Abstract
Abstract 3068
Abnormal cytokine expression accompanies the disease process in primary myelofibrosis (PMF) and the levels of proinflammatory cytokines have been shown to be down-regulated by JAK inhibitor therapy. The prognostic relevance of increased cytokine levels in PMF has not been systematically studied. The objectives of the current study were to describe the spectrum of abnormal cytokine expression in PMF and determine its prognostic relevance.
A multiplex biometric sandwich immunoassay (Invitrogen multiplex assays, Invitrogen Corporation-Carlsbad CA, USA) was used for simultaneous analysis of 30 cytokine levels. Diluted plasma was mixed with fluorescently addressed microbeads bound with anti-cytokine antibodies. Biotin anticytokine secondary antibodies were then added and allowed to bind to cytokine-bead complexes. Total surface fluorescence for each bead was then measured using a Luminex (Luminex Corporation, Austin, TX, USA) fluorescent flow-based detection system.
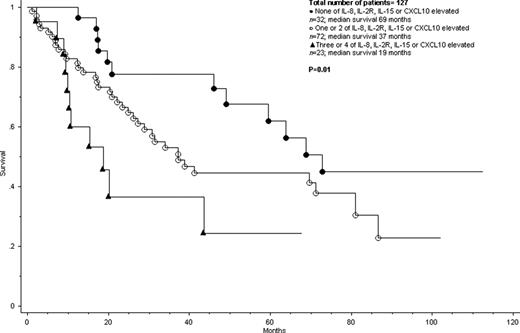
Cytokine levels at diagnosis were analyzed for a total of 127 treatment naïve patients with PMF, who had stored sera at the time of diagnosis or first referral to the Mayo Clinic. The circulating levels of 30 cytokines in the multiplex assay were compared between PMF patients (n=127) and normal controls (n=31). Significant differences (p<0.05) were evident for 20 of the 30 cytokines: IL-1b, IL-1RA, IL-2R,IL-6, IL-8, IL-10, IL-12, IL-13, IL- 15, TNF-α, G-CSF, INF-α, INF-γ, MIP-1α, MIP-1β, HGF, CXCL10, MIG, MCP-1 and VEGF. On univariate analysis, increased levels of 9 of these 20 cytokines were associated with shortened survival (p<0.05): IL-1RA, IL-2R, IL-6, IL-8, IL-12, IL-15, MIP-1α, CXCL10 and MIG. On multivariable analysis, 4 of these 9 cytokines maintained their prognostic value for survival: IL-2R (p=0.0011), IL-8 (p<0.0001), IL-15 (p=0.0124) and CXCL10 (p=0.0031). The independent prognostic value of these 4 cytokines was sustained during additional multivariable analysis that included the Dynamic International Prognostic System Score and cytogenetic risk category. Next, we divided the 127 patients into three cytokine risk categories based on the serum levels of IL-2R, IL-8, IL-15 and CXCL10: none elevated, one or two elevated and three or four elevated. The respective median survivals were 69, 37 and 19 months (p=0.01; Figure 1) and such cytokine risk categorization was both DIPSS and cytogenetic risk independent; p values for multivariable analysis including cytokine, DIPSS, cytogenetic risk groups were 0.02, 0.0001 and 0.004, respectively.
Elevated serum levels of IL-2R, IL-8, IL- 15 and CXCL10 independently predict shortened survival in PMF and such prognostication appears to be independent of DIPSS and cytogenetic risk category. The current study suggests clinical relevance of multiple cytokines in PMF that could be therapeutically targeted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.