg | 0.94 (0.07-8.95) |
| Infused TNC × 107/kg | 2.18 (0.91-12.79) |
| Infused total CD34+ cells × 105/kg | 1.00 (0.1-5.68) |
| Infused viable CD34+ cells × 105/kg | 0.92 (0.08-4.77) |
| Infused CFU × 104/kg | 2.60 (0.17-18.43) |
| Infused viable CD3+ cells × 106/kg | 4.27 (0.8-15.3) |
Univariate analysis of variables potentially associated with neutrophil engraftment in 128 myeloablative double-unit CBT recipients
| Variable . | Category . | HR (95%CI) . | P . |
|---|---|---|---|
| Recipient age (per decade) | 0.90 (0.82-0.99) | .03 | |
| Disease type | Myeloid | Reference | .15 |
| Lymphoid | 1.31 (0.91-1.88) | ||
| Recipient CMV serology | Negative | Reference | .18 |
| Positive | 1.27 (0.89-1.82) | ||
| Conditioning regimen | High-dose myeloablative | Reference | .49 |
| Reduced intensity* | 1.13 (0.80-1.62) | ||
| HLA allele match to recipient† | 8-9/10 | Reference | .98 |
| 6-7/10 | 1.05 (0.66-1.67) | ||
| 2-5/10 | 1.02 (0.63-1.64) | ||
| Reported by bank prefreeze† | TNC dose × 107/kg | 1.19 (1.10-1.28) | <.001 |
| CD34+ cell dose × 105/kg | 1.39 (1.24-1.54) | <.001 | |
| Postthaw (infused) at MSKCC† | TNC dose × 107/kg | 1.28 (1.16-1.41) | <.001 |
| Viable CD34+ cell dose × 105/kg | 1.88 (1.58-2.24) | <.001 | |
| CFU × 104/kg | 1.08 (1.03-1.13) | .001 | |
| Viable CD3+ cell dose × 106/kg | 1.09 (1.02-1.16) | .006 | |
| Variable . | Category . | HR (95%CI) . | P . |
|---|---|---|---|
| Recipient age (per decade) | 0.90 (0.82-0.99) | .03 | |
| Disease type | Myeloid | Reference | .15 |
| Lymphoid | 1.31 (0.91-1.88) | ||
| Recipient CMV serology | Negative | Reference | .18 |
| Positive | 1.27 (0.89-1.82) | ||
| Conditioning regimen | High-dose myeloablative | Reference | .49 |
| Reduced intensity* | 1.13 (0.80-1.62) | ||
| HLA allele match to recipient† | 8-9/10 | Reference | .98 |
| 6-7/10 | 1.05 (0.66-1.67) | ||
| 2-5/10 | 1.02 (0.63-1.64) | ||
| Reported by bank prefreeze† | TNC dose × 107/kg | 1.19 (1.10-1.28) | <.001 |
| CD34+ cell dose × 105/kg | 1.39 (1.24-1.54) | <.001 | |
| Postthaw (infused) at MSKCC† | TNC dose × 107/kg | 1.28 (1.16-1.41) | <.001 |
| Viable CD34+ cell dose × 105/kg | 1.88 (1.58-2.24) | <.001 | |
| CFU × 104/kg | 1.08 (1.03-1.13) | .001 | |
| Viable CD3+ cell dose × 106/kg | 1.09 (1.02-1.16) | .006 | |
Conditioning was functionally myeloablative.
Dominant unit.
In multivariate analysis that included only precryopreservation cell doses and recipient age, the bank-reported precryopreservation CD34+ cell dose was the only independent predictor of neutrophil engraftment (hazard ratio [HR], 1.43; 95% CI: 1.14-1.80; P = .002). When postthaw infused cell doses of the dominant unit were also included (all variables with P < .05 in Table 3), only infused viable CD34+ cell dose was independently associated with neutrophil engraftment (HR, 1.95; 95% CI: 1.30-2.90; P < .001). Neutrophil engraftment displayed by quartiles of dominant unit infused viable CD34+ cell dose is shown in Figure 1. The median time to engraftment was 19 days (range, 12-33 days) for the highest viable CD34+ cell dose quartile (>1.4 × 105/kg) vs 31 days (range, 21-43 days) for the lowest (<0.5 × 105/kg). Five recipients had dominant units with <75% viable CD34+ cells; 1 failed to engraft, and engraftment in the others was delayed (range, 31-43 days).
Sustained neutrophil engraftment after myeloablative double-unit CBT by infused viable CD34+ cell dose per kilogram of the dominant unit (n = 128). Neutrophil engraftment was significantly associated with the dominant unit infused viable CD34+ cell dose.
Sustained neutrophil engraftment after myeloablative double-unit CBT by infused viable CD34+ cell dose per kilogram of the dominant unit (n = 128). Neutrophil engraftment was significantly associated with the dominant unit infused viable CD34+ cell dose.
Characteristics of 402 CB units thawed at MSKCC
To determine whether unit characteristics associated with the infused viable CD34+ cell dose could be identified at the time of unit selection, all 402 CB units thawed at our center were then analyzed. The units originated from 43 banks, including 302 units from 15 US banks and 100 units from 28 non-US banks. Most units (350/402; 87%) were from banks accredited by Netcord Foundation for the Accreditation of Cellular Therapy (Netcord-FACT). The proportion of units from Netcord-FACT–accredited banks was similar for US (261/302; 86%) and non-US (89/100; 89%) units. Thirty-six CB units were cryopreserved in two 24.5- to 26.0-mL bags, 1 unit was in 2 bags of <24.5 mL each, 30 units were in 2 bags with >26.0 mL each, and 4 units were in 3 bags (each bag < 24.5 mL). Most units were RBC depleted (396/402; 99%).
Comparison of bank-reported precryopreservation CD34+ cell counts with postthaw values (CD34+ cell correlation and recovery)
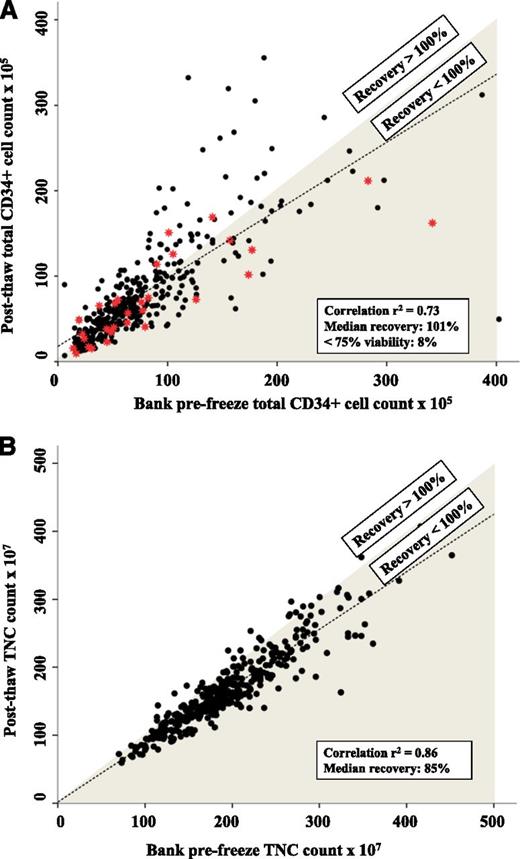
There was a strong correlation between the bank’s precryopreservation total CD34+ cell count and the MSKCC postthaw total CD34+ cell count overall (r2 = 0.73; Figure 2A), but significant variation between banks was observed (r2 = 0.44-0.96; Table 4). Seven banks accounting for 279 units (74%) showed very close correlation with MSKCC total CD34+ cell counts (r2 > 0.80). Correlation was better for CB units from banks that were accredited by Netcord-FACT (r2 = 0.80) than those from banks that were not (r2 = 0.63). There was also better correlation for more recent CB units (cryopreserved in 2005-2012, r2 = 0.77) than for earlier units (1997-2004, r2 = 0.65).
Comparison of prefreeze vs postthaw cell counts to demonstrate the correlation between bank and MSKCC measurements and the postthaw recovery. (A) Comparison of prefreeze CD34+ cell count reported by the bank with the postthaw CD34+ cell count measured at MSKCC. The MSKCC total CD34+ cell counts are shown (not adjusted for postthaw viability). The line of best fit is shown as a dashed line. CB units in the shaded region had <100% recovery postthaw. Red stars represent CB units with postthaw CD34+ cell viability <75%. (B) Comparison of prefreeze TNC count reported by the bank and the postthaw TNC count measured at MSKCC. The correlation between bank and postthaw MSKCC TNC count is stronger than for CD34+ cell count.
Comparison of prefreeze vs postthaw cell counts to demonstrate the correlation between bank and MSKCC measurements and the postthaw recovery. (A) Comparison of prefreeze CD34+ cell count reported by the bank with the postthaw CD34+ cell count measured at MSKCC. The MSKCC total CD34+ cell counts are shown (not adjusted for postthaw viability). The line of best fit is shown as a dashed line. CB units in the shaded region had <100% recovery postthaw. Red stars represent CB units with postthaw CD34+ cell viability <75%. (B) Comparison of prefreeze TNC count reported by the bank and the postthaw TNC count measured at MSKCC. The correlation between bank and postthaw MSKCC TNC count is stronger than for CD34+ cell count.
Correlation between bank prefreeze and MSKCC postthaw total CD34+ cell counts, CD34+ cell recovery, and postthaw CD34+ cell viability by bank grouped according to the number of CB units thawed
| Bank by number of units thawed . | Bank vs MSKCC total CD34+ cell count correlation* . | Median % CD34+ cell count recovery postthaw (range)* . | Percent with <75% viable CD34+ cells postthaw† . |
|---|---|---|---|
| ≥20 units each | |||
| Bank A | r2 = 0.82 | 99% (46-156) | 9% |
| Bank B | r2 = 0.81 | 115% (48-280) | 2% |
| Bank C | r2 = 0.96 | 72% (55-89) | 0% |
| 10-19 units each | |||
| Bank D | r2 = 0.85 | 122% (88-189) | 0% |
| Bank E | r2 = 0.44 | 73% (44-108) | 6% |
| Bank F | r2 = 0.56 | 87% (38-127) | 54% |
| Bank G | r2 = 0.83 | 90% (58-140) | 6% |
| Bank H | r2 = 0.62 | 109% (58-252) | 7% |
| Bank I | r2 = 0.56 | 100% (12-137) | 0% |
| Bank J | r2 = 0.52 | 96% (62-169) | 0% |
| 5-9 units each | |||
| Bank K | r2 = 0.81 | 111% (75-156) | 20% |
| Bank L | r2 = 0.56 | 57% (42-106) | 0% |
| Bank M | r2 = 0.81 | 93% (62-149) | 20% |
| 1-4 units each | |||
| Other (29 banks) | r2 = 0.68 | 87% (47-1480) | 25% |
| Bank by number of units thawed . | Bank vs MSKCC total CD34+ cell count correlation* . | Median % CD34+ cell count recovery postthaw (range)* . | Percent with <75% viable CD34+ cells postthaw† . |
|---|---|---|---|
| ≥20 units each | |||
| Bank A | r2 = 0.82 | 99% (46-156) | 9% |
| Bank B | r2 = 0.81 | 115% (48-280) | 2% |
| Bank C | r2 = 0.96 | 72% (55-89) | 0% |
| 10-19 units each | |||
| Bank D | r2 = 0.85 | 122% (88-189) | 0% |
| Bank E | r2 = 0.44 | 73% (44-108) | 6% |
| Bank F | r2 = 0.56 | 87% (38-127) | 54% |
| Bank G | r2 = 0.83 | 90% (58-140) | 6% |
| Bank H | r2 = 0.62 | 109% (58-252) | 7% |
| Bank I | r2 = 0.56 | 100% (12-137) | 0% |
| Bank J | r2 = 0.52 | 96% (62-169) | 0% |
| 5-9 units each | |||
| Bank K | r2 = 0.81 | 111% (75-156) | 20% |
| Bank L | r2 = 0.56 | 57% (42-106) | 0% |
| Bank M | r2 = 0.81 | 93% (62-149) | 20% |
| 1-4 units each | |||
| Other (29 banks) | r2 = 0.68 | 87% (47-1480) | 25% |
n = 361 CB units as 41 units were excluded due to missing prewash CD34+ cell count (n = 40) or missing bank CD34+ cell count (n = 1).
n = 402 CB units.
The median CD34+ cell recovery postthaw was 101% but varied substantially (range, 12-1480; mean, 110%; standard deviation [SD], ±82%). CD34+ cell recovery was <65% in 38 units (11%) and >150% in 44 units (12%). Recovery varied by bank of origin (Table 4). On univariate analysis, units from non–Netcord-FACT–accredited banks and those with a cryopreservation volume <24.5 or >26.0 mL were more likely to have low postthaw recovery (<65%) (supplemental Table 1). There was no association between low CD34+ cell recovery and whether the unit was from a US or non-US bank (P = .112), duration of frozen storage (analyzed in quartiles, P = .823), year of cryopreservation (1997-2004 vs 2005-2012, P = .096), or processing method (manual vs automated/semiautomated, P = .717). By multivariate analysis, only lack of bank Netcord-FACT accreditation was independently associated with low CD34+ cell recovery (supplemental Table 1). High CD34+ cell recovery (>150%) was not associated with any of these unit characteristics (data not shown).
Comparison of bank-reported precryopreservation TNC counts with postthaw counts (TNC and CD34+ cells)
We also investigated the prefreeze and postthaw TNC correlation and recovery for comparison with that of CD34+ cells. The correlation between precryopreservation and postthaw TNC counts was stronger (r2 = 0.86; Figure 2B) than the CD34+ cell correlation and, unlike CD34+ cells, was more consistently strong across individual CB banks (supplemental Table 2). The median TNC recovery was 85% (range, 50-125%; mean, 86%; SD, ±10%) and was more consistent between banks than was CD34+ cell recovery, ranging from 78% to 100% (supplemental Table 2). However, the correlation between the precryopreservation TNC count and the postthaw total CD34+ cell count (r2 = 0.34) was weak and notably worse than the correlation between precryopreservation and postthaw CD34+ cell counts (r2 = 0.73).
Postthaw CD34+ cell viability
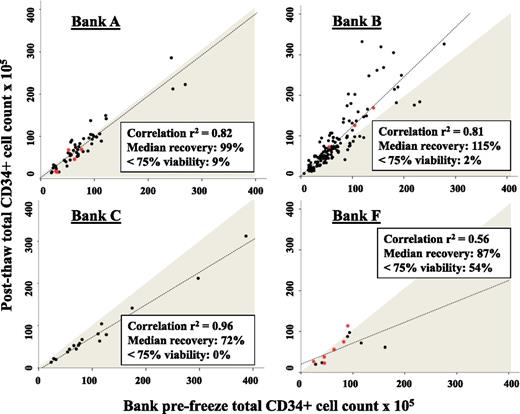
The median percentage of viable CD34+ cells postthaw was 92% and ranged from 34% to 99% (mean, 89%; SD, ±11%). Thirty-three CB units (8%) had <75% viable CD34+ cells (Figures 2A and 3). The frequency of units with <75% viability varied substantially by CB bank (Table 4). Higher frequency of poor viability was associated on univariate analysis with units from banks that were not Netcord-FACT accredited, were cryopreserved before 2005, had cryopreservation volume <24.5 or >26.0 mL, or had been processed by the CB bank using manual RBC and/or plasma reduction techniques (Table 5). Although the measurements are independent of each other, poor viability was associated with poor CD34+ cell recovery. Among units with <65% recovery, 23% had CD34+ cell viability <75% compared with only 7% of units with better recovery (P = .003). Viability was not associated with duration of cryopreservation (analyzed in quartiles, P = .530), whether the unit was from a US or non-US bank (P = .740), the shipping distance (New York vs Australia, for example, P = .503), or the number of cryopreservation bags (single vs multiple, P = .189). By multivariate analysis, Bank Netcord-FACT accreditation and cryopreservation volume were strongly and independently associated with viability, whereas processing method and year of cryopreservation were not significant (Table 5).
Comparison of prefreeze vs postthaw CD34+ cell counts to demonstrate the bank-MSKCC CD34+ cell count correlation, recovery, and postthaw viability for selected banks. Banks are labelled as per Table 4. The line of best fit is shown as a dashed line, CB units in the shaded region had less than 100% recovery postthaw, and red stars represent CB units with postthaw CD34+ cell viability <75%. CB units from Bank A had close Bank-MSKCC correlation and almost 100% recovery but a significant percentage had poor postthaw viability. CB units from Bank B had high recovery and few units had poor viability. CB units from Bank C had close Bank-MSKCC correlation, all units had good viability but recovery was low. Units from Bank F had both poor Bank-MSKCC correlation and low postthaw viability.
Comparison of prefreeze vs postthaw CD34+ cell counts to demonstrate the bank-MSKCC CD34+ cell count correlation, recovery, and postthaw viability for selected banks. Banks are labelled as per Table 4. The line of best fit is shown as a dashed line, CB units in the shaded region had less than 100% recovery postthaw, and red stars represent CB units with postthaw CD34+ cell viability <75%. CB units from Bank A had close Bank-MSKCC correlation and almost 100% recovery but a significant percentage had poor postthaw viability. CB units from Bank B had high recovery and few units had poor viability. CB units from Bank C had close Bank-MSKCC correlation, all units had good viability but recovery was low. Units from Bank F had both poor Bank-MSKCC correlation and low postthaw viability.
Variables associated with low postthaw CD34+ cell viability
| Variable . | N units . | N with <75% CD34+ cell viability (%) . | Univariate analysis . | Multivariate analysis . | ||
|---|---|---|---|---|---|---|
| Odds ratio (95% CI) . | P . | Odds ratio (95% CI) . | P . | |||
| Cord blood bank Netcord-FACT accreditation | ||||||
| Yes | 350 | 15 (4%) | Reference | <.001 | Reference | .002 |
| No | 52 | 18 (35%) | 11.8 (5.5-25.6) | 4.9 (1.8-13.3) | ||
| Year of cryopreservation | ||||||
| 1997-2004 | 119 | 17 (14%) | 2.8 (1.4-5.7) | .005 | 1.47 (0.6-3.7) | .408 |
| 2005-2012 | 283 | 16 (6%) | Reference | Reference | ||
| Cryopreserved volume, mL | ||||||
| <24.5 | 14 | 5 (36%) | 20.1 (5.5-73.9) | <.001 | 8.8 (1.9-41.7) | <.001 |
| 24.5-26.0 | 298 | 8 (3%) | Reference | Reference | ||
| 26.1-29.9 | 45 | 7 (16%) | 6.7 (2.3-19.5) | 8.5 (2.6-28.0) | ||
| ≥30.0 | 45 | 13 (29%) | 14.7 (5.7-38.2) | 7.5 (2.5-22.0) | ||
| Method of processing | ||||||
| Manual | 187 | 24 (13%) | 3.4 (1.5-7.5) | .003 | 2.3 (0.8-6.5) | .131 |
| Automated and semiautomated* | 215 | 9 (4%) | Reference | Reference | ||
| Variable . | N units . | N with <75% CD34+ cell viability (%) . | Univariate analysis . | Multivariate analysis . | ||
|---|---|---|---|---|---|---|
| Odds ratio (95% CI) . | P . | Odds ratio (95% CI) . | P . | |||
| Cord blood bank Netcord-FACT accreditation | ||||||
| Yes | 350 | 15 (4%) | Reference | <.001 | Reference | .002 |
| No | 52 | 18 (35%) | 11.8 (5.5-25.6) | 4.9 (1.8-13.3) | ||
| Year of cryopreservation | ||||||
| 1997-2004 | 119 | 17 (14%) | 2.8 (1.4-5.7) | .005 | 1.47 (0.6-3.7) | .408 |
| 2005-2012 | 283 | 16 (6%) | Reference | Reference | ||
| Cryopreserved volume, mL | ||||||
| <24.5 | 14 | 5 (36%) | 20.1 (5.5-73.9) | <.001 | 8.8 (1.9-41.7) | <.001 |
| 24.5-26.0 | 298 | 8 (3%) | Reference | Reference | ||
| 26.1-29.9 | 45 | 7 (16%) | 6.7 (2.3-19.5) | 8.5 (2.6-28.0) | ||
| ≥30.0 | 45 | 13 (29%) | 14.7 (5.7-38.2) | 7.5 (2.5-22.0) | ||
| Method of processing | ||||||
| Manual | 187 | 24 (13%) | 3.4 (1.5-7.5) | .003 | 2.3 (0.8-6.5) | .131 |
| Automated and semiautomated* | 215 | 9 (4%) | Reference | Reference | ||
Specific techniques: AutoXpress Platform (AXP) (n = 82), Sepax (n = 102), Optipress (n = 27), Compomat (n = 3), and Biotrans Separator (n = 1).
Combined assessment of individual CB banks for postthaw CD34+ cell count correlation, recovery, and viability
Among the 43 CB banks that contributed units for this analysis, 13 banks supplied 5 or more units to MSKCC. The performance of these banks as assessed by postthaw CD34+ cell correlation, recovery, and viability varied considerably. As shown in Table 4 and illustrated by 4 examples in Figure 3, some banks consistently provided CB units with optimal CD34+ cell count correlation, recovery, and viability, whereas others provided units with none of these. Notably, high bank-MSKCC CD34+ cell count correlation was not necessarily associated with optimal CD34+ cell recovery. For example, units from bank C (Table 4; Figure 3) had the strongest Bank-MSKCC CD34+ cell count correlation (r2 = 0.96) but a relatively low median postthaw CD34+ cell recovery (72%; range, 55-89%).
Effect of banking practice on neutrophil engraftment
Having identified the association between Netcord-FACT accreditation and postthaw CD34+ cell recovery, and between both Netcord-FACT accreditation and cryopreservation volume and postthaw CD34+ cell viability in the 402 unit analysis, we then investigated whether these characteristics in the dominant CB unit were associated with neutrophil engraftment in the cohort of 129 myeloablative dCBT recipients. Both lack of Netcord-FACT accreditation and cryopreservation volume <24.5 or >26.0 mL were associated with a reduced cumulative incidence of neutrophil engraftment on univariate analysis (HR, 0.42; 95% CI: 0.21-0.84; P = .014 and HR, 0.65; 95% CI: 0.43-1.00; P = .048, respectively). In multivariate analysis adjusting for precryopreservation CD34+ cell dose, Netcord-FACT accreditation remained independently associated with neutrophil engraftment (HR, 0.45 for units from nonaccredited banks; 95% CI: 0.22-0.93; P = .032), whereas cryopreservation volume did not (HR, 0.80 for cryovolume <24.5 or >26.0 mL; 95% CI: 0.51-1.25; P = .329).
Discussion
In this study, the infused viable CD34+ cell dose of the dominant unit was the most critical determinant of neutrophil engraftment in recipients of myeloablative double-unit CBT. To our knowledge, our center is the first to report that the dominant unit infused viable CD34+ cell dose is an independent determinant of engraftment after double-unit CBT, and this finding is consistent with reports of single-unit CBT.6,21 Thus, whereas CD34+ cell enumeration assays are not as well standardized as those for TNC (as reflected in the lower correlations between bank and MSKCC CD34+ cell counts compared with TNC counts in the 402 units analyzed in this study), CD34+ cell dose (whether measured precryopreservation or postthaw) was a more accurate measure of unit potency than TNC dose as determined by clinical effectiveness (neutrophil engraftment). In addition, the correlation between precryopreservation TNC and postthaw CD34+ cell count was considerably weaker than that observed between precryopreservation and postthaw CD34+ cell counts. Moreover, the close correlations we observed between prefreeze and postthaw CD34+ cell measurements for units from many banks support previous reports that reproducibility within laboratories35 and between laboratories36 can be achieved.
Further critical novel findings of the 402 unit analysis were that the key determinants of infused viable CD34+ cell dose (ie, recovery and viability) were associated with information that was available at the time of unit selection and that poor unit quality (low postthaw recovery and viability) relates to variations in bank practices. Specifically, units from banks that were not Netcord-FACT accredited were more likely to have a low CD34+ cell recovery than units from accredited banks. CB units from nonaccredited banks were also more likely to have low CD34+ cell viability. Accreditation requires compliance with Netcord-FACT standards for CB collection, laboratory testing, processing methods, cryopreservation, storage, and shipping, with adherence to protocols, validation of procedures, and on-site verification. Our study provides indirect evidence that the practices of nonaccredited banks may not be as consistent as those of accredited banks, with the consequence that the quality of their units is variable and sometimes compromised. Moreover, the observation that significant deviation from the standard 25 mL cryopreservation volume (<24.5 or >26.0 mL) was associated with poor viability is direct evidence that bank practices affect CB unit quality. This may be mediated by alterations in cryoprotectant concentration and cooling rate in units with nonstandard volumes.37-39
Inaccuracies in MSKCC laboratory measurements might account for the observed variations in Bank-MSKCC CD34+ cell correlation, postthaw recovery, and postthaw viability, but this is unlikely for several reasons. First, that the infused viable CD34+ cell dose was a better predictor of neutrophil engraftment than the precryopreservation CD34+ cell dose provides evidence that the postthaw measurement was the more accurate estimate of progenitor cell content. Second, aberrant postthaw CD34+ cell recovery and viability were not distributed randomly between banks but rather followed discernible patterns, with low or high recovery and low viability occurring with increased frequency in units from specific banks. Furthermore, this variation in postthaw recovery and viability also correlated with specific bank practices.
Our findings warrant further investigation and have significant implications for CB banking and unit selection. CB banks should conform to Netcord-FACT standards. The specific practices that are the most important determinants of postthaw CB unit quality need to be further characterized. Factors not available to transplant centers such as the maximal permitted time from collection to processing, for example, could have an impact on quality. This and other banking procedures may be critical to postthaw recovery and viability. Furthermore, hundreds of millions of dollars have been spent establishing CB banks worldwide, and the global public inventory now surpasses 600 000 CB units.40 However, the size of the inventory of quality CB units may be considerably lower. Finally, current guidelines regarding CB unit selection emphasize the importance of precryopreservation TNC.31,41 Our results indicate that despite assay standardization issues, consideration of precryopreservation CD34+ cell dose should be incorporated into unit selection criteria.
In conclusion, CD34+ cell dose and factors that are associated with unit quality now emerge as additional criteria for unit selection. At our center, to optimize postthaw cell dose and quality, we now prioritize (1) prefreeze CD34+ cell dose over TNC dose among units above an arbitrary TNC threshold of 1.5 × 107/kg and a CD34+ cell threshold of 0.7 × 105/kg; (2) units from Netcord-FACT–accredited banks to optimize CD34+ cell recovery and viability; and (3) units with a cryopreserved volume between 24.5 and 26.0 mL to optimize viability. Choosing the best CB unit by these criteria for single-unit CBT or the 2 best units available for double-unit CBT is a cost-effective strategy to optimize the speed and success of CB engraftment. How CD34+ cell dose should be weighed against high-resolution, HLA-A, -B, -C, -DRB1 match in unit selection strategies will be an important question for future studies.
Finally, because no bank can guarantee optimal cell count and quality postthaw, transplant centers must be able to react to a lower than expected postthaw CD34+ cell dose and/or low CD34+ cell viability. Therefore, we recommend that centers use methods to measure the infused viable CD34+ cell dose on transplant day (or another rapidly available measure of potency) and have a backup strategy in place in case of a compromised CB unit.42 This is even more important in single-unit CBT in which, unlike double-unit CBT, engraftment is solely dependent on the engraftment potential of the single unit graft.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the staff of the CB Banks who provided additional information for this analysis.
This work was supported in part by the Haematology Society of Australia and New Zealand (D.P.), the Gabrielle’s Angel Foundation for Cancer Research (J.N.B.), the MSKCC (J.N.B.), the Translational and Integrative Medicine research grant (J.N.B.), and National Cancer Institute grant P01 CA23766 (J.N.B.).
Authorship
Contribution: D.P., A.S., C.E.S., and J.N.B. analyzed and interpreted the data and wrote the manuscript; K.S. and J.T. performed laboratory analyses; S.D., R.M., S.G., N.A.K., and D.M.P. wrote the manuscript; and M.L. analyzed data.
Conflict-of-interest disclosure: A.S. is a joint employee of MSKCC and the New York Blood Center. The remaining authors declare no competing financial interests.
Correspondence: Juliet N. Barker, Box 259, 1275 York Ave, New York, NY 10065; e-mail: barkerj@mskcc.org.