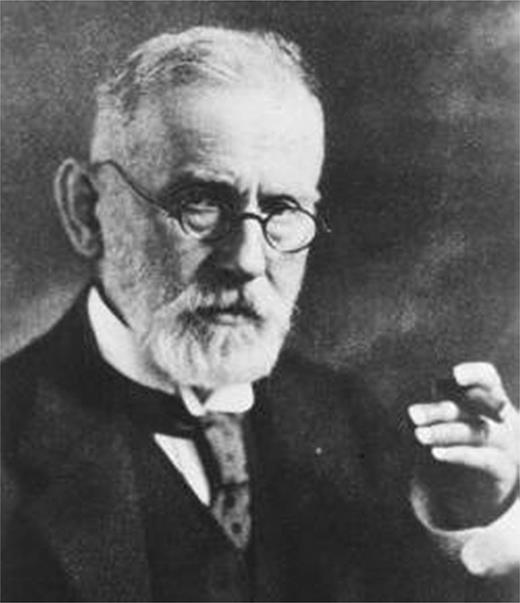
Inspired by his work with antiserum to prevent and treat infectious disease, Paul Ehrlich (see figure) envisioned a day when molecules could be fashioned to specifically bind rogue cells and equipped with a toxic moiety to mediate cell death. The magischen Kugeln or “magic bullets” first conceptualized by Ehrlich at the turn of the 20th century remain a holy grail for cancer researchers in search of targeted therapeutics that kill the tumor and spare the host.
Ehrlich’s theoretical notion took a major leap forward in 1975, when George J. F. Köhler and César Milstein fused splenocytes from immunized mice with murine myeloma cells and discovered that such fusions created an unlimited supply of antibodies with a single, definable specificity, also termed monoclonal antibodies (mAbs).1 Despite enthusiasm among the scientific and lay community that this invention would rapidly translate into “magic bullets” to treat cancer, it soon became clear that hurdles remained to be scaled if murine mAbs were to be effective cancer therapeutics. Murine mAbs are highly immunogenic and often induce allergic reactions and neutralizing anti-antibody responses. Murine mAbs are also poor inducers of complement-mediated cytotoxicity and antibody-dependent cell-mediated cytotoxicity by human effector cells.2 Gradually, with advances in molecular cloning and improved understanding of immunobiology, these hurdles were overcome, and the anti-CD20 mAb rituximab and anti-HER2 mAb trastuzumab were the first 2 mAbs approved for the treatment of cancer in 1997 and 1998, respectively. Despite their status as blockbuster drugs and the impressive increases in survival rates observed when these agents were combined with cytotoxic regimens, neither rituximab nor trastuzumab induced regression of established tumors when administered as single agents.3 The “magic bullet” as envisioned by Ehrlich was not yet realized.
Progress in the development of antibody-derived therapeutics has continued since the 1990s and numerous other mAbs have now been approved for the treatment of cancer and other diseases.2 Using modern phage-display technologies, fully human mAbs can now be created to target essentially any conceivable protein with variable epitope specificity, affinity, and subclass. Still, however, naked mAbs that rely solely on the induction of naturally occurring effector mechanisms have yet to demonstrate potent, reproducible single-agent activity against established cancer. To increase potency, it is now common practice to isolate the binding moiety of mAbs, most commonly in the form of a single-chain variable fragment (scFv) and link these molecules, chemically or genetically, to a variety of toxic partners. Progress in the engineering of such antibody-derived therapeutics is moving at an impressive pace, and the last 5 years have seen substantial advances in the march toward the development of “magic bullets.”
In this series, “Antibody Derivatives as New Therapeutics for Hematologic Malignancies,” a variety of antibody-derived therapeutics that currently show promise for the treatment of hematologic malignancies are described and reviewed in depth. Drs Maria Palanca-Wessels and Oliver Press (from the Fred Hutchinson Cancer Center) provide a review of radioconjugates and antibody drug conjugates. Two radioconjugates, ibritumomab and tositumomab, both targeting CD20 have already been approved by the US Food and Drug Administration (FDA) for non-Hodgkin lymphoma, and another antibody drug conjugate (brentuximab vedotin, which targets CD30) is FDA approved for the treatment of Hodgkin disease. The authors review novel radioconjugates currently under study, describe new approaches to optimize tumor targeting based upon preadministration of nonradiolabeled antibody, and discuss current challenges facing clinical application of radioconjugates that have limited widespread use of these agents following FDA approval. The authors also review the current status of the rapidly moving field of antibody drug conjugates for hematologic malignancies, including advances in linker technology that have accelerated clinical development of this class of therapeutics, and opened an array of new possibilities for future applications.
Unlike antibody drug conjugates and radioconjugates, which must be chemically linked to the mAb-derived binding moiety, genetic engineering can link mAbs with naturally occurring cytotoxic proteins derived from microorganisms to create immunotoxins. In this series, Dr Alan Wayne (of the Children’s Hospital of Los Angeles, The Norris Comprehensive Cancer Center, and Keck School of Medicine, University of Southern California) and Drs David FitzGerald, Robert Kreitman, and Ira Pastan (of the National Cancer Institute) review the current status of the development of antibodies linked to diphtheria toxin, Pseudomonas exotoxin A, and ricin to target hematologic malignancies. The authors review agents currently in clinical trials and discuss mechanisms of resistance and clinical results thus far. They also describe advances from the last 5 years that have substantially improved the activity (including new approaches to augment specificity and potency) to diminish immunogenicity and to overcome challenges in production of these agents.
In the final review of this series, Drs Marcela Maus, Stephen Grupp, David Porter, and Carl June (from the University of Pennsylvania) describe the recent impressive activity of chimeric antigen receptor–based therapies for hematologic malignancies. Briefly, chimeric antigen receptors are genetically engineered to encode one protein comprising an mAb-derived binding moiety, a transmembrane domain, a CD3 ζ signaling domain plus an endodomain from a T-cell costimulatory molecule. Genes encoding for the engineered receptors are stably integrated into the DNA of mature T cells, most commonly using viral-based vectors, and such modified autologous T cells are administered to patients with cancer. In the setting of several hematologic malignancies, including B precursor acute lymphoblastic leukemia, the administration of T cells genetically engineered to express chimeric antigen receptors has induced dramatic antitumor effects. This is the first approach to effectively harness the benefits of humoral and cellular immunity into a single therapeutic. Chimeric antigen receptors combine the exquisite binding specificity of antibodies to target cell-surface receptors in a major histocompatibility complex–unrestricted fashion with the potent expansion and killing capacity of human T cells. The authors review results of reported clinical trials thus far and discuss some of the challenges facing this novel therapy, including toxicities observed and complexities associated with large-scale cell manufacturing.
In summary, the search for “magic bullets” that can potently eradicate cancer without damaging normal tissues continues unabated. Just as Ehrlich was inspired by his work with antiserum, the modern scientific community continues to work from the fundamental premise that antibody-based binding, or binding mediated by an antibody derivative, provides the first essential ingredient needed for a “magic bullet.” Which, if any, toxic moiety will ultimately prove superior remains to be seen, but the recent promising results presented in this series suggest that with a little luck, our patients may have an array of ammunition to target their hematologic malignancies in the coming years.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal