Abstract
The use of immunodeficient mice, particularly of the nonobese diabetic/severe combined immunodeficient (NOD/SCID) strain, has allowed detection of very primitive malignant progenitors from patients with acute myelogenous leukemia (AML). To define the sensitivity and reproducibility with which the engraftment of different AML cells can be detected, 61 different samples from patients with newly diagnosed AML representing a variety of cytogenetic and French-American-British (FAB) subtypes were injected into NOD/SCID mice. Eight weeks after intravenous injection of 107 AML cells, the average percent of human cells in mouse bone marrow was 13.3%, with 70% of samples showing easily detectable engraftment of CD45+ cells. AML samples with cytogenetic changes associated with a poor clinical prognosis tended to engraft to higher levels than those with changes associated with a good prognosis. Cells with FAB subtypes M3 and, to a lesser extent, M2, engrafted more poorly (P = .002 and .06, respectively) than those from other subtypes. Intraperitoneal injection of human interleukin-3 and Steel factor thrice weekly for 4 weeks did not enhance the levels of AML cell engraftment. However, AML samples that showed cytokine-independent colony growth in methylcellulose assay or expressed growth-factor mRNA in malignant blasts achieved significantly higher levels of engraftment than those which were cytokine dependent in culture or failed to express cytokine message (P < .03 and P < .02, respectively). In 6 patient samples, the frequency of NOD/SCID leukemia-initiating cells (NOD/SL-IC) varied from 0.7 to 45 per 107 cells, which was 200- to 800-fold lower than the frequency of AML long-term culture-initiating cells (AML LTC-IC) in the same samples. Each NOD/SL-IC will produce more than 106leukemic blasts as well as many AML-CFC and AML LTC-IC as detected 8 weeks postinjection into mice. Serial transplant experiments showed the ability of NOD/SL-IC to maintain their own numbers over at least 3 to 4 weeks in vivo. The ability of these progenitors to self-renew combined with their potential to differentiate to produce large numbers of more mature progenitors and leukemic blasts suggests that the NOD/SL-IC assay identifies leukemic ‘stem cells’ that may maintain the malignant clone in human patients. The further use of this assay should facilitate studies of AML stem cell biology and the evolution of novel therapeutic strategies.
THE MALIGNANCIES encompassed by the term acute myelogenous leukemia (AML) are clonal disorders of hematopoiesis associated with varying degrees of deregulation of normal hematopoietic differentiation and proliferation. However, despite these defects it has been possible to show that the hierarchical organization of progenitor cells that characterizes normal blood cell formation is preserved to a large extent in these diseases. Thus, a proportion of leukemic cells will form colonies of blasts in semisolid medium when supplied with a source of hematopoietic growth factors (AML colony-forming cells or AML-CFC).1 More recently it has been shown that leukemic progenitors which are more rare than AML-CFC can give rise to long-term malignant hematopoiesis when placed in coculture with supportive feeder layers or in suspension cultures supplemented with cytokines.2,3 The cell-surface phenotype of these leukemic long-term culture-initiating cells (AML LTC-IC) or suspension culture-initiating cells appears to be very similar to normal LTC-IC.3-5
Transplantation models in mice have been critical to the development of our understanding of the most primitive hematopoietic progenitors that are capable of reconstituting multilineage hematopoiesis in lethally irradiated recipients. It has been possible to use some of the principles that were used to develop these assays for murine ‘stem cells’ to study normal human cells that exhibit similar potential when injected into sublethally irradiated immunodeficient mice. Recent studies have shown that multilineage human hematopoiesis can be successfully established in nonobese diabetic/LtSz-scid/scid (NOD/SCID) mice6 after intravenous (IV) injection of normal human marrow or cord blood cells.7-11
Immunodeficient mice will also support the growth of malignant progenitors from patients with chronic myelogenous leukemia and AML.12-15 IV injection of cells directly isolated from patients with AML into NOD/SCID mice can result in the engraftment and proliferation of these cells in mouse hematopoietic tissues in a fashion similar to that seen in the human disease.15 AML cells with the potential to initiate leukemia in mice (NOD/SCID leukemia-initiating cells or NOD/SL-IC) are rare progenitors that are largely CD34++ CD38−,14,15CD71− and HLA-DR−,16and Thy-1−.17 These results suggested that NOD/SCID animals could be used for the detection and further characterization of very primitive leukemic progenitors that may be analogous to those which maintain the leukemic clone in patients. The fact that such cells are the obvious targets for novel therapeutic approaches in AML further supported our efforts to enhance our understanding of this model system.
Although it was clear from the preceding studies that AML cells would grow successfully in the appropriate mouse strains, the variability of the growth potential of various AML samples was not so apparent. In addition, little was known about factors that may influence growth of human AML cells in these animals and how various classes of malignant progenitors were maintained over time in the mice. The current studies were undertaken to answer several of these questions. Firstly, we surveyed a large series of AML samples representative of the clinical, phenotypic, and genetic heterogeneity seen in these diseases for their ability to grow in NOD/SCID mice. Secondly, the human cytokine requirements of NOD/SL-IC were studied and compared with both the growth-factor responsiveness of AML-CFC and autocrine growth-factor gene expression by the malignant blasts from the same patient specimen. Thirdly, the frequency and proliferative capacity of NOD/SL-IC was described and compared with the same parameters obtained for AML LTC-IC. These data show the ability of NOD/SCID mice to allow the detection and quantitation of these very primitive leukemic progenitors in most AML samples. Furthermore, clinical features of the disease with prognostic significance in patients, cytokine gene expression in the malignant clone, and the growth characteristics of leukemic progenitors in culture appear to predict the growth potential of NOD/SL-IC from different cell sources in mice.
MATERIALS AND METHODS
Patients’ cells.
Peripheral blood or bone marrow cells were obtained from 61 patients (pts) with newly diagnosed AML undergoing marrow and blood examination for diagnostic purposes after informed consent and with the approval of the Clinical Research Ethics Board of the University of British Columbia. Mononuclear cells were separated by Ficoll-Hypaque (Pharmacia, Uppsala, Sweden) density gradient centrifugation and either used immediately for the experiments described below or cryopreserved in Iscove’s modified Dulbecco’s medium (IMDM; Stem Cell Technologies, Vancouver, Canada) with 50% fetal calf serum (FCS) and 10% dimethylsulfoxide. Frozen cells were thawed at 37°C, washed in α-MEM (Stem Cell Technologies) with 5% FCS, and cell viability was determined by trypan blue exclusion. As part of their clinical evaluation, all patient samples had morphological, histochemical, and flow cytometric studies performed on their leukemic blasts with subsequent classification according to French-American-British (FAB) subtypes.18 Cytogenetic analysis was performed on the initial diagnostic bone marrow samples.
Eleven patient samples were analyzed in more detail than the group as a whole for their cytokine responsiveness and/or the frequency and proliferative capacity of malignant progenitors. Clinical characteristics of these patients at presentation are shown in Table 1.
Patient Samples
| Patient . | Age . | Sex . | FAB . | WBC (% blasts) (×109/L) . | Bone Marrow Cytogenetics [% abnormal] . |
|---|---|---|---|---|---|
| 1 | 59 | M | M2 | 75 (53) | 46,XY,t(9;22); 46,XY,t(9;22),del(20q) [100] |
| 2 | 63 | F | M1 | 295 (>90) | ND |
| 3 | 29 | F | M4 | 87 (6) | 46,XX; 46,XX,del(16)(q22) [32] |
| 4 | 44 | M | M1 | 148 (95) | 46,XY |
| 5 | 58 | F | M4 | 370 (46) | 46,XX; 47,XX,+13 [37] |
| 6 | 69 | F | M4 | 65 (83) | 47,XX,+8 [100] |
| 7 | 64 | F | M5a | 129 (95) | 47,XX,+8,rea(11)(q23) [100] |
| 8 | 77 | M | M2 | 57 (51) | 47,XY,+8,t(12;22)(p13q12),del(20)(q1.2q1.3) [100] |
| 9 | 60 | F | M4 | 56 (76) | 46,XX,del(7q),del(16q); 46,XX,del(16q),+22 [100] |
| 10 | 63 | F | M1 | 27 (80) | 46,XX,t(8;20)(p12q32) [100] |
| 11 | 48 | M | M5a | 72 (53) | 46,XY |
| Patient . | Age . | Sex . | FAB . | WBC (% blasts) (×109/L) . | Bone Marrow Cytogenetics [% abnormal] . |
|---|---|---|---|---|---|
| 1 | 59 | M | M2 | 75 (53) | 46,XY,t(9;22); 46,XY,t(9;22),del(20q) [100] |
| 2 | 63 | F | M1 | 295 (>90) | ND |
| 3 | 29 | F | M4 | 87 (6) | 46,XX; 46,XX,del(16)(q22) [32] |
| 4 | 44 | M | M1 | 148 (95) | 46,XY |
| 5 | 58 | F | M4 | 370 (46) | 46,XX; 47,XX,+13 [37] |
| 6 | 69 | F | M4 | 65 (83) | 47,XX,+8 [100] |
| 7 | 64 | F | M5a | 129 (95) | 47,XX,+8,rea(11)(q23) [100] |
| 8 | 77 | M | M2 | 57 (51) | 47,XY,+8,t(12;22)(p13q12),del(20)(q1.2q1.3) [100] |
| 9 | 60 | F | M4 | 56 (76) | 46,XX,del(7q),del(16q); 46,XX,del(16q),+22 [100] |
| 10 | 63 | F | M1 | 27 (80) | 46,XX,t(8;20)(p12q32) [100] |
| 11 | 48 | M | M5a | 72 (53) | 46,XY |
Abbreviations: WBC, white blood cell count; ND, not done.
Transplantation of AML cells into NOD/SCID mice.
NOD/SCID mice were bred and maintained under sterile conditions in the British Columbia Cancer Research Center Joint Animal Facility according to protocols approved by the Animal Care Committee of the University of British Columbia. Six- to 8-week-old mice were irradiated with 350 cGy from a 137Cs source 24 hours before injection of patient AML cells via the tail vein. After various periods of time, mice were killed by CO2 inhalation. Blood cells were obtained by cardiac puncture. Bone marrow was removed from the 4 long bones of the limbs by flushing with α-MEM with 5% FCS. Spleen cells were obtained by mincing and flushing separated cells free with media. Cells from mouse tissues were then used in the assays described below. When human cytokines were administered to mice they were diluted in sterile phosphate-buffered saline (PBS) with 0.1% bovine serum albumin (BSA) and injected intraperitoneally on Monday, Wednesday, and Friday of each week beginning 4 weeks after injection of AML cells.
Cytokines.
Human interleukin-3 (IL-3) was obtained from Sandoz International (Basel, Switzerland) and human Steel factor (SF) was purified in our center from supernatants of COS cells transfected with the cytokine cDNA. Cytokine levels in mouse serum were determined by enzyme-linked immunosorbent assay (ELISA) according to the manufacturer’s instructions (R&D Systems, Minneapolis, MN).
Flow cytometry.
Cells from mouse tissues were treated with 7% ammonium chloride (Stem Cell Technologies) to lyse red blood cells, then spun down and resuspended in Hanks’ balanced salt solution with 2% FCS (HFN) and 5% human serum for blocking of human Fc receptors. Cells were incubated on ice with an anti-mouse IgG Fc receptor monoclonal antibody (2.4G2; SyStemix, Palo Alto, CA) for blocking of nonspecific binding to mouse Fc receptors. Half of each sample was then incubated on ice with fluoresceinated anti-CD45, a human-specific pan-leukocyte marker (prepared in our center from American Type Culture Collection [ATCC] clone no. HB10508, Rockville, MD) to detect human cells, and the other half with fluoresceinated mouse IgG1(Becton Dickinson Immunocytometry Systems, San Jose, CA) as an isotype control for nonspecific immunofluorescence. Finally, cells were stained with 2 μg/mL propidium iodide in HFN. Flow cytometric analysis was performed on a Becton Dickinson FACScan or FACSort flow cytometer. A gate was set to exclude at least 99.9% of cells labeled with the isotype control, and the percent of CD45+ cells was then determined using the same gate after excluding nonviable cells. In experiments where bone marrow cells from control mice that had not been previously injected with human bone marrow cells were analyzed, the mean ± SEM percent CD45+ cells was 0.09% ± 0.01% (n = 30) and the highest level of apparently CD45+ cells detected in 1 of these 30 control mice was 0.33%. In some experiments, CD45+ cells were sorted into media and used for functional assays, fluorescence in situ hybridization (FISH), or morphological analysis.
Histology and FISH.
Bone marrow smears were obtained from mice at the time of killing by snipping the end off the femur and smearing the cut end on a glass slide. Alternatively, cytospin preparations were made from bone marrow cell suspensions or flow-sorted CD45+ cells. Slides were then fixed in either methanol:acetone (1:3) for 20 minutes for May-Grünwald-Giemsa staining, or in methanol:acetic acid (3:1) for FISH as previously described2 to detect the presence of cytogenetic abnormalities characteristic of the leukemic cells. Briefly, the probe used to detect the +8 abnormality was the D8Z2 plasmid (ATCC), which is specific for centromeric repeat sequences on human chromosome 8, and which was labeled with digoxigenin (DIG; Boehringer Mannheim, Mannheim, Germany) by nick translation. To detect the +13 abnormality, the Quint-Essential 13-specific DNA probe labeled with DIG was purchased from Oncor (Gaithersburg, MD). For both probes, all slides were pretreated as previously described.2 For the chromosome 8 probe, hybridization and washing conditions were as previously described; for the chromosome 13 probe, hybridization and washing conditions were as instructed by the manufacturer. In both cases, detection of DIG-labeled probes was performed using sheep anti-DIG–fluorescein isothiocyanate (FITC) antibody (Boehringer Mannheim) and rabbit anti-sheep–FITC antibody (Vector Labs, Burlingame, CA), as previously described.2 Finally, slides were counterstained with 0.5 μg/mL propidium iodide in antifade (200 mmol/L 1,4 diazabicyclo-[2,2,2]-octane, 2 mmol/L Tris, pH 8, in 90% glycerol) and viewed on a Zeiss Axioplan fluorescence microscope (Zeiss, Oberkochen, Germany) equipped with a double bandpass filter to allow simultaneous visualization of the FITC signal and the propidium iodide counterstain. In the case of BM smears or cytospins prepared from unsorted mouse BM, only cells that clearly had either 2 signals or 3 signals were counted (ie, only human cells). The number of cells counted in these cases ranged from 5 to 76 per slide, with the lower end of this range being due to a low engraftment level in that mouse (≈1%). For CD45+ sorted cells, again only cells with a clear 2 or 3 signals were counted, and the number of cells counted ranged from 42 to 85 per slide. In the case of colonies, each colony was scored as either normal or abnormal only if a minimum of 5 cells per colony showed a clear signal, and if at least 80% of the cells in a given colony showed either the normal or the abnormal signal. The human origin of colonies was confirmed by hybridization with the human specific FISH probes.
May-Grünwald-Giemsa–stained slides were examined by bright-field microscopy and a minimum of 200 cells scored for the presence of AML blasts to obtain percentages for comparison with the results of CD45 analysis.
DNA analysis.
In some cases, the proportion of human cells in mouse tissue was determined by DNA analysis. Cells from mouse tissue suspended in media were centrifuged and resuspended in 2 mL of DNA lysis buffer (10 mmol/L Tris, pH 8.0, 150 mmol/L NaCl, 10 mmol/L EDTA, 0.5% sodium dodecyl sulfate [SDS], 200 μg/mL proteinase K [Life Technologies, Gaithersburg, MD]) and incubated at 37°C overnight. Two equal-volume phenol extractions and 2 equal-volume chloroform:isoamyl alcohol (24:1) extractions were performed, and then DNA was dialyzed for 48 hours, with 3 changes of dialysis buffer (10 mmol/L Tris, 1 mmol/L EDTA, pH 7.5). For Southern blotting, 10 μg of the resulting DNA was digested with 100 U of EcoRI (Life Technologies) overnight at 37°C, run in a 1% agarose gel, and blotted by standard procedures.19 Blots were hybridized with a32P-labeled EcoRI fragment of the human endogenous retroviral sequence (HERV-H) as a human-specific probe. This DNA sequence is known to be present at approximately 1,000 copies in the human genome.20 To estimate the proportion of human cells in mouse-tissue DNA, a dilution series of human genomic DNA mixed with mouse DNA, ranging from 0.1% to 100% human DNA, was run on the same gel as the samples to be evaluated and the intensities of hybridization signals from the samples compared with that from the known mixtures. The correlation between the proportion of human cells in mouse tissues estimated by this method compared with that determined by FACS analysis was .93, P < .001. However, whereas the limit of sensitivity for FACS analysis was approximately 0.5% human cells, less than 0.1% human cells could be detected using the Southern blotting technique.
Detection of cytokine gene expression in AML blasts.
Total amplified cDNA was generated from AML blasts with an oligo(dT)-based primer and poly(A) tailing strategy, as described.5,21 Briefly, total RNA was extracted from aliquots of 104 cells and reverse transcribed using a 60-mer oligo(dT) primer. The reverse transcription product was then poly(A)-tailed, and this mixture was polymerase chain reaction (PCR)–amplified using the oligo(dT) primer, to yield total amplified cDNA. An aliquot of total amplified cDNA was subjected to Southern blotting followed by hybridization with probes for human cytokines. To ensure that cDNA amplification had been successful, each blot was also hybridized with a β-actin probe.22 Hybridization and washing conditions were as described.21
To enhance the sensitivity with which growth-factor cDNA could be detected, a second round of PCR was performed using cytokine-specific primers when Southern blotting of total cDNA did not detect expression of the growth factors. The 50-μL PCR reaction contained 1 μL of total amplified cDNA, 1X PCR buffer containing 20 mmol/L Tris-HCl pH 8.4 and 50 mmol/L KCl (Life Technologies), 1 U of Taq DNA polymerase (Life Technologies), and 10 pmol of each primer, as follows: IL-3 (5′-GCTCCCATGACCCAGACAACGTCC-3′) and (5′-CAGATAGAACGTCAGTTTCCTCCG-3′); SF (5′-GGATCTGCAGGAATCGTGTGACTA-3′) and (5′-CTTCAGGAGTAAAGAGCCTGGGTT-3′); granulocyte colony-stimulating factor (G-CSF) (5′-CTCTGGACAGTGCAGGAAGCCACC-3′) and (5′-GCTGGGCAAGGTGGCGTAGAACGC-3′); granulocyte-macrophage colony-stimulating factor (GM-CSF) (5′-CGGCGTCTCCTGAACCTGAG-3′) and (5′-CCAGCAGTCAAAGGGGATGA-3′), to give DNA fragments of 345 bp, 335 bp, 547 bp, and 300 bp, respectively. Thirty cycles of 94°C for 30 seconds, 60°C for 1 minute, and 72°C for 1 minute were then performed. As a positive control, mouse cell lines that had been transfected with the appropriate human growth-factor cDNA were analyzed in parallel. PCR products were gel electrophoresed and transferred onto a nylon membrane before hybridization with cytokine cDNA probes (Zeta-probe; BioRad, Hercules, CA).
The following gel-purified fragments were used to synthesize the probes: the entire 950-bp coding sequence of the human SF cDNA,23 the entire 600-bp coding sequence of the human IL-3 cDNA,24 the 466-bp PstI fragment of the human GM-CSF cDNA,25 the entire 700-bp coding sequence of the human G-CSF cDNA,26 and the 1,200-bp PstI fragment of a chicken β-actin cDNA.22 Probes were labeled with32P-dCTP (Amersham, Arlington Heights, IL) using a random-primer DNA labeling system (Life Technologies) according to the manufacturer’s instructions and purified on a Sephadex-G50 column (Pharmacia Biotech, Uppsala, Sweden). Blots were hybridized overnight at 65°C in 6X SSC,19 1% SDS, 1X Denhardt’s solution (0.02% wt/vol Ficoll, 0.02% polyvinylpyrrolidone, 0.02% BSA), then washed twice in 0.3X SSC, 0.1% SDS for 30 minutes each at 65°C, and exposed to Kodak XAR film (Eastman Kodak, Rochester, NY).
AML-CFC assays.
To quantitate AML-CFC numbers, cells obtained either directly from mice or after FACS purification of CD45+ cells were plated at a concentration of 0.2 to 1 × 105 cells/mL in methylcellulose medium (0.92% methylcellulose, 30% FCS, 2 mmol/L L-glutamine, 10−4 mol/L β-mercaptoethanol, 1% BSA in IMDM; Stem Cell Technologies) with 3 U/mL human erythropoietin (Epo; Stem Cell Technologies), 10 ng/mL GM-CSF (Sandoz), 10 ng/mL IL-3, 50 ng/mL SF, and 50 ng/mL Flt-3 ligand (Immunex, Seattle, WA). Cultures were scored for the presence of colonies containing more than 20 cells and clusters of 4 to 20 cells 14 days later. Because it is possible for some mouse colonies to grow under the conditions of these colony assays, when cells were assayed directly without FACS purification colonies were plucked onto glass slides for FISH to determine their human origin as well as the presence or absence of cytogenetic abnormalities that were present in the initial leukemic clone.
LTC.
LTC were established as previously described27 by coculture of mouse bone marrow cells with Sl/Sl-J-IL3 feeders, which consist of Sl/Sl fibroblasts, originally obtained from Sl/Sl mouse embryos28 engineered to produce human IL-3 at a concentration of 16.5 ng/mL. These feeders were irradiated to 80 Gy and plated in collagen-coated tissue culture dishes at 3 × 104 cells/cm2 at least 24 hours before coculture. Bone marrow cells from engrafted mice were sorted by FACS for CD45 expression before coculture with these feeders in cases where engraftment levels were low (<10%), or were placed directly into coculture in cases where higher engraftment levels were achieved. Cell numbers plated ranged from 3 to 8 × 105 per 35-mm diameter dish in the case of CD45+ sorted cells, and from 3 to 5 × 106 per dish in the case of unsorted mouse marrow cells. In all cases, cells were suspended in Myelocult LTC media (Stem Cell Technologies) with 10−6 mol/L solucortef (Sigma-Aldrich Canada, Oakville, Ontario, Canada). Cultures were maintained at 37°C in 5% CO2 and received weekly ½-media changes and twice-weekly additions of SF to give 50 ng/mL. After 5 weeks the entire contents of the culture were harvested by trypsinization and cells placed in methylcellulose assays for detection of AML-CFC as described above.
Limiting dilution analysis in mice.
The frequency of progenitors that initiate AML cell growth in mice was estimated by limiting dilution analysis. Cohorts of up to 8 mice each were injected with 5 different doses of AML cells from the same patient sample, ranging from 1 × 105 to 1 × 107. Because of concerns that the seeding efficiency of the AML cells would be reduced when very small numbers of cells were injected, 2 × 106 irradiated (15 Gy) normal human bone marrow cells were coinjected with leukemic cell doses of 1 × 105 and 3 × 105. Eight weeks after injection mouse bone marrow was analyzed for percent CD45+cells, and the frequency of NOD/SCID leukemia-initiating cells (NOD/SL-IC) calculated from the frequency of negative mice in each group by using Poisson statistics. In cases where the engraftment levels were less than 1% by FACS analysis, DNA analysis was also performed to confirm that small numbers of human cells were not present.
Calculations and statistical analysis.
Comparisons of levels of engraftment and correlation coefficients were done using a 2-tailed Student t-test. Comparisons between numbers of samples showing high levels of engraftment in mice or factor-independent colony growth and those expressing growth-factor mRNA were done using χ2 analysis. A significance level of .05 was chosen.
For limiting dilution analysis, the frequency of NOD/SL-IC in the starting cell population was calculated from the frequency of mice negative for the presence of AML cells in bone marrow in each group of animals injected with different numbers of cells as previously described.29
For calculation of the total number of human AML cells present per mouse, it was assumed that the number of cells recovered from the marrow of 4 long bones represented approximately 25% of the entire mouse bone marrow30 and that more than 90% of the AML cells in the animal were present in the marrow. The total number of AML blasts in a mouse at the time of analysis would thus be the percent CD45+ cells in mouse marrow multiplied by the number of cells recovered from 4 long bones divided by 0.25.
To determine the average number of cell progeny per NOD/SL-IC, the calculated number of AML blasts, AML-CFC, or AML-LTC-IC present in the mouse at week 8 postinjection was divided by the number of NOD/SL-IC injected into the mouse on day 0 as determined by limiting dilution.
RESULTS
Variability of engraftment of AML samples in NOD-SCID mice.
Light-density peripheral blood cells were isolated from 61 different patients with newly diagnosed AML. Eight weeks after IV injections of 107 cells per mouse femoral bone marrow was removed and analyzed for the presence of human cells by flow cytometry. An average of 3 (range, 1 to 10) mice were analyzed per patient sample and mean percent CD45+ bone marrow cells in the group of mice calculated to derive the values shown in Fig 1. Human CD45+ cells were easily detectable by flow cytometry in mouse bone marrow for 43 (70%) of the 61 samples (reliable detection of CD45+ cells above background fluorescence was 0.5%). Among the 61 samples, the mean ± SEM level of engraftment was 13.3% ± 3.1% (Fig 1A).
Engraftment of AML samples in NOD/SCID mice. The percent CD45+ cells in mouse marrow was determined for each sample 8 weeks after IV injection of 107 cells. Each point represents the mean percent engraftment in the bone marrow of all mice injected with cells from an individual patient sample (mean, 3 mice per sample; range, 1 to 10 mice). The numerical values shown are the means for each group of samples. (A) Influence of cytogenetic abnormalities. Changes associated with a poor prognosis included inv(3), +8, 11q23 rearrangements, t(9;22), del(20q), del(7q), +13, t(12;22), and a variety of complex abnormalities. Changes associated with a good prognosis included inv(16) or variants, or t(15;17). There was a trend toward higher levels of engraftment with samples with poor-risk cytogenetic features (P = .06). (B) Influence of FAB subtype. Fifty-seven of the 61 samples could be classified into AML subtypes according to FAB criteria. The mean engraftment levels obtained from each subtype are shown. Levels of engraftment were lower with samples with FAB subtypes M3 (P = .002) and M2 (P = .06) than with other subtypes. (▴), AML samples with cytogenetic abnormalities with a poor prognosis; (▪), samples with cytogenetic change with favorable prognosis; (•), samples with normal cytogenetics and intermediate prognosis.
Engraftment of AML samples in NOD/SCID mice. The percent CD45+ cells in mouse marrow was determined for each sample 8 weeks after IV injection of 107 cells. Each point represents the mean percent engraftment in the bone marrow of all mice injected with cells from an individual patient sample (mean, 3 mice per sample; range, 1 to 10 mice). The numerical values shown are the means for each group of samples. (A) Influence of cytogenetic abnormalities. Changes associated with a poor prognosis included inv(3), +8, 11q23 rearrangements, t(9;22), del(20q), del(7q), +13, t(12;22), and a variety of complex abnormalities. Changes associated with a good prognosis included inv(16) or variants, or t(15;17). There was a trend toward higher levels of engraftment with samples with poor-risk cytogenetic features (P = .06). (B) Influence of FAB subtype. Fifty-seven of the 61 samples could be classified into AML subtypes according to FAB criteria. The mean engraftment levels obtained from each subtype are shown. Levels of engraftment were lower with samples with FAB subtypes M3 (P = .002) and M2 (P = .06) than with other subtypes. (▴), AML samples with cytogenetic abnormalities with a poor prognosis; (▪), samples with cytogenetic change with favorable prognosis; (•), samples with normal cytogenetics and intermediate prognosis.
Thirty-two of the 61 patient samples (52%) had cytogenetic abnormalities detected in their diagnostic bone marrow samples. Thirteen samples had cytogenetic changes associated with a good clinical prognosis, ie, inv(16) or variants (n = 11) or t(15;17) (n = 2).31 The mean level of engraftment in this group was 5.7% (range, <0.1% to 35%). The remaining 19 samples had chromosomal rearrangements associated with a poor prognosis. These abnormalities included inv(3), +8, 11q23 rearrangements, t(9;22), del(20q), del(7q), +13, t(12;22), and a variety of complex abnormalities. The mean level of engraftment in mouse bone marrow in this group was 20.5% (range, <0.1% to 100%). As shown in Fig 1A, it appears that AML samples with poor-risk cytogenetic features often engraft in mice to higher levels than those with changes associated with a good prognosis. However, there is considerable heterogeneity and overlap between the 2 groups and the difference in levels of engraftment obtained did not reach statistical significance (P = .06 by Studentt-test).
Fifty-seven of the group of 61 AML samples could be classified into different AML subtypes according to FAB criteria.18 When the levels of engraftment of these different cell types in mice were compared among the subgroups, the lowest mean percent human cells in mouse marrow was seen among the AML M0 (n = 1), M2 (n = 4), and M3 (n = 5) samples (0.24%, 4.5%, and 1.8%, respectively), whereas the highest were seen among those with M1 (n = 8), M4 (n = 24), and M5 (n = 11) subtypes, 13.7%, 14.6%, and 18.9%, respectively. The difference in levels of engraftment between M3 samples and all others was highly statistically significant (P = .002) and approached significance (P = .06) for M2 samples (Fig 1B). Figure 1B also indicates the cytogenetic prognostic subgroup for the patient samples in the different FAB subtypes where cytogenetic abnormalities had been detected. Among patients with FAB subtypes M2 and M5, all those with detectable cytogenetic abnormalities had chromosome rearrangements associated with a poor prognosis. In contrast, the 2 M3 samples that were cytogenetically abnormal both had the favorable prognostic change t(15;17). Two samples with unfavorable and 1 with favorable prognostic abnormalities were found among the 9 AML-M1 cases. The most heterogeneity was seen among the M4 AMLs. As expected, all but 1 of the 11 patient samples with good prognosis chromosome 16 abnormalities were found in this group. However, an additional 8 patients with changes associated with a poor prognosis were also classified with this FAB subtype.
To confirm that the human cells growing in the mice were leukemic, May-Grünwald-Giemsa–stained bone marrow touch preparations or cytospins of marrow cells from mice 8 weeks posttransplant were examined for 21 patient samples. The proportion of blast cells identified in the differential cell counts on these slides were in most cases comparable to the percent CD45+ cells as assessed by flow cytometry (r = .74, P < .001). In some cases, characteristic morphological features such as dysplastic eosinophils from AML M4eo samples were clearly distinguishable in mouse marrow samples (Fig 2A).
(A) Bone marrow smear from a mouse 8 weeks after injection with cells from a patient with AML M4Eo showing the characteristic morphology of this subtype, including dysplastic eosinophils (black arrowhead) and leukemic blasts (white arrowheads). (B) FISH on a colony grown from the marrow of a mouse 8 weeks after injection with cells from pt 8. The probe used was D8Z2, which is specific for centromeric repeat sequences on human chromosome 8. The +8 abnormality previously identified in the leukemic clone of this patient is illustrated.
(A) Bone marrow smear from a mouse 8 weeks after injection with cells from a patient with AML M4Eo showing the characteristic morphology of this subtype, including dysplastic eosinophils (black arrowhead) and leukemic blasts (white arrowheads). (B) FISH on a colony grown from the marrow of a mouse 8 weeks after injection with cells from pt 8. The probe used was D8Z2, which is specific for centromeric repeat sequences on human chromosome 8. The +8 abnormality previously identified in the leukemic clone of this patient is illustrated.
Four AML samples that engrafted well in mice had cytogenetic markers that could be detected easily by FISH on interphase cells. Three samples with the +8 abnormality (pts 6, 7, and 8) showed levels of engraftment of CD45+ cells at week 8 postinjection of 5%, 3%, and 15%. FACS-sorted CD45+ cells from these mice showed the +8 abnormality in 95%, 15%, and 100% of analyzed cells, respectively (Fig 2B). For a fourth sample (pt 5), in which 37% of metaphases in the patient’s diagnostic bone marrow contained trisomy 13, 50% of mouse marrow cells were CD45+ at week 8 and 27% of these were +13 by FISH. Thus, the human cells engrafting in these animals are characteristic of the malignant clone initially identified in patients both morphologically and cytogenetically.
The spleen and peripheral blood of animals injected with 59 of the AML samples were also examined for the presence of human leukemic cells. Although in every case the proportion of human cells detected was lower in spleen and blood than in the marrow (mean percent human cells, 2.7%, 3.0% and 12.0%, respectively) there was a direct correlation between the percent AML cells in each of these tissues (r = .63, .76, and .85 for comparison of percent human cells in marrow and spleen, marrow and blood, and spleen and blood, respectively; P< .001, Student t-test). All of the 16 patient samples where the proportion of human cells in marrow was greater than 10% had AML cells easily detected in spleen and 15 also had human leukemic cells detected in blood.
Treatment of mice with human cytokines does not improve the overall ability of AML samples to engraft NOD-SCID mice.
The original description of growth of human AML cells in immunodeficient (SCID) mice had suggested that repeated injections of human cytokines were necessary to achieve high levels of engraftment. Although this suggestion is consistent with the known cytokine-responsiveness of human AML cells in vitro, in the current study we discovered that 13 of the 61 samples showed ≥25% human leukemic cells in mouse marrow 8 weeks postinjection without treatment of the mice with any human growth factors. Nevertheless, because we were unable to show engraftment of all samples tested and the level of engraftment of human cells was low in a number of others, we studied the ability of cytokine injections to enhance the levels of human AML cells detected in NOD/SCID mice. Because greater than 90% of AML blast samples will proliferate in response to the combination of IL-3 and SF as measured in short-term 3H-thymidine incorporation assays,2 we chose to test these growth factors for their effect on AML cell growth in mice. 107 cells per mouse from different AML samples were injected into groups of 4 mice each. Four weeks after injection of AML cells, 1 animal in each cohort was killed. For 36 AML samples, the bone marrow of this mouse contained less than 25% CD45+ cells. After this had been determined, 1 of the 3 remaining mice in these cohorts began to receive 6 μg of human IL-3 and 10 μg of human SF intraperitoneally Monday, Wednesday, and Friday, while the second mouse received IL-3 only according to the same dose and schedule, and the third mouse continued to not receive any cytokines. Cytokine levels in the serum of a treated mouse 1.5 hours postinjection were 8,000 pg/mL of IL-3 and greater than 100,000 pg/mL of SF, while levels at 48 hours postinjection and immediately before the next scheduled dose of cytokine(s) had decreased to undetectable levels for IL-3 and 55 pg/mL of SF. When these groups of 3 mice were analyzed at week 8 after initial injection of AML cells, the mean ± SEM proportions of human cells in mouse bone marrow were not significantly different for animals receiving or not receiving human cytokines (2.6% ± 1.0% for animals that never received cytokines [n = 36], 3.5% ± 1.7% for animals treated with IL-3 only [n = 19], and 2.6% ± 0.9% for animals treated with IL-3 and SF [n = 36]).
Although these results suggested that cytokines of the type and dose injected were ineffective in enhancing AML cell growth in mice, there were 4 samples in which comparison of the individual cytokine-treated and untreated mice suggested a possible enhancement of engraftment with the combination of IL-3 and SF. Thus, the above experiment was repeated with these cells with larger numbers of mice in the treated and untreated groups. Table 2 shows the results from these 4 experiments. In no case was the difference between mice treated or not treated with cytokines statistically significant.
Human Cytokine Injections Do Not Enhance the Growth of AML Cells in NOD/SCID Mice
| Patient . | Mean % CD45+Cells in Mouse BM ± SEM (n) . | P . | |
|---|---|---|---|
| No Cytokines . | IL-3 + SF* . | ||
| 1 | 5.8 ± 2.2 (4) | 2.2 ± 1.4 (4) | .22 |
| 2 | 33.0 ± 15.8 (3) | 10.9 ± 4.1 (3) | .29 |
| 3 | 13.0 ± 6.1 (6) | 16.2 ± 9.3 (4) | .79 |
| 4 | 0.25 ± 0.18 (2) | 6.5 ± 4.2 (3) | .27 |
| Patient . | Mean % CD45+Cells in Mouse BM ± SEM (n) . | P . | |
|---|---|---|---|
| No Cytokines . | IL-3 + SF* . | ||
| 1 | 5.8 ± 2.2 (4) | 2.2 ± 1.4 (4) | .22 |
| 2 | 33.0 ± 15.8 (3) | 10.9 ± 4.1 (3) | .29 |
| 3 | 13.0 ± 6.1 (6) | 16.2 ± 9.3 (4) | .79 |
| 4 | 0.25 ± 0.18 (2) | 6.5 ± 4.2 (3) | .27 |
Human IL-3 and SF were injected intraperitoneally at a dose of 6 μg and 10 μg, respectively, Monday, Wednesday, and Friday of each of the 4 weeks before killing. Mice were analyzed a total of 8 weeks after injection of AML cells.
Factor-independent growth of AML-CFC predicts AML cell growth in mice.
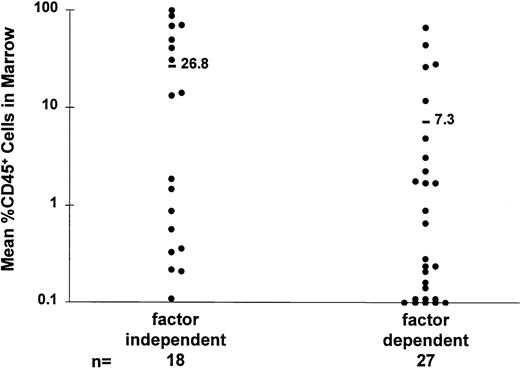
A subset of AML cells from most patient samples will form colonies of blast cells when placed in semisolid medium with a source of cytokines.1 However, the growth of these AML-CFC from some patient samples appears to be relatively factor-independent.2,32 33 When 45 of the AML samples that were tested in mice were placed in methylcellulose assay containing serum but no other source of cytokines, 17 developed ≥5 colonies per 105 cultured cells. One additional patient showed less than 5 colonies but equivalent numbers of small clusters both with and without cytokines. These 18 samples were considered to show factor-independent AML-CFC growth. In 25 cases ≤1 colony formed per 105 cells without growth factors, but when cytokines were added to cultures, colonies formed in every case. In the remaining 2 cases, 2 or 3 colonies per 105 cells formed without cytokines but there was a greater than 10-fold increase in colony numbers when cytokines were added. The latter 27 cases were considered to be factor dependent. When the ability of AML samples that were either factor dependent or independent in colony assays were compared for their ability to grow in mice, there was a significant difference (P = .03) with factor-independent samples showing higher proportions of human cells in mouse bone marrow than factor-dependent samples (Fig 3).
AML-CFC factor independence is associated with increased growth of AML cells in mice. Engraftment levels obtained from samples which could be classified as either growth-factor dependent or independent in methylcellulose colony assays are compared. Samples that were factor independent showed a significantly higher mean level of engraftment than those which were factor dependent (P = .03).
AML-CFC factor independence is associated with increased growth of AML cells in mice. Engraftment levels obtained from samples which could be classified as either growth-factor dependent or independent in methylcellulose colony assays are compared. Samples that were factor independent showed a significantly higher mean level of engraftment than those which were factor dependent (P = .03).
Growth-factor mRNA expression in AML blasts predicts high-level engraftment in mice.
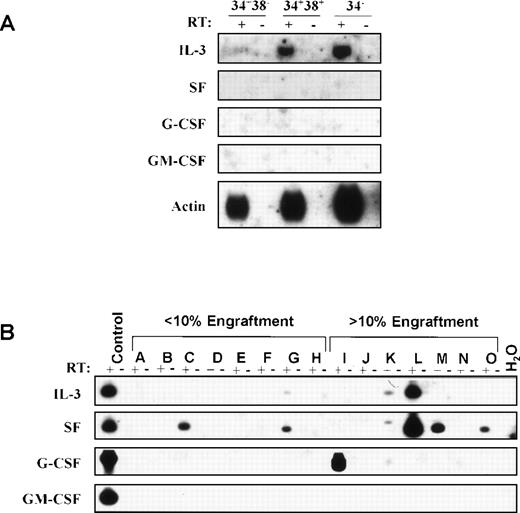
To assess the possibility that autocrine growth-factor production might be associated with differences in the growth of human leukemic cells in mice, reverse transcriptase (RT)-PCR was used to generate total cDNA from 19 AML samples where levels of engraftment in NOD/SCID mice had previously been determined. If hybridization of Southern blots of the total cDNA with probes specific for the 4 candidate cytokines failed to show evidence of expression of these genes, a second round of PCR using primers specific for the human growth factors SF, IL-3, GM-CSF, and G-CSF was performed as described in Materials and Methods. IL-3 expression was detected in 4 AML samples, SF expression in 6, and G-CSF expression in 2. In 3 of these samples both IL-3 and SF expression was detected. When leukemic blasts from patient 8 in Table 1 which showed factor-independent colony growth were sorted into subpopulations based on their expression of CD34 and CD38, 80% of the cells in each fraction was cytogenetically abnormal by FISH.21 IL-3 expression was detected in all 3 of the subpopulations: CD34+CD38−, CD34+CD38+, and CD34− on Southern blotting of total cDNA (Fig 4A). Among the 19 samples tested for growth-factor gene expression, 9 showed greater than 10% human AML cells in mouse marrow 8 weeks after injection of 107 leukemic blasts. Seven of these 9 had cDNA detected for 1 or more of the 4 cytokines evaluated. In constrast, only 2 of the remaining 10 samples that engrafted to levels of less than 10% under the same conditions had detectable cytokine message (Fig 4). The difference in proportion of samples with detectable cytokine expression between those with greater than or less than 10% engraftment in NOD/SCID marrow was significant by χ2analysis (P < .02). Six of the 9 samples in which cytokine expression was detected produced factor-independent AML-CFC growth, while 3 of 10 cytokine-negative samples were factor independent in this assay (P < .1).
Growth-factor mRNA expression in AML blasts. RT-PCR was used to generate total cDNA from AML samples. (A) Southern blots of total cDNA from the CD34+CD38−, CD34+CD38+, and CD34−fractions of cells from pt 8 in Table 1 hybridized with probes specific for IL-3, SF, G-CSF, GM-CSF and, as a positive control, β-actin. IL-3 expression was detected in all 3 subpopulations. SF, G-CSF, and GM-CSF expression was undetectable. RT, reverse transcriptase. (B) Total cDNA from 15 AML samples was subjected to a second round of PCR using cytokine specific primers. Patients A through H showed less than 10% human AML cells in mouse marrow 8 weeks after injection of 107 cells; patients I through O showed greater than 10% human AML cells in mouse marrow under the same conditions. For each cytokine, the positive control was a murine cell line transfected with the corresponding human cytokine cDNA. Southern blots of PCR products were hybridized with the corresponding cytokine-specific probes. Expression of 1 or more cytokines was detected in 2 of the 8 samples shown that achieved less than 10% engraftment, and in 5 of the 7 samples shown that achieved greater than 10% engraftment. In a separate experiment, 2 additional samples with less than 10% engraftment showed no detectable growth-factor expression while 1 sample with greater than 10% engraftment showed expression of G-CSF message.
Growth-factor mRNA expression in AML blasts. RT-PCR was used to generate total cDNA from AML samples. (A) Southern blots of total cDNA from the CD34+CD38−, CD34+CD38+, and CD34−fractions of cells from pt 8 in Table 1 hybridized with probes specific for IL-3, SF, G-CSF, GM-CSF and, as a positive control, β-actin. IL-3 expression was detected in all 3 subpopulations. SF, G-CSF, and GM-CSF expression was undetectable. RT, reverse transcriptase. (B) Total cDNA from 15 AML samples was subjected to a second round of PCR using cytokine specific primers. Patients A through H showed less than 10% human AML cells in mouse marrow 8 weeks after injection of 107 cells; patients I through O showed greater than 10% human AML cells in mouse marrow under the same conditions. For each cytokine, the positive control was a murine cell line transfected with the corresponding human cytokine cDNA. Southern blots of PCR products were hybridized with the corresponding cytokine-specific probes. Expression of 1 or more cytokines was detected in 2 of the 8 samples shown that achieved less than 10% engraftment, and in 5 of the 7 samples shown that achieved greater than 10% engraftment. In a separate experiment, 2 additional samples with less than 10% engraftment showed no detectable growth-factor expression while 1 sample with greater than 10% engraftment showed expression of G-CSF message.
Kinetics of engraftment.
The kinetics with which human leukemic cells engraft and proliferate in NOD/SCID mice were examined in 3 experiments, each performed with a different patient sample. Animals injected with 1 × 107 cells were killed at various times postinjection, the marrow from 4 long bones analyzed for CD45+ cells, and the calculated total number of human cells present in the mice plotted over time as shown in Fig 5. Human cells were detectable in 10- to 100-fold lower numbers than the number initially injected 2 days postinjection. Thereafter, a rapid expansion of CD45+ cell numbers was seen in the bone marrow which continued throughout the 8-week period of assessment. The fold-increase in human cells between 2 days and 8 weeks postinjection ranged from 20- to almost 5,000-fold. These data suggested that a relatively small number of cells in the initial inoculum was responsible for the growth and maintenance of leukemic cells in the animals.
Kinetics of AML cell growth in NOD/SCID mice. Animals injected with 107 cells from pts 6, 8, and 11 were killed at various timepoints postinjection and the total number of CD45+ cells per mouse was determined by FACS and plotted over time. A continuous expansion in cell numbers throughout the 8-week-period of assessment was seen.
Kinetics of AML cell growth in NOD/SCID mice. Animals injected with 107 cells from pts 6, 8, and 11 were killed at various timepoints postinjection and the total number of CD45+ cells per mouse was determined by FACS and plotted over time. A continuous expansion in cell numbers throughout the 8-week-period of assessment was seen.
Limiting dilution analysis of AML progenitors engrafting in NOD/SCID mice.
In previous studies we have used limiting dilution analysis to show that the frequency of AML progenitors that initiate long-term culture (AML LTC-IC) is 10- to greater than 100-fold lower than the frequency of AML-CFC in the same patient sample, and that each LTC-IC will generate more than 1 clonogenic cell progeny over 5 weeks in culture.2 Using the same principles, we determined the frequency of cells capable of initiating growth of leukemic cells in NOD/SCID mice (NOD/SCID leukemia-initiating cells or NOD/SL-IC). Five different doses of the same AML sample ranging from 1 × 105 to 1 × 107 cells were injected into cohorts of up to 8 mice each. Using Poisson statistics, the frequency of NOD/SL-IC in a given sample was calculated based on the frequency of mice in which CD45+ cells could not be detected in bone marrow 8 weeks after injection of each cell dose. Because the limit of sensitivity of FACS analysis for CD45+ cells was ≈0.5%, apparently negative FACS results were confirmed by hybridizing Southern blots of genomic DNA from mouse tissues with a human-specific probe for endogenous retroviral sequences (HERV-H). As described in Materials and Methods, this technique allows detection of less than 0.1% human cells in mouse tissues. The results of limiting dilution experiments with 6 AML samples (pts 5 through 10) are shown in Table 3. The frequencies of NOD/SL-IC ranged from 0.7 to 45 per 107 cells. This number was 214- to 800-fold lower than the frequency of LTC-IC determined previously for 3 of the same 6 patient samples.2
Frequency of NOD/SL-IC in AML Samples
| Patient . | NOD/SL-IC/107 (95% confidence interval) . | LTC-IC/107 3-150 (95% confidence interval) . |
|---|---|---|
| 5 | 21 (11-38) | ND |
| 6 | 1.8 (0.8-3.8) | 500 (367-707) |
| 7 | 0.7 (0.2-2.6) | 150 (102-227) |
| 8 | 1.5 (0.7-3.0) | 1,200 (820-1,792) |
| 9 | 5 (2.7-9.9) | ND |
| 10 | 45 (21-100) | ND |
| Patient . | NOD/SL-IC/107 (95% confidence interval) . | LTC-IC/107 3-150 (95% confidence interval) . |
|---|---|---|
| 5 | 21 (11-38) | ND |
| 6 | 1.8 (0.8-3.8) | 500 (367-707) |
| 7 | 0.7 (0.2-2.6) | 150 (102-227) |
| 8 | 1.5 (0.7-3.0) | 1,200 (820-1,792) |
| 9 | 5 (2.7-9.9) | ND |
| 10 | 45 (21-100) | ND |
Abbreviation: ND, not determined.
Data from Ailles et al.2
After determining the frequency of NOD/SL-IC in these samples, it was possible to use these values to quantitate the numbers of cell progeny of different types produced per NOD/SL-IC. The average number of AML blast cell progeny produced by each NOD/SL-IC at week 8 postinjection ranged from 1.1 × 106 to 7.5 × 106cells/NOD/SL-IC (mean ± SEM, 3.7 × 106 ± 1.0 × 106) (Table 4).
Cell Production per NOD/SL-IC 8 Weeks Postinjection Into Mice
| Patient . | Blast Cells . | AML-CFC . | AML-LTC-IC . | |||
|---|---|---|---|---|---|---|
| No. Produced (×106) . | FISH4-150 . | No.Produced . | FISH4-150 . | No.Produced . | FISH4-150 . | |
| 5 | 1.2 | 21/78 | ||||
| 6 | 3.4 | 40/42 | 497 | 7/7 | 299 | ND |
| 7 | 4.0 | 13/85 | ||||
| 8 | 5.1 | 31/31 | 4,877 | 30/30 | 36 | 3/3 |
| 9 | 7.5 | ND | ||||
| 10 | 1.1 | ND | ||||
| Patient . | Blast Cells . | AML-CFC . | AML-LTC-IC . | |||
|---|---|---|---|---|---|---|
| No. Produced (×106) . | FISH4-150 . | No.Produced . | FISH4-150 . | No.Produced . | FISH4-150 . | |
| 5 | 1.2 | 21/78 | ||||
| 6 | 3.4 | 40/42 | 497 | 7/7 | 299 | ND |
| 7 | 4.0 | 13/85 | ||||
| 8 | 5.1 | 31/31 | 4,877 | 30/30 | 36 | 3/3 |
| 9 | 7.5 | ND | ||||
| 10 | 1.1 | ND | ||||
Abbreviation: ND, not done.
FISH, number abnormal/total number of cells analyzed.
Assays for AML-CFC were performed on bone marrow cells from mice engrafted with cells from pts 6 and 8. The number of CFC produced at week 8 postinjection per NOD/SL-IC was 497 and 4,877 for cells from pts 6 and 8, respectively. FISH analysis of cells from colonies grown from such samples showed that 100% of AML-CFC carried the +8 abnormality characteristic of the leukemic clone (Fig 2B, Table 4). These same samples were also analyzed for the presence of AML-LTC-IC. For samples from pts 6 and 8 the average numbers of LTC-IC produced per NOD/SL-IC was 599 and 36, respectively, with FISH analysis confirming the presence of the +8 abnormality in AML LTC-IC from patient 8 (Table 4).
Secondary transplants of NOD/SL-IC.
To determine if AML progenitors capable of engrafting in mice persisted for significant time periods posttransplantation and to quantitate their numbers, NOD/SCID animals injected with AML cells 3 to 4 weeks previously were killed and their bone marrow cells transplanted into secondary recipients. When bone marrow from the secondary recipients was analyzed 8 to 12 weeks later, 2 of 3 mice injected with cells from primary recipients of AML cells from patients 5 and 10 and 1 of 3 mice injected with marrow from a recipient of patient 9 cells showed engraftment with human cells (Table 5). Using Poisson statistics, it can be estimated from this data that the marrow of the primary mice contained approximately 10 to 20 NOD/SL-IC at the time of secondary transfer. Because the primary mice were injected with AML cells from 3 samples for which the frequency of NOD/SL-IC had previously been determined at limiting dilution (Table3), it was possible to compare the number of NOD/SL-IC injected into primary mice initially with the number recovered 3 to 4 weeks later. As shown in Table 5, at least in the case of cells from patients 5 and 9, the number of NOD/SL-IC was apparently well preserved over that time period. Furthermore, FISH performed on CFC grown from the bone marrow of a secondary recipient of cells from patient 5 harvested 12 weeks posttransplant carried the +13 cytogenetic abnormality characteristic of the leukemic clone in 8 of 9 colonies, confirming the malignant nature of these progenitors.
Maintenance of NOD/SL-IC Numbers In Vivo
| Patient . | No.NOD/SL-IC per 1° Mouse Day 0 . | % BM From 1° Mouse Injected per 2° Mouse5-150 . | No.Positive 2° Mice . | % CD45+ Cells in Positive 2° Mice . | Estimated No. NOD/SL-IC in 1° Mouse at Week 3-45-151 . |
|---|---|---|---|---|---|
| 5 | 21 | 5 | 2/3 | 1.9, 2.6 | 20 |
| 9 | 5 | 5 | 1/3 | 1.2 | 10 |
| 10 | 45 | 10 | 2/3 | 1.8, 3.0 | 10 |
| Patient . | No.NOD/SL-IC per 1° Mouse Day 0 . | % BM From 1° Mouse Injected per 2° Mouse5-150 . | No.Positive 2° Mice . | % CD45+ Cells in Positive 2° Mice . | Estimated No. NOD/SL-IC in 1° Mouse at Week 3-45-151 . |
|---|---|---|---|---|---|
| 5 | 21 | 5 | 2/3 | 1.9, 2.6 | 20 |
| 9 | 5 | 5 | 1/3 | 1.2 | 10 |
| 10 | 45 | 10 | 2/3 | 1.8, 3.0 | 10 |
1° mice were killed 3 to 4 weeks postinjection of AML cells. Marrow harvested from these animals was injected into secondary recipients that were killed for analysis 8 weeks later.
Using Poisson statistics it was estimated that when 2/3 of 2° mice showed engraftment with human cells on average 1 NOD/SL-IC was present in the fraction of 1° mouse marrow initially injected into 2° recipients.
DISCUSSION
Over the last few years, evidence has been accumulating to support the hypothesis that malignant transformation in AML typically occurs in a rare primitive hematopoietic progenitor with many of the characteristics associated with normal multipotential hematopoietic precursors or ‘stem cells.’ These characteristics include the ability to initiate long-term hematopoiesis in culture,2 the expression of cell-surface antigens such as CD34,17 and the relative lack of expression of molecules such as CD38, CD71, and HLA-DR that are expressed by more mature, lineage-committed progenitors,15,16 and the ability to engraft and proliferate in the marrow of immunodeficient mice.15-17 The availability of an in vivo assay for cells responsible for maintenance of the malignant clone has obvious importance for the development of new therapeutic strategies and for more basic studies aimed at a further understanding of leukemic stem cell biology.
The first description of an in vivo assay for human AML progenitors in immunodeficient mice used sublethally irradiated SCID animals injected with human cytokines.14 Although this assay for SL-IC was a clear demonstration of the feasibility of this approach, the somewhat low and inconsistent levels of engraftment obtained limited the usefulness of the technique. We and others have found that the use of NOD/SCID mice as hosts for leukemic progenitors directly isolated from AML patients has greatly enhanced the sensitivity and reproducibility of the NOD/SL-IC assay over that which can be obtained with SCID mice and a variety of other immunodeficient strains (data not shown).15 As shown by the data presented here, 8 weeks after IV injection of 107 light-density peripheral blood cells from patients with newly diagnosed AML, human CD45+cells were usually easily detected in NOD/SCID mouse bone marrow. The leukemic origin of these cells was obvious from their characteristic morphology and could be confirmed by demonstration of chromosomal abnormalities that had previously been identified in the patient’s diagnostic bone marrow cytogenetic analysis. Thus, the use of these animals allows the routine detection and quantitation of primitive leukemic progenitors from most patient samples.
In preliminary experiments, we observed that the proportion of human cells detected in mouse marrow increased with the number of AML cells initially injected (data not shown). Thus, to compare the ability of various patient samples to grow in mice, a standardized cell dose was selected. The dose of 107 cells was chosen because of limitations in cell numbers from some samples and because this number of cells appeared to be adequate to generate reproducible engraftment from many samples. However, as indicated in Table 3, the frequency of NOD/SL-IC in some patient samples is less than 1 in 107cells. Thus, the low or undetectable numbers of human cells observed in some cases may reflect the injection of inadequate cell numbers. The 8-week endpoint for most of these experiments was chosen after initial studies had indicated that the level of engraftment continued to increase steadily until that timepoint and to provide a standard endpoint for comparison of the growth characteristics in different samples. However, it is likely that choice of a different timepoint would have yielded somewhat different overall results. In a limited number of experiments it was possible to show continued expansion of AML cell numbers up to 12 to 14 weeks postinjection into mice. Unfortunately, because of the inherent tendency of NOD/SCID mice to spontaneously develop malignant thymomas as they age, it is difficult to continue these experiments much beyond that timepoint.6
Since the original description of the ability of AML cells to form colonies in semisolid media, it has been recognized that AML progenitors share at least some of the cytokine-responsiveness of their normal cell counterparts.1 Although some cytokines that stimulate normal and malignant myelopoiesis show species cross-reactivity between mice and humans, a number of key molecules, such as IL-3, do not, and others, such as SF, show less potency on cells from a different species of origin.34,35 Thus, it seemed reasonable to suppose that provision of relevant human growth factors would enhance the growth of human AML cells in mice. However, it has also been well-documented that progenitors in many AML samples can exhibit varying degrees of factor-independent growth. In many cases, this is associated with autocrine growth-factor production.36-39 Thus, it was not certain whether human cytokines would be necessary to allow the growth of all leukemic samples in mice. In fact, using the protocol established in this study, 17 of the 61 samples tested showed more than 10% replacement of NOD/SCID marrow with leukemic cells in the absence of any human cytokine supplements. In comparing the growth-factor requirements for 45 of these 61 AML samples in colony assays with their ability to grow in mice, we discovered that most (9 of 14) samples which showed more than 10% replacement of mouse marrow with AML cells demonstrated factor-independent growth in AML-CFC assays. To explore the possibility that autocrine growth-factor production might be associated with more rapid growth of human AML cells in NOD/SCID mice, RT-PCR was used to amplify mRNA for 4 candidate growth factors from AML blasts. The 4 factors (SF, IL-3, G-CSF, and GM-CSF) were chosen because more than 90% of AML samples will respond to 1 or more of these factors alone or in combination in in vitro assays. In addition, these cytokines had all been shown to be produced in an autocrine fashion by some leukemia samples in previous studies.32,38,40-42 However, AML blasts may produce a variety of other growth factors and their receptors.33 Thus, the data shown in Fig 4 represent a minimal estimate of the autocrine factor production in these cells. Nevertheless, consistent with previous data, we found that most samples expressing 1 or more of the 4 growth factors studied exhibited factor-independent growth in AML-CFC assays.32 33 Even more striking was the association between growth factor gene expression and high-level engraftment of AML cells in NOD/SCID mice.
In this study we chose to inject IL-3 and SF thrice weekly intraperitoneally into mice for 4 weeks before killing of the animals for analysis. In previous experiments testing a variety of growth factors alone and in combination, we had found that this combination stimulated maximal proliferation of AML blasts in short-term assays and that AML LTC-IC also responded to these cytokines.2Initiation of cytokine injections was delayed until 4 weeks postinjection of AML cells to allow detection of factor-independent AML cell growth in an initial test animal and thereby avoid cytokine injections if they were unnecessary. In addition, human growth factor injections for 2 weeks before killing of NOD/SCID mice previously injected with adult human bone marrow cells had been shown to enhance detection of normal myeloid progenitors.11 Although the dose of both factors administered was high enough to achieve substantial serum levels immediately postinjection, their relatively short half-life resulted in little or no detectable cytokine by the time of the next injection. Thus, although it is clear that the dose and schedule of cytokine administration chosen did not improve the growth of human AML cells in NOD/SCID mice, beginning the injections earlier or giving them more frequently or at higher dosages may have produced different results. Other investigators have suggested that there is a relationship between the dose of hIL-3 administered and the level of AML cell engraftment observed in SCID mice.43 The fact that leukemic cells which showed cytokine-dependent colony growth and lacked detectable growth-factor mRNA expression often failed to grow well in mice also suggests that an alternative strategy for human growth-factor administration may be necessary to optimize the sensitivity of the NOD/SL-IC assay. We are particularly interested in the possibility that immunodeficient mice transgenic for human cytokine genes may provide improved hosts for human AML progenitors.44,45 In addition, newly developed mouse strains with more profound immunodeficiency than the NOD/SCID animals may enhance engraftment with both normal and malignant human hematopoietic cells.46
The proportion of leukemic cells detected in mouse marrow after injection of AML samples known to contain chromosomal rearrangements associated with a good clinical prognosis was generally lower than that observed after injection of cells with rearrangements associated with a poor prognosis (Fig 1A). Similarly, as shown in Fig 1B, the levels of engraftment were higher with samples from patients with AML FAB subtypes M1, M4, and M5 than with AML-M3 and M2 samples. Clinically, AML-M3 has a relatively favorable prognosis compared with AML-M5, which is associated with an aggressive course and poor overall survival.47 48 In NOD/SCID mice, human leukemic cells will also disseminate from bone marrow into both the peripheral blood and spleen, and this occurs as bone marrow infiltration becomes more extensive. Although most of the animals in this study were killed before advanced tumor growth could cause their death, in some cases unexpected deaths were associated with extensive infiltration of AML cells in marrow and other hematopoietic tissues. Thus, the development and spread of leukemia in NOD/SCID mice resembles in many ways the clinical disease in patients.
NOD/SL-IC are rare progenitors, as shown at limiting dilution on Table3. These frequencies are consistent with those reported by others using similar techniques and are not greatly different from the frequencies determined for NOD/SCID competitive repopulating units (CRU) in normal human bone marrow.11 These frequencies are, however, several hundred-fold lower than the frequencies previously determined for AML LTC-IC detected in 5-week-old cultures.2 These relative frequencies are similar to those previously determined for normal CRU and LTC-IC.10,49,50 The proliferative capacity of NOD/SL-IC is high. Each of these progenitors is capable of producing more than 106 leukemic blasts and hundreds of AML-CFC (Table 4). In 2 cases it was possible to show that AML LTC-IC were also produced in large numbers. These data contrast with the average cell production for AML LTC-IC, which for cells from patients 6 and 8 had been previously determined as 1.8 and 1.2 AML-CFC per LTC-IC, respectively.2 One interpretation of these differences in frequency and proliferative capacity is that they indicate that the NOD/SL-IC and AML LTC-IC assays detect different populations of progenitor cells. Studies of retroviral-mediated gene transfer efficiencies and cell-surface phenotype have suggested to some investigators that this may be the case for normal LTC-IC and progenitors that are detected in NOD/SCID mice.51 However, using similar comparisons, others have obtained data consistent with a close relationship between these 2 cell types.49,52 Recent studies of our own have also shown that the majority of AML progenitors that initiate long-term malignant hematopoiesis in culture share the cell-surface phenotype of NOD/SL-IC and are predominantly CD71− and HLA-DR− as well as CD38− and CD34+.16 21 Thus, it appears likely that the LTC-IC and NOD/SL-IC assays detect overlapping, if not identical, populations of progenitors. The apparent differences in the frequency and proliferative capacity of the cells detected is likely to be at least partly explained by differences in the sensitivity of the 2 assays and their relative ability to support the proliferative potential of the cells detected.
Under the conditions used in these experiments, NOD/SL-IC numbers are maintained at relatively constant levels for at least 3 to 4 weeks posttransplantation into mice (Table 5) while other investigators have suggested that an absolute expansion of their numbers may be possible in vivo.15 This apparent ability to self-renew their own numbers combined with the potential to differentiate to produce large numbers of more committed progenitors and mature leukemic blasts suggests NOD/SL-IC as candidate leukemic ‘stem cells.’ These primitive characteristics and the ability to sensitively detect and quantitate NOD/SL-IC from the majority of AML samples suggests the use of this assay for preclinical evaluation of novel therapeutic strategies53 and to study the relative importance of specific molecular abnormalities in the in vivo behavior of the leukemic clone.
Supported by grants from the National Cancer Institute of Canada with funds from the Terry Fox Foundation and the B.C. Health Research Foundation. L.E.A. was the recipient of a Roman N. Babicki Fellowship in Medical Research.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Donna E. Hogge, MD, PhD, Terry Fox Laboratory, B.C. Cancer Agency, 601 W 10 Ave, Vancouver, BC Canada V5Z 1L3; e-mail: donna@terryfox.ubc.ca.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal