Abstract
The t(4;14) translocation occurs frequently in multiple myeloma (MM) and results in the simultaneous dysregulated expression of 2 potential oncogenes, FGFR3 (fibroblast growth factor receptor 3) from der(14) and multiple myeloma SET domain protein/Wolf-Hirschhorn syndrome candidate gene 1 from der(4). It is now shown that myeloma cells carrying a t(4;14) translocation express a functional FGFR3 that in some cases is constitutively activated by the same mutations that cause thanatophoric dysplasia. As with activating mutations of K-ras and N-ras, which are reported in approximately 40% of patients with MM, activating mutations ofFGFR3 occur during tumor progression. However, the constitutive activation of ras and FGFR3 does not occur in the same myeloma cells. Thus the activated forms of these proteins appear to share an overlapping role in tumor progression, suggesting that they also share the signaling cascade. Consistent with this prediction, it is shown that activated FGFR3—when expressed at levels similar to those seen in t(4;14) myeloma—is an oncogene that acts through the MAP kinase pathway to transform NIH 3T3 cells, which can then generate tumors in nude mice. Thus,FGFR3, when overexpressed in MM, may be not only oncogenic when stimulated by FGF ligands in the bone marrow microenvironment, but is also a target for activating mutations that enable FGFR3to play a ras-like role in tumor progression.
Introduction
Chromosomal translocations to the immunoglobulin heavy-chain (IgH) locus on chromosome 14q32 are the hallmark of many B-cell malignancies, and their characterization has led to the identification of critical dysregulated oncogenes (eg, c-myc, bcl-2, cyclin D1) that play a key role in the pathogenesis of these diseases. In contrast, conventional cytogenetics failed to identify recurrent translocations in patients with multiple myeloma (MM). Recently, we developed a molecular approach and identified frequent IgH translocations in MM.1 Three chromosome loci are most frequently involved—11q13, 16q23, and 4p16—with the consequent dysregulation of cyclin D1, c-maf, and fibroblast growth factor receptor 3 (FGFR3),respectively.2-4
In particular, we previously reported that the novel, karyotypically silent t(4;14)(p16;q32) translocation occurs in approximately 20% of MM cells and tumors.4 More recently, others5,6 have confirmed a high incidence of t(4;14)(p16;q32) translocation in patients with MM. As a result of this translocation, the expression of 2 genes at the 4p16.3 locus is dysregulated. The expression of FGFR3 is dysregulated by juxtaposition to the 3′ Cα enhancer on der(14), whereas multiple myeloma SET domain protein/Wolf-Hirschhorn syndrome candidate gene 1 (MMSET/WHSC1) is dysregulated by association with the intronic enhancer (Eμ) on der(4).7 It remains unclear how each of these dysregulated genes contributes to the pathogenesis of MM.
FGFR3 is one of 4 high-affinity tyrosine kinase receptors for the FGF family of ligands. It is normally expressed in the lungs and kidneys, and it is expressed at high levels in the developing central nervous system, precursor bone cartilage rudiments, and resting cartilage at the end of growing bones.8 We found that it is undetectable by Northern blot or Western blot analysis in mononuclear cells isolated from the bone marrow or the blood, suggesting a very low level of expression in B-cell lineage.4 On ligand stimulation, FGFR3 undergoes dimerization and tyrosine autophosphorylation, resulting in cell proliferation or differentiation, depending on the cell context, through the mitogen-activated protein kinase (MAPK) and phospholipase Cγ signal transduction pathways.9
Constitutive activation of FGFR3 by germline point mutations is the major cause of dwarfism, with the severity of the phenotype directly proportional to the degree of activation of the receptor.10-12 These mutations may occur in differentFGFR3 domains: the extracellular Ig-like domain, the transmembrane domain, and the tyrosine kinase domain. We previously reported that the same activating mutations that cause thanatophoric dysplasia (TD), the most severe and lethal form of dwarfism, are present in 2 of 5 MM cell lines and in one of 3 primary tumors that have a t(4;14) translocation.4 The phenotype observed in dwarfism suggests that the dysregulation of FGFR3 activity in the tissues in which it is normally expressed could impair cell growth and differentiation.13-15 On the other hand, we have recently transduced an IL-6–dependent murine plasmacytoma cell with a retrovirus expressing FGFR3, and we have shown that we can replace IL-6 dependence with FGF1 dependence. We also showed that interfering with FGFR3 signaling by removing FGF1 causes MM cell apoptosis.16 The current study explores whether the ectopic expression of an activated signaling molecule, such as the FGFR3, could lead to malignant transformation. In particular the oncogenic role of FGFR3 dysregulation in MM is analyzed by characterization of the genetic anatomy of myeloma cells and by studying the consequences of ectopic expression of FGFR3 and its mutated forms found in MM.
Materials and methods
Cell culture
The human MM cell lines, as described in detail previously, were grown in Petri dishes in RPMI 1640 medium supplemented with 10% fetal calf serum (Biowhittaker, Walkersville, MD).1,17-20 They were all Epstein-Barr virus-negative by polymerase chain reaction (PCR) or Southern blot analysis. OPM1 and OPM2 are 2 cell lines established independently from the same myeloma patient.21 The MM5.2 cell line is a subclone of the stroma-dependent MM5.1 lines that has become stroma independent.22 PE1 has been established in our laboratory from a patient with MM. NIH 3T3 cells were purchased from ATCC and maintained in DMEM medium supplemented with 10% calf serum (Biowhittaker).
Immunofluorescence staining
Approximately 20 000 cells were seeded by cytospin onto glass slides and fixed for 10 minutes in 4% formaldehyde in phosphate-buffered saline (PBS). Blocking with 5% milk in PBS was followed by incubation with a rabbit antiserum specific for the N-term of FGFR3 (sc-9007; Santa Cruz Biotechnology, Santa Cruz, CA) and with goat antirabbit IgG fluorescein isothiocyanate (FITC)–conjugated secondary antibody (Sigma, St Louis, MO), both at 1:200 dilution in blocking solution. After counterstaining the cell nuclei with DAPI (Pierce, Rockford, IL), the slides were covered with Vectashield mounting solution (Vector, Burlingame, CA) and imaged.
Flow cytometry
Nonpermeabilized cells were incubated with rabbit anti-FGFR3 (see above) or rabbit preimmune serum (SER-RB100l; Stressgen, Victoria, Canada) at a 1:100 dilution for 1 hour at 4°C. After washing with ice-cold PBS–0.5% BSA (Sigma), FITC-conjugated goat antirabbit IgG (see above) was added to the cells at a 1:200 dilution and incubated for 30 minutes at 4°C. The cells were washed and fixed in PBS with 1% formalin (Sigma), and the samples were analyzed on a FACSCalibur flow cytometer (Becton Dickinson, Franklin Lakes, NJ).
MAPK analysis
MM cells were starved for 48 hours in RPMI 0% serum. Fresh RPMI 0% serum was added 2 hours before stimulation. Cells were stimulated with aFGF (R&D Systems, Minneapolis, MN) at 10 ng/mL and heparin (Sigma) at 10 μg/mL for 10 minutes at 37°C, washed in PBS, and lysed in sodium dodecyl sulfate (SDS) sample buffer. Total protein extracts obtained were separated by electrophoresis through a 12% SDS-PAGE (polyacrylamide gel electrophoresis) gel and transferred to nitrocellulose. The filter was incubated with phospho-p44/42 MAPK antibody (New England Biolabs, Beverly, MA) and horseradish peroxidase-conjugated goat antirabbit IgG (Santa Cruz Biotechnology) and was developed with the ECL Western blotting detection reagent (Amersham, Arlington Heights, IL). After stripping, the filter was reincubated with ERK2 goat antibody and horseradish peroxidase-conjugated goat antigoat IgG (Santa Cruz Biotechnology). Densitometric analysis was performed, and the levels of phospho-MAPK were normalized to those of ERK2.
Detection of FGFR3 and ras mutation
The 4 FGFR3 regions—extracellular (EC) domain, transmembrane (TM) domain, tyrosine kinase (TK) domain, and stop codon (SC)—known to be hot spots for activating mutations, were amplified by reverse transcription (RT)–PCR in the following manner (Figure 2). A first RT-PCR reaction was performed using oligonucleotides o201 and o202 to amplify a 668-bp region containing EC and TM. Similarly, another RT-PCR reaction was performed using the primer pair o5724-o5725 to amplify a 636–base pair (bp) region containing TK and SC. The products of the first PCR reactions were then re-amplified with 4 nested PCR reactions to obtain 4 fragments corresponding to the EC (primer pair o5666-o5706, 117 bp), TM (primer pair o5580-o202, 442 bp), TK (primer pair o5724-o5703, 120 bp), and SC (primer pair o66-o5725, 313 bp). Each PCR fragment was then directly sequenced (Thermo Sequenase–radiolabeled terminator cycle sequencing kit; Amersham) or analyzed by single-strand conformation polymorphism (SSCP). The oligonucleotides used for each reaction are as follows (listed in 5′-3′ orientations): o201, AAC TAC ACC TGC GTC GTG GAG AAC; o202, CTC CCC TGA GGA CAG CCT TGC GAT; o5724, ATG AAG ATC GCA GAC TTC GGG; o5725, ATC TGC ACT GAG TCT CAT GCC; o5666, CGG CAG ACG TAC ACG CTG; o5706, CTT GCA GTG GAA CTC CAC GTC; o5580, GCG CTA ACA CCA CCG ACA AG; o5703, GTA GAC TCG GTC AAA CAA GGC; and o66, CTC CCA GAG GCC AAC CTT CAA GCA G.
A region spanning codons 12, 13, and 61 of human N-ras and K-ras was amplified by RT-PCR from MM cell lines using these primer pairs: ATG ACT GAG TAC AAA CTG GTG GTG GTT GGA and CAA ATG ACT TGC TAT TAT TGA TG for N-ras, and GGC CTG CTG AAA ATG ACT GAA TA and CCC ACC TAT AAT GGT GAA TAT CT for K-ras. The PCR product was than run through an SSCP gel or directly sequenced.
Vector construction
The full-length FGFR3 cDNAs, wild type and containing the K650E mutations, were obtained from Daniel J. Donoghue (University of California, San Diego, CA). They were excised from the pCDNA3 vector by restriction digestion with HindIII and XbaI and inserted into pCEFL vector digested with HindIII andXbaI to obtain the FGFR3 wild-type and K650E vector, respectively. The F384L and Y373C mutant forms of FGFR3 were amplified by RT-PCR from LP1 and KMS11 cDNA, respectively, using primer pairs CGG CAG ACG TAC ACG CTG and TTG CAG GTG TCG AAG GAG TAG TC. The amplified products were digested with Eco47III and XhoI, and the obtained 627-bp bands were cloned into pCEFL/FGFR3 vectors to replace the corresponding fragment. Similarly, the MM5.1 deletion mutant was obtained by RT-PCR amplification using the primers AAG AAG ACA ACC AAC GGC CG and GTC AGG AGA CCG TTG CAC AGC. The PCR product was digested with SphI and KpnI, and the obtained 400-bp fragment was subcloned into pCEFL/FGFR3 vector to obtain the Δ795-808 FGFR3 vector. RasV12, RasN17, and Raf301 vectors were kindly provided by Silvio Gutkin (National Institutes of Health, Bethesda, MD).
Focus formation assay
Approximately 105 NIH 3T3 cells were plated onto 10-cm plates 24 hours before calcium phosphate precipitation transfection. A total amount of plasmid plus carrier DNA equal to 35 μg was used. Sixteen to 24 hours after transfection, cells were washed in PBS and incubated in the presence or absence of 750 μg/mL Geneticin (Gibco-BRL, Rockville, MD). The culture medium was then replaced every 2 days. In some cases, 0.5 and 5 ng/mL aFGF was added to the medium. Serial dilutions of neomycin-resistant cells were performed to measure the efficiency of transfection. Twelve to 14 days after transfection the plates were methanol fixed, stained with Wright staining (Sigma), and scored for the presence of cellular foci. Every transfection was conducted on triplicate plates, and at least 3 independent transfection experiments were performed.
Tumorigenesis in nude mice
NIH 3T3 cells were plated onto 10-cm dishes and transfected by calcium phosphate with 1 μg pCEFL, wild-type FGFR3, or K650E FGFR3. Transfectant cells were kept under neomycin selection and expanded for 3 passages only. To avoid spontaneous transformation, they were never allowed to reach confluent growth. Cells were then trypsinized, washed in PBS, and counted. Three different cell amounts—105, 3 × 105, and 9 × 105—were used for the injections. Six-week-old athymic nude mice (Harlan, Indianapolis, IN) received simultaneously 3 subcutaneous injections into their superior (pCEFL on the right and K650 on the left) and inferior (wild-type FGFR3) right flanks with each of the 3 types of transfected cells, resuspended in 200 μL PBS. Each experiment was conducted in triplicate. Two control mice did not receive any injection. The tumor was removed, formalin fixed, and stained with hematoxylin and eosin.
Other procedures
Results
The t(4;14) translocation induces ectopic expression of a fully functional FGFR3 in MM
We previously characterized the t(4;14) translocation in 5 of 21 MM lines and 3 of 10 primary MM tumors.4 Taking advantage of our hybrid mRNA transcript RT-PCR assay for the rapid detection of the t(4;14) translocation,7 we have now screened additional MM cell lines and primary MM tumors. Four (LP1, MM5.1/2, KHM11, and Karpas 1272) of these 9 cell lines and 4 of the 19 tumors have the t(4;14) translocation (Table 1). Together with our previous results, 9 of 30 (30%) MM cell lines and 7 of 29 (24%) tumors have a t(4;14) translocation. Immunofluorescence analysis on MM lines shows perfect correlation between the presence of the t(4;14) translocation and the expression of FGFR3. Figure1A shows a representative example ofFGFR3 expression on the plasma membrane of OPM2 myeloma cell line with a t(4;14)(p16;q32) but not in the control Delta-47 line that does not have a t(4;14) translocation and does not express FGFR3.In addition, FGFR3 can be detected on the surfaces of these cells by flow cytometric analysis (Figure 1B).
FGFR3 and ras mutations in multiple myeloma cell lines
| . | Line . | t(4;14) . | FGFR3 . | FGFR3 cd mut . | nt Change . | N,K-ras cd mut . | nt Change . |
|---|---|---|---|---|---|---|---|
| 1 | UTMC2 | + | + | No | − | No | − |
| 2 | LP1 | + | + | F384L | TTC > CTC | No | − |
| 3 | KMS11 | + | + | Y373C | TAT > TGT | No | − |
| 4 | MM5.1/2 | + | + | Δ* | deletion | No | − |
| 5a | OPM2 | + | + | K650E | AAG > GAG | No | − |
| 5b | OPM1 | + | + | K650E | AAG > GAG | K71 − Q >* | CAG > TAG |
| 6 | H929 | + | + | No | − | N13 − G > D | GGT > GAT |
| 7 | JIM3 | + | − | No | − | K12 − G > D | GGT > GAT |
| 8 | KHM11 | + | + | No | − | N61 − Q > K | CAA > AAA |
| 9 | Karpas1272 | + | + | No | − | K61 − Q > H | CAA > CAC |
| 10 | 8226 | − | − | ND | − | K12 − G > A | GGT > GCT |
| 11 | ARK | − | − | ND | − | N61 − Q > R | CAA > CGA |
| 12 | EJM | − | − | ND | − | K12 − G > A | GGT > GCT |
| 13 | Karpas620 | − | − | ND | − | K12 − G > D | GGT > GAT |
| 14 | KMM1 | − | − | ND | − | N13 − G > D | GGT > GAT |
| 15 | L363 | − | − | ND | − | N61 − Q > H | CAA > CAC |
| 16 | MM1.144 | − | − | ND | − | K12 − G > A | GGT > GCT |
| 17 | MM.S1 | − | − | ND | − | N12 − G > D | GGT > GAT |
| 18 | SKMM1 | − | − | ND | − | N12 − G > D | GGT > GAT |
| 19 | DELTA 47 | − | − | ND | − | No | − |
| 20 | FLAM 76 | − | − | ND | − | No | − |
| 21 | FR4 | − | − | ND | − | No | − |
| 22 | H1112 | − | − | ND | − | No | − |
| 23 | JJN3 | − | − | ND | − | No | − |
| 24 | KMS12 | − | − | ND | − | No | − |
| 25 | ANBL6 | − | − | ND | − | No | − |
| 26 | OCI-MY5 | − | − | ND | − | No | − |
| 27 | PE1 | − | − | ND | − | No | − |
| 28 | SKMM2 | − | − | ND | − | No | − |
| 29 | TH | − | − | ND | − | No | − |
| 30 | U266 | − | − | ND | − | No | − |
| . | Line . | t(4;14) . | FGFR3 . | FGFR3 cd mut . | nt Change . | N,K-ras cd mut . | nt Change . |
|---|---|---|---|---|---|---|---|
| 1 | UTMC2 | + | + | No | − | No | − |
| 2 | LP1 | + | + | F384L | TTC > CTC | No | − |
| 3 | KMS11 | + | + | Y373C | TAT > TGT | No | − |
| 4 | MM5.1/2 | + | + | Δ* | deletion | No | − |
| 5a | OPM2 | + | + | K650E | AAG > GAG | No | − |
| 5b | OPM1 | + | + | K650E | AAG > GAG | K71 − Q >* | CAG > TAG |
| 6 | H929 | + | + | No | − | N13 − G > D | GGT > GAT |
| 7 | JIM3 | + | − | No | − | K12 − G > D | GGT > GAT |
| 8 | KHM11 | + | + | No | − | N61 − Q > K | CAA > AAA |
| 9 | Karpas1272 | + | + | No | − | K61 − Q > H | CAA > CAC |
| 10 | 8226 | − | − | ND | − | K12 − G > A | GGT > GCT |
| 11 | ARK | − | − | ND | − | N61 − Q > R | CAA > CGA |
| 12 | EJM | − | − | ND | − | K12 − G > A | GGT > GCT |
| 13 | Karpas620 | − | − | ND | − | K12 − G > D | GGT > GAT |
| 14 | KMM1 | − | − | ND | − | N13 − G > D | GGT > GAT |
| 15 | L363 | − | − | ND | − | N61 − Q > H | CAA > CAC |
| 16 | MM1.144 | − | − | ND | − | K12 − G > A | GGT > GCT |
| 17 | MM.S1 | − | − | ND | − | N12 − G > D | GGT > GAT |
| 18 | SKMM1 | − | − | ND | − | N12 − G > D | GGT > GAT |
| 19 | DELTA 47 | − | − | ND | − | No | − |
| 20 | FLAM 76 | − | − | ND | − | No | − |
| 21 | FR4 | − | − | ND | − | No | − |
| 22 | H1112 | − | − | ND | − | No | − |
| 23 | JJN3 | − | − | ND | − | No | − |
| 24 | KMS12 | − | − | ND | − | No | − |
| 25 | ANBL6 | − | − | ND | − | No | − |
| 26 | OCI-MY5 | − | − | ND | − | No | − |
| 27 | PE1 | − | − | ND | − | No | − |
| 28 | SKMM2 | − | − | ND | − | No | − |
| 29 | TH | − | − | ND | − | No | − |
| 30 | U266 | − | − | ND | − | No | − |
MM indicates multiple myeloma; *, stop codon; Δ*, deletion of the stop codon; ND, not determined.
At the top of the table are listed the MM cell lines (1-9) that have a t(4;14) translocation and therefore express FGFR3. JIM3 does not express FGFR3, but the original tumor sample from which the cell line was derived does.4 At the bottom of the table are shown the MM lines (10-30) that do not have a t(4;14) translocation and therefore do not express FGFR3. Shaded are the activating mutations in FGFR3 or N,K-ras. Note that the F384L FGFR3 mutation in LP1 and the K71 Ras mutation in OPM1 are not activating (and are not shaded).
A functional FGFR3 is ectopically expressed in t(4;14) myeloma cells.
(A) Delta-47, with no t(4;14) translocation, and OPM2 cells, with a t(4;14) translocation, have been stained by indirect immunofluorescence using rabbit polyclonal anti-FGFR3 primary antibody and goat antirabbit IgG FITC-conjugated secondary antibody (green signal), both at 1:200 dilution. Cell nuclei have been counterstained with DAPI (blue signal). (B) Flow cytometric analysis of nonpermeabilized OPM2 cells was performed on staining with anti-FGFR3 antibodies (gray line) or rabbit preimmune serum control (black curve), followed by secondary FITC-conjugated goat antirabbit IgG. Results shown represent fluorescent cells after gating on live cells. (C) aFGF induces ERK1 and ERK2 phosphorylation in MM cells expressing FGFR3. MM cells with no (KMS12) or with (LP1, KMS11, H929) t(4;14) translocation were starved for 48 hours and then stimulated for 10 minutes with 10 ng/mL aFGF in the presence of 10 μg/mL heparin. Cell lysates were analyzed by Western blot using anti–phospho-p42/p44 MAPK antibody. As loading control, the same blot was stripped and reprobed with anti-p42 MAPK antibody. The intensity of each phospho-MAPK band was measured and normalized against the p42 loading control, and the fold induction of phospho-MAPK was calculated as shown in the graph.
A functional FGFR3 is ectopically expressed in t(4;14) myeloma cells.
(A) Delta-47, with no t(4;14) translocation, and OPM2 cells, with a t(4;14) translocation, have been stained by indirect immunofluorescence using rabbit polyclonal anti-FGFR3 primary antibody and goat antirabbit IgG FITC-conjugated secondary antibody (green signal), both at 1:200 dilution. Cell nuclei have been counterstained with DAPI (blue signal). (B) Flow cytometric analysis of nonpermeabilized OPM2 cells was performed on staining with anti-FGFR3 antibodies (gray line) or rabbit preimmune serum control (black curve), followed by secondary FITC-conjugated goat antirabbit IgG. Results shown represent fluorescent cells after gating on live cells. (C) aFGF induces ERK1 and ERK2 phosphorylation in MM cells expressing FGFR3. MM cells with no (KMS12) or with (LP1, KMS11, H929) t(4;14) translocation were starved for 48 hours and then stimulated for 10 minutes with 10 ng/mL aFGF in the presence of 10 μg/mL heparin. Cell lysates were analyzed by Western blot using anti–phospho-p42/p44 MAPK antibody. As loading control, the same blot was stripped and reprobed with anti-p42 MAPK antibody. The intensity of each phospho-MAPK band was measured and normalized against the p42 loading control, and the fold induction of phospho-MAPK was calculated as shown in the graph.
Stimulation of FGFR3 with the aFGF ligand results in activation of the MAPK signaling cascade. To determine whether the endogenous FGFR3 expressed by the t(4;14) myeloma cells is functional, we measured its ability to signal in the presence of ligand, leading to phosphorylation of the ERK1 and ERK2 members of the MAPK family. As shown in Figure 1C, no MAPK phosphorylation was detected either before or after stimulation with aFGF in the KMS12 myeloma cell line, which does not have a t(4;14) translocation and therefore does not express FGFR3.Conversely, stimulation with aFGF caused rapid MAPK phosphorylation in the t(4;14) LP1, KMS11, and H929 myeloma lines that did not express any other FGF receptors (except for a very low FGFR2 expression in KMS11 and FGFR4 expression in LP1, detectable only by 30 cycles of RT-PCR; data not shown), indicating that the t(4;14) translocation results in ectopic expression of a functional FGFR3in myeloma cells.
FGFR3 activating mutations are present in MM cells with t(4;14) translocation
Ectopic expression of signaling molecules that lead to proliferative responses, such as MAPK activation, could constitute a premalignant step in oncogenesis. Acquired mutations that dysregulate this signaling activity will be positively selected by the cells and may have oncogenic potential. This was clearly shown for proto-oncogenic receptors such as Her-2/neu.25
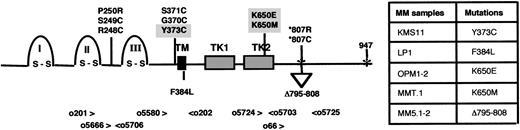
We previously reported that 2 of 5 MM cell lines and 1 of 3 MM tumors with the t(4;14) translocation have the same FGFR3activating mutations that, when inherited in the germline, cause thanatophoric dysplasia. Among the 4 additional independent MM cell lines with a t(4;14), one (MM5.1/MM5.2) has an FGFR3activating mutation. The related MM5.1 and MM5.2 myeloma lines carry an in-frame deletion of 42 bp (nucleotide [nt] 2421 to 2462) in the region spanning the FGFR3 stop codon, giving rise to a protein elongated by 99 amino acids (aa) (data not shown) (GenBankAF238374). A similarly elongated protein has been reported in patients with TD where a base substitution in the FGFR3 stop codon (codon 807) results in an mRNA that is translated through an additional 423 bp (141 aa) until the same in-frame stop codon (codon 947) is reached.26 Thus, of 9 independent MM lines with t(4;14) translocation, 3 have activating mutations of FGFR3 that are identical or similar to those reported in TD (Figure2, Table 1). In addition to theFGFR3 activating mutation, we also confirmed the presence in the LP1 MM line of an F384L mutation in the expressed FGFR3transmembrane domain (data not shown).27 As previously shown for OPM2 and KMS11, in all the 4 independent cell lines with an FGFR3 mutation, only the mutated FGFR3allele is expressed, consistent with the t(4;14) translocation causing the selective expression of the translocated allele. Unfortunately, we did not have primary tumor cells for any of the MM lines with activating mutations of FGFR3, so we were unable to determine directly whether the mutation is present in the primary tumor. However, in one case, 2 MM cell lines (OPM1 and OPM2) were generated independently from the same primary tumor sample. Because the K650E activating mutation is present in both the OPM1 and OPM2 MM cell lines, the mutation must have occurred in the primary MM tumor and not during propagation of the cells in culture (data not shown).
FGFR3 activating mutations in TD and MM.
Schematic representation of FGFR3 receptor, with the 3 Ig-like domains (I, II, and III), the transmembrane (TM) domain, and the 2 tyrosine kinase (TK) domains. At the top of the diagram are shown the FGFR3 mutations reported in TD. Shaded are the mutations that we also identified in MM. At the bottom of the diagram are listed the mutations present uniquely in MM. Numbers indicate FGFR3 codons, and asterisks indicate stop codons. Arrowheads and smaller numbers indicate the oligonucleotides used in RT-PCR reactions to screen for mutations. The table summarizes all the FGFR3 mutations we found in MM.
FGFR3 activating mutations in TD and MM.
Schematic representation of FGFR3 receptor, with the 3 Ig-like domains (I, II, and III), the transmembrane (TM) domain, and the 2 tyrosine kinase (TK) domains. At the top of the diagram are shown the FGFR3 mutations reported in TD. Shaded are the mutations that we also identified in MM. At the bottom of the diagram are listed the mutations present uniquely in MM. Numbers indicate FGFR3 codons, and asterisks indicate stop codons. Arrowheads and smaller numbers indicate the oligonucleotides used in RT-PCR reactions to screen for mutations. The table summarizes all the FGFR3 mutations we found in MM.
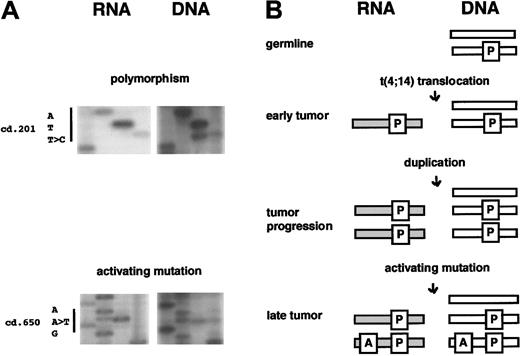
From the 4 additional primary MM tumors with t(4;14), we did not identify any with activating mutations of FGFR3, so that the overall incidence of activating mutations of FGFR3 is 1 (MM.T1) of 7 tumors that has a t(4;14) translocation. In contrast to the 3 cell lines that have activating mutations of FGFR3 and express only the activated form of FGFR3 mRNA, for the MMT.1 primary tumor cells we detected equal expression of both the activated (K650M) and normal forms (K650K) of FGFR3 mRNA (Figure3A). However, MMT.1 has 2 silent mutations in FGFR3 (T > C at nt 642, cd 201 and G > A at nt 702, cd 221), each of which allows us to distinguish the wild-type from the polymorphic FGFR3 allele (Figure 3A). Only the polymorphic allele is expressed, consistent with dysregulation of the polymorphic allele by the t(4;14) translocation. Therefore, approximately half the polymorphic alleles dysregulated by the t(4;14) translocation have an activating K650M mutation of FGFR3,whereas half do not. We conclude that the t(4;14) translocation occurs at an early stage of tumorigenesis and that activatingFGFR3 mutations occur later, during tumor progression (Figure 3B).
FGFR3 activating mutations occur during tumor progression.
(A) MMT.1 DNA and cDNA sequence analysis showed a polymorphism (ATT > ATC) at cd 201 of FGFR3. Although wild-type and polymorphic alleles are present in the tumor cells, only the polymorphic one (ATC) is expressed. Additional sequence in another region of FGFR3 identified the presence of an activating mutation at cd 650 (AAG > ATG). Both wild-type and mutant alleles are expressed. (B) At the time of the t(4;14) translocation, the 2FGFR3 alleles are distinguishable for the presence of the polymorphism (P). None of them is expressed. The translocation involved the polymorphic allele, causing its dysregulated expression (indicated by the gray bar). During tumor progression duplication of the entire or a portion of the genome occurred, followed by the acquisition of the activating mutation (A) by one of the polymorphic, duplicated alleles, so that only half of the expressed allele has the activating mutation.
FGFR3 activating mutations occur during tumor progression.
(A) MMT.1 DNA and cDNA sequence analysis showed a polymorphism (ATT > ATC) at cd 201 of FGFR3. Although wild-type and polymorphic alleles are present in the tumor cells, only the polymorphic one (ATC) is expressed. Additional sequence in another region of FGFR3 identified the presence of an activating mutation at cd 650 (AAG > ATG). Both wild-type and mutant alleles are expressed. (B) At the time of the t(4;14) translocation, the 2FGFR3 alleles are distinguishable for the presence of the polymorphism (P). None of them is expressed. The translocation involved the polymorphic allele, causing its dysregulated expression (indicated by the gray bar). During tumor progression duplication of the entire or a portion of the genome occurred, followed by the acquisition of the activating mutation (A) by one of the polymorphic, duplicated alleles, so that only half of the expressed allele has the activating mutation.
FGFR3 and ras mutations are mutually exclusive in MM
Activating mutations of K-ras or N-ras,which are reported in approximately 40% of MM tumors, contributes to IL-6–independent growth of the tumor cell.28-30Similarly, the presence of activated FGFR3 confers IL-6 independence to a mouse IL-6–dependent plasmacytoma line.16 It has also been shown that the stimulation ofFGFR3 by its ligand leads to activation of the mitogen-activated protein kinase pathway through recruitment of Ras.9 Accordingly, FGFR3 and rasactivating mutations may play an analogous role in the pathogenesis of MM.
We analyzed our panel of 30 MM lines for the presence of N-ras or K-ras activating mutations in codons 12, 13, and 61 (Table 1). Among the 9 lines that have a t(4;14) translocation and express FGFR3, 3 (33%) have anFGFR3 activating mutation (the F384L mutation in LP1 is not activating, see below), 4 (44%) have activating rasmutations, 2 (22%) have neither, none have both. Among the 21 lines that do not have a t(4:14) translocation, 9 (43%) have rasactivating mutations (Table 1). Similarly, the MMT.1 patient sample that has a K650M FGFR3 activating mutation does not have either an N-ras or a K-ras mutation. These results indicate that myeloma cells have either FGFR3 orras activating mutations, but not both, suggesting that these mutations affect the same pathway so that mutational activation of both genes in the same tumor cell would be redundant. In addition,FGFR3, like ras, may play an oncogenic role in MM tumor progression by becoming oncogenically activated by the same mutations that in another cell context cause dwarfism.
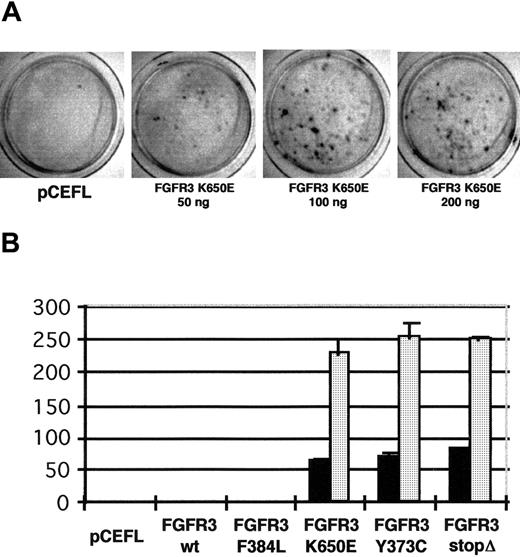
Ectopic expression of FGFR3 leads to malignant transformation
Amplification or ectopic expression of FGFR1 andFGFR2 has been detected in cancer cells,31-34and each of these FGFRs has been shown to be oncogenic in model systems.35,36 However, even though activatingFGFR3 mutations also have been reported recently in bladder and cervical cancer,37 a direct involvement of FGFR3in tumorigenesis has not yet been demonstrated. To show thatFGFR3 can function as an oncogene, we tested the ability of wild-type and mutated FGFR3 to induce cellular transformation in fibroblasts. We constructed FGFR3 expression vectors in which the wild-type and the FGFR3 mutations identified in MM (Y373C, F384L, K650E, and Δ795-808) were cloned into the pCEFL vector under the EF-1α promoter that confers a high level of expression after integration in the eukaryotic genome.38Because it has been shown that the FGFR3 receptor carrying the K650E mutation is capable of undergoing autophosphorylation in the absence of ligand—ie, it is constitutively activated39—we first tested its ability to induce focus formation in NIH 3T3 cells that do not express endogenous FGFR3. We transfected NIH 3T3 cells with pCEFL empty vector and with increasing amounts of K650E FGFR3 plasmid. Twelve days after the transfection, there were no foci in the control plate, whereas numerous foci were apparent in the K650E-transfected plates (Figure 4A). We then repeated the same assay with the other FGFR3 mutants for which the constitutive activity had not been tested. When transfected in equal amounts, Y373C, K650E, and Δ795-808 FGFR3 induced the same number of foci in NIH 3T3 cells. In contrast, we could not detect any transformation in NIH 3T3 cells transfected with the F384L polymorphic variant of FGFR3 or with wild-type FGFR3, even in the presence of its ligand aFGF (Figure 4B). These data indicate that the activating mutations of FGFR3 occurring in MM are oncogenic.
Activated forms of FGFR3 identified in MM induce transformation in NIH 3T3 in a dose-dependent fashion.
(A) NIH 3T3 cells were transfected in triplicate with 200 ng empty vector (pCEFL) and with 50, 100, and 200 ng FGFR3 carrying the activating mutation K650E. Cellular foci were stained 12 days after transfection. (B) NIH 3T3 cells were transfected in triplicate with 0.1 μg (▪) and 1 μg ( ) the indicated plasmids. Plates were scored for the presence of foci 12 to 14 days after transfection, after fixing and staining. We monitored the efficiency of transfection for each construct by counting the number of neomycin-resistant colonies on control plates.
) the indicated plasmids. Plates were scored for the presence of foci 12 to 14 days after transfection, after fixing and staining. We monitored the efficiency of transfection for each construct by counting the number of neomycin-resistant colonies on control plates.
Activated forms of FGFR3 identified in MM induce transformation in NIH 3T3 in a dose-dependent fashion.
(A) NIH 3T3 cells were transfected in triplicate with 200 ng empty vector (pCEFL) and with 50, 100, and 200 ng FGFR3 carrying the activating mutation K650E. Cellular foci were stained 12 days after transfection. (B) NIH 3T3 cells were transfected in triplicate with 0.1 μg (▪) and 1 μg ( ) the indicated plasmids. Plates were scored for the presence of foci 12 to 14 days after transfection, after fixing and staining. We monitored the efficiency of transfection for each construct by counting the number of neomycin-resistant colonies on control plates.
) the indicated plasmids. Plates were scored for the presence of foci 12 to 14 days after transfection, after fixing and staining. We monitored the efficiency of transfection for each construct by counting the number of neomycin-resistant colonies on control plates.
Consistent with the data from the focus formation assay, the K650E-transfected cells, but not the pCEFL- or the wild-type FGFR3-transfected cells, were found to be tumorigenic when injected into nude mice. Each of 9 mice received 3 subcutaneous injections with different amounts of pCEFL-, K650E-, and wild-type FGFR3-transfected cells. Fourteen days after the injection, progressively growing tumors started to appear at the site of K650E injection only in the set of mice that received the highest dose of cells (Figure5A). Two days and 4 days later the other sets of mice, injected with medium- and low-dose cells, developed tumors at the site of K650E cell inoculation. In contrast, no tumors appeared in the other sites up to 33 days after injection. From external examination the tumors appear to have a highly vascular capsule. Histologic analysis of tumor tissue revealed a vascular fibrosarcoma (Figure 5B).
Tumorigenicity of K650E expressing NIH 3T3 cells in nude mice
. (A) 105, 5 × 105, and 9 × 105 NIH 3T3 cells transfected with pCEFL (upper left flank), K650E (upper right flank), and wild-type FGFR3 (lower right flank) were subcutaneously injected into 6-week-old nude mice. A representative mouse that received 9 × 105 cells is shown 19 days after the injection. (B) Microscopic appearance of a section of K650E expressing tumor tissue stained with hematoxylin and eosin. An abundance of blood vessels is shown.
Tumorigenicity of K650E expressing NIH 3T3 cells in nude mice
. (A) 105, 5 × 105, and 9 × 105 NIH 3T3 cells transfected with pCEFL (upper left flank), K650E (upper right flank), and wild-type FGFR3 (lower right flank) were subcutaneously injected into 6-week-old nude mice. A representative mouse that received 9 × 105 cells is shown 19 days after the injection. (B) Microscopic appearance of a section of K650E expressing tumor tissue stained with hematoxylin and eosin. An abundance of blood vessels is shown.
FGFR3 transforms cells through the MAPK pathway
Our data indicate that the activating mutations of FGFR3 are oncogenic and tumorigenic. The fact that in MM these mutations are mutually exclusive with those of Ras and that, as Ras, FGFR3 activation leads to MAPK activation9 suggests that they may induce overlapping oncogenic signaling. Therefore, we investigated whetherFGFR3 transforms cells through the Ras signaling pathway leading to MAPK activation. We tested the ability of a dominant-negative form of Ras or Raf to inhibit the K650E-induced transformation of NIH 3T3 cells. We transfected NIH 3T3 cells with FGFR3 K650E or a constitutive active Ras-V12, in the presence or absence of pCEFL, or plasmids expressing the dominant negative Ras N-17 or Raf-301. After 12 to 14 days, the FGFR3 K650E focus number was significantly reduced by cotransfection with dominant-negative Ras-N17 (Figure 6). Similarly, both FGFR3 K650E and Ras transformation were inhibited by Raf301 cotransfection, confirming that FGFR3, like Ras, is able to transform cells through activation of the MAPK cascade and indicating that in MM it can play a Raslike role in tumor progression.
FGFR3 transformation can be inhibited by Raf-301 and Ras-N17.
NIH 3T3 cells were transfected in triplicate with 200 ng FGFR3 or with 50 ng Ras V12, in the presence of 4× molar excess of pCEFL, Raf 301, or Ras N17. Twelve to 14 days after transfection, the number of foci was counted and the percentage of inhibition by Ras N-17 or Raf-301 on the focus formation was calculated.
FGFR3 transformation can be inhibited by Raf-301 and Ras-N17.
NIH 3T3 cells were transfected in triplicate with 200 ng FGFR3 or with 50 ng Ras V12, in the presence of 4× molar excess of pCEFL, Raf 301, or Ras N17. Twelve to 14 days after transfection, the number of foci was counted and the percentage of inhibition by Ras N-17 or Raf-301 on the focus formation was calculated.
Discussion
The t(4;14) translocation, present in 20% to 30% of MM tumors, is unusual because it causes the concomitant dysregulation ofFGFR3 on der(14) and MMSET/WHSC1 on der(4).7 We now show cumulative evidence pointing to an oncogenic role of the t(4;14) translocation in MM. First, we find that t(4;14) cells express a functional FGFR3 on the surface of the MM cell, able to activate MAPK. Second, FGFR3 activating mutations are acquired by the myeloma cells during tumor progression and are mutually exclusive with those of Ras. Third, using an NIH 3T3 model, we demonstrate that activatedFGFR3 functions as an oncogene through the Ras pathway, indicating that it can play a Raslike role in tumor progression.
Other lines of evidence have suggested a role of FGFs and FGFRs in human cancer.40 Amplification or ectopic expression of FGFs induces cellular transformation,41 and overexpression of FGFR1 and FGFR2 has been found in many human cancers.31-34 In particular, FGFR1 is the gene dysregulated by the 8p12 translocations in stem cell myeloproliferative disorder.42,43 Consistent with these observations, activated FGFR1 and FGFR2 are able to induce transformation in NIH 3T3 cells.35,36 However, despite the occurrence of activating mutations in FGFR3 in MM and in bladder and cervical cancer,37 others were unable to show that activated FGFR3 functions as an oncogene in NIH 3T3 cells. To demonstrate an oncogenic effect in this assay, they generated chimeric forms of activated FGFR3 in which the transmembrane domain of neu receptor replaced the FGFR3transmembrane domain, or they added a myristylation signal that targeted FGFR3 to the cytoplasmic membrane.44,45 These results contrast with our finding that transformation occurs with full-length activated FGFR3.This contradictory result is best explained by the different levels of expression achieved in the transfection experiments. Previous investigators used a cytomegalovirus (CMV) promoter to drive the expression of FGFR3, whereas we used the human elongation factor 1 α (EF-1α) promoter. We found, by Western blot analysis, that in transient transfections the CMV promoter gives a higher level of expression. However, in stable transfectants, the highest expression was achieved with the EF-1α promoter, which leads to FGFR3expression at levels comparable to those seen in the MM cell lines (data not shown). Consistently, we also did not obtain cellular foci when we transfected NIH 3T3 cells with activated FGFR3 under the CMV promoter (data not shown). In this regard, by interchanging the kinase domain of FGFR3 with that of FGFR1, Ornitz11demonstrated that the kinase activity of FGFR3 is weaker than that of FGFR1. Therefore, it is not surprising that a higher level of expression is required for transformation with FGFR3 than with FGFR1. As for FGFR2, we did not obtain cellular transformation with wild-type FGFR3 in the presence of ligand.36 Chronic stimulation by ligand is not equivalent to constitutive activity of the receptor, because constitutively activated receptors are not always under the control of physiologic cellular responses that lead to the down-regulation of receptor signaling. In fact the G380R mutation of FGFR3 has recently been reported to have defective receptor down-regulation.46 FGFR3 signaling has been reported to cause growth arrest in vivo in chondrocytes and in transfected 293T cells. It seems from our results that the outcome of FGFR3depends not only on the cell type but also on the level of expression. Therefore, our results now show that activated FGFR3is an oncogene able to induce cellular transformation in fibroblasts and tumors in nude mice. Moreover, using murine bone marrow cells transduced with retroviral vectors containing an activatedFGFR3, we have shown that FGFR3 can produce lymphoid malignancies in mice, strongly supporting a role forFGFR3 in myeloma (manuscript submitted). To study more definitively the oncogenic role of FGFR3 dysregulation in MM cells (as opposed to fibroblasts), we are constructing transgenic mice that will express FGFR3 only in late B and plasma cells.
Three of 9 MM lines and 1 of 7 primary MM tumors with the t(4;14) translocation have the same FGFR3 activating mutations that in the germline cause TD, the most severe form of dwarfism that leads to neonatal lethality. In one case, we were able to prove that the activating mutation is present in a fraction of the FGFR3alleles with the t(4;14) translocation. This indicates that the t(4;14) translocation occurs at an early stage of tumorigenesis and that the subsequent activating mutation in the dysregulated FGFR3occurs during tumor progression. The frequency of FGFR3mutations in patients with t(4;14) MM appears to be low (1 of 7). To accurately determine the frequency at diagnosis and relapse of these mutations, paired samples taken at diagnosis and at advanced, florid relapse from MM patients with FGFR3 expression, identified by immunohistochemistry or by flow cytometry, should be evaluated by SSCP and sequencing analysis of cDNA. Similarly, N-ras and K-ras activating mutations, which occur in approximately 40% of MM tumors, are associated with tumor progression.28 Stimulation of FGFR3 by its ligand FGF, which is expressed by bone marrow stromal cells, leads to activation of the MAPK pathway through the recruitment of Ras. Accordingly,FGFR3 and ras activating mutations seem to fulfill an analogous role in the pathogenesis of MM. This is consistent with our observation that mutations of Ras and of FGFR3 are mutually exclusive in the MM samples we analyzed. Furthermore, FGFR3-induced transformation can be inhibited by cotransfection with dominant-negative forms of either Ras (Ras N17) or Raf (Raf 301), confirming that FGFR3, like Ras, acts through MAPK activation.
IL-6 is secreted by the stromal cells in the bone marrow47and is an important survival and growth factor for normal plasma cells and for MM cells during the early stages of the disease.48Stimulation with IL-6 activates several signaling pathways, including the Ras pathway. When transfected into the IL-6–dependent MM cell line ANBL6, activated N-Ras causes augmented growth in suboptimal IL-6 concentrations and in IL-6–independent growth of the cells.29 Similarly, we recently found that ectopic expression of an activated FGFR3 is able to confer IL-6 independence, enhanced IL-6 proliferative response, and reduced apoptosis to a murine IL-6–dependent plasmacytoma cell line.16 Neither activated Ras nor activated FGFR3 is sufficient to replace stromal cells or IL-6 in all MM tumors. First, 2 of 5 IL-6–dependent MM cell lines have activating mutations of N- or K-ras but remain IL-6 dependent.49 Second, both the MM5.1 and the MM5.2 MM cell lines have an activating mutation of FGFR3, but for survival and proliferation MM5.1 cells require stromal cells plus IL-6, whereas MM5.2 cells do not require stromal cells but still require IL-6.22
Oncogenesis is a multistep process. The best-characterized example is colon cancer, in which progressive tumor-suppressor gene inactivation and oncogene activation correlate with defined stages of tumor progression. We hypothesize that chromosomal translocations into an IgH switch region, causing ectopic expression of oncogenes, represent the first step in the establishment of the “malignant” myeloma clone by causing immortalization of a plasma cell that otherwise would die within approximately 30 days after isotype switching (Figure7). In the case of t(4;14) myeloma, the same translocation event may provide several oncogenic signals to the cell by simultaneously dysregulating 2 putative oncogenes. The dysregulation of MMSET/WHSC1 in MM, together with its homology to the HRX/ALL-1 gene involved in 11q23 translocation in acute leukemia, suggests an oncogenic role forMMSET in MM tumors with t(4;14) translocation. We have not found that the full-length MMSET protein is transforming in NIH 3T3 cells, but we have found that a truncated version, expressed together with the full-length protein in t(4;14) MM tumor cells, acts as a tumor-suppressor gene by inhibiting the transforming activity of every tested oncogene (M.C., unpublished data, 1999). The simultaneous dysregulation of FGFR3 by the same t(4;14) translocation may provide a survival or proliferative signal through its stimulation by FGF ligands expressed in the bone marrow microenvironment. Alternatively, it is possible that the overexpression of FGFR3 has no immediate effects on tumor formation but that the occurrence of point mutations causing constitutive activation of FGFR3 in the absence of ligand contributes to tumor progression. Our results demonstrate that indeed these FGFR3 activating mutations occurring in MM are oncogenic and that the ectopically expressed activated FGFR3 is a novel oncogene that can play a Raslike role in MM tumor progression.
A model of progressive genetic events in t(4;14) MM.
A plasma cell (PC) is immortalized by a t(4;14) translocation, resulting in dysregulated expression of FGFR3 and MMSET in MGUS. Activating mutations occur in either FGFR3 or Ras and are associated with malignant progression of the myeloma clone. Subsequent genetic events, such as c-myc dysregulation by 8q24 translocation,17 lead to extramedullary growth of the tumor cells, resulting in secondary plasma cell leukemia (PCL).
A model of progressive genetic events in t(4;14) MM.
A plasma cell (PC) is immortalized by a t(4;14) translocation, resulting in dysregulated expression of FGFR3 and MMSET in MGUS. Activating mutations occur in either FGFR3 or Ras and are associated with malignant progression of the myeloma clone. Subsequent genetic events, such as c-myc dysregulation by 8q24 translocation,17 lead to extramedullary growth of the tumor cells, resulting in secondary plasma cell leukemia (PCL).
Acknowledgment
We thank Dr Melissa Pope (The Rockefeller University, New York) for assistance with flow cytometry.
Supported by the Howard Temin Award from the National Cancer Institute (CA74265) and by a Translational Research Award of the Leukemia and Lymphoma Society of America.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
P. Leif Bergsagel, Department of Medicine, Division of Hematology-Oncology, New York Presbyterian Hospital–Weill Medical College of Cornell University, Rm C-609, 525 East 68th St, New York, NY 10021; e-mail: plbergsa@med.cornell.edu.





This feature is available to Subscribers Only
Sign In or Create an Account Close Modal