Abstract
Abstract 332
PURPOSE: In Multiple Myeloma (MM), the combination of serum beta-2-microglobulin level with serum albumin concentration has been proposed as an outcome predictor in the International Staging System (ISS). More recently, subgroups of MM defined by genetic and cytogenetic abnormalities have been associated with unique biologic, clinical, and prognostic features.
PATIENTS AND METHODS: We analyzed the prognostic value of 12 chromosomal abnormalities by fluorescent in situ hybridization (FISH) in a series of 354 MM patients treated within the HOVON-65/GMMG-HD4 trial. Patients with newly diagnosed MM were randomized to receive either three cycles of VAD (arm A; vincristine, adriamycin, dexamethasone) or PAD (arm B; bortezomib, adriamycin, dexamethasone). All patients underwent autologous stem cell transplantation (ASCT) followed by maintenance therapy with thalidomide 50 mg daily (arm A) or bortezomib 1.3 mg/m2 once every 2 weeks (arm B), respectively. In addition, a second cohort of patients was analyzed as a control group (n=462), undergoing ASCT at the University of Heidelberg between September 1994 and December 2010.
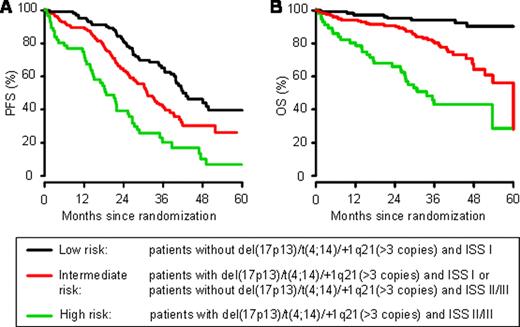
RESULTS: For the entire group of patients treated within the HOVON-65/GMMG-HD4 trial, we identified 233 patients with 2 copies (67.7%), 95 patients with 3 copies (27.6%) and 16 patients (4.7%) with more than three copies of the chromosomal region 1q21. In addition to del(17p13) and t(4;14), we added +1q21 (>3 copies) to the group of high-risk aberrations, since the outcome of these patients was almost as poor as it was observed for patients with del(17p13). Subsequently, we analyzed whether combining the ISS score with information on the presence of high-risk aberrations could improve the prognostic value with regard to patients' outcome. A combination of the presence or absence of del(17p13), t(4;14), or +1q21 (>3 copies) with the ISS score allowed patients to be stratified into three distinct groups: low-risk [absence of del(17p13)/t(4;14)/+1q21 (>3 copies) and ISS I], high-risk [presence of del(17p13)/t(4;14)/+1q21 (>3 copies) and ISS II/III], and intermediate-risk (all remaining patients). Most of the patients belonged to the low- (33%) and intermediate-risk (49%) groups, whereas 18% were allocated to the high-risk group. The median PFS times for the low-, intermediate-, and high-risk groups were 41.9 months, 31.1 months (HR=1.7; p=0.0018) and 18.7 months (HR=3.6; p<0.0001), respectively. The 3yr-overall survival (OS) decreased from 94% in the low-risk group to 80% (HR=4.6; p=0.0001) and 43% (HR=12.8; p<0.0001) in the intermediate- and high-risk groups, respectively.
These results were confirmed in the independent cohort of patients: From date of first ASCT, the median PFS times for the low-, intermediate-, and high-risk groups were 43.3 months, 23.0 months (HR=1.5; p=0.015) and 13.8 months (HR=2.4; p=0.0003), respectively. The 4yr-OS decreased from 84% in the low-risk group to 71% (HR=2.1; p=0.0043) and 49% (HR=3.84; p<0.0001) in the intermediate- and high-risk groups, respectively.
van de Velde:Ortho Biotech Oncology Research & Development: Employment. Sonneveld:Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen-Cilag: Membership on an entity's Board of Directors or advisory committees, Research Funding; Onyx: Membership on an entity's Board of Directors or advisory committees, Research Funding; Millennium: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal