Abstract
Human bone marrow endothelial cells immortalized with the T antigen of SV40 (TrHBMEC) have previously been characterized by us with regard to their properties that are similar to primary marrow endothelial cells and their utility as a model system. We now report that TrHBMEC express a recently discovered signal transduction molecule termed RAFTK (related adhesion focal tyrosine kinase), also called Pyk2 or CAK-β. RAFTK, the second member of the focal adhesion kinase (FAK) family, is known to be activated in response to calcium flux in neuronal cells and integrin stimulation in megakaryocytes and B cells. We have studied the effects of cytokines on RAFTK activation in TrHBMEC. Treatment of TrHBMEC with the vascular endothelial growth factor (VEGF ), as well as the VEGF-related protein (VRP), the recently identified ligand for the FLT-4 receptor, resulted in enhanced tyrosine phosphorylation of RAFTK. Similar changes in RAFTK phosphorylation were observed upon stimulation of TrHBMEC with basic fibroblast growth factor (bFGF ) or oncostatin M (OSM). Stimulation of these cells with growth factors also resulted in an increase in RAFTK activity and the c-Jun NH2 -terminal kinase (JNK). RAFTK coimmunoprecipitated with the cytoskeletal protein paxillin through its C-terminal proline-rich domain in TrHBMEC. These results suggest that, in marrow endothelium, activation of RAFTK by VEGF, VRP, OSM, and bFGF represents a new element in the signal transduction pathways used by these growth factors and likely acts to coordinate signaling from their surface receptors to the cytoskeleton, thereby modulating cell growth and function.
BONE MARROW endothelial cells are an important component of the stromal compartment that supports hematopoiesis. It has recently been possible to isolate and immortalize in vitro human bone marrow endothelial cells, thereby allowing for in vitro studies of cell function that previously were not feasible in these cells.1-3 We have derived such a permanent bone marrow endothelial cell line termed TrHBMEC from an adult female donor's cells by transfection with the SV40 T antigen under the control of a truncated vimentin promoter.4,5 TrHBMEC manifest normal characteristics of the cell of origin, including expression of von Willebrand factor, P-selectin, CD31, CD34, CD44, very late antigen-5 (VLA-5), and intercellular adhesion molecule-2 (ICAM-2).4 These cells respond to, but do not require, endothelial cell growth factors for proliferation and they also maintain contact inhibition in culture. After treatment with stimulatory cytokines, TrHBMEC increase surface expression of E-selectin, vascular cell adhesion molecule-1 (VCAM-1), and ICAM-1 in a manner similar to normal bone marrow endothelium and support adhesion of hematopoietic precursors. TrHBMEC therefore provide a useful model to study functions of marrow endothelium.
Although considerable data have been generated on signal transduction in other types of endothelium, particularly that derived from the umbilical vein,6-9 there is little information on signal transduction pathways in bone marrow endothelial cells. Defining such pathways may provide insights into the mechanisms by which specific cytokines, elaborated by neighboring cells within the marrow microenvironment, modulate bone marrow endothelial growth and function. To that end, we have characterized TrHBMEC for expression of several known and novel growth factor receptors and intracellular signaling molecules. We observed that TrHBMEC express both the FLK-1 receptor for the vascular endothelial growth factor (VEGF )10,11 as well as the FLT-4 receptor for the recently identified member of the VEGF family termed VEGF-related protein (VRP).12-15 In addition, TrHBMEC express a newly identified signaling molecule termed related adhesion focal tyrosine kinase (RAFTK),16 also known as Pyk217 or CAK-β.18
RAFTK is a member of the focal adhesion kinase (FAK) family and has a deduced amino acid structure quite similar to FAK.19,20 RAFTK/Pyk2 has previously been reported to be expressed in brain and hematopoietic cells and appears to link calcium-, integrin-, and cytokine-mediated signaling pathways to the cytoskeleton.16-18,21 Recent studies indicate that the c-Jun NH2 -terminal kinase (JNK), also known as stress-activated protein kinase (SAPK), is involved in the downstream signaling events of RAFTK/Pyk2 activation in neuronal cells.22 The JNK kinases participate in cellular proliferation via the modulation of transcriptional activation factors such as AP-1.23-26 After the treatment of TrHBMEC with a variety of cytokines, we observed enhanced phosphorylation and activation of RAFTK and its association with the cytoskeletal protein paxillin. This association of RAFTK with paxillin appears to be mediated via the carboxyl domain of the kinase. Furthermore, treatment of TrHBMEC with VEGF, VRP, or oncostatin M (OSM) increased JNK activity in TrHBMEC.
These observations suggest that several cytokines believed to modulate the growth and function of bone marrow endothelium use the recently identified RAFTK signaling molecule to transduce signals to the cytoskeleton and downstream to JNK.
MATERIALS AND METHODS
Cells and cell culture.TrHBMEC were derived from bone marrow aspirates and prepared as previously described.2,4 Cells were grown on gelatin-coated plasticware in Dulbecco's modified Eagle's medium (DMEM) with 5% fetal calf serum (FCS), 1% glucose, 3 mmol/L glutamine, 10 mmol/L HEPES, vitamins, 50 μg/mL penicillin, and 50 μg/mL streptomycin. Cultures were grown until near confluence before the different treatments in the signaling studies described below. Normal human umbilical vein endothelial cells (HUVEC) carried in endothelial cell growth medium (EGM; Clonetics Corp, San Diego, CA) were used as a positive control for FLK-1 expression. Human erythroleukemia cells (HEL-JW) grown in RPMI-1640 with 10% FCS, 50 μg/mL penicillin, and 50 μg/mL streptomycin were used as a positive control for FLT-4 expression.27
Reagents and antibodies.RAFTK antibodies were generated using glutathione S-transferase (GST)-fusion proteins to the various domains of the molecule and by immunizing New Zealand rabbits as previously described.21 Using an enzyme-linked immunosorbent assay (ELISA), sera were screened for specific binding to the RAFTK protein. Serum R-4250 was chosen for further studies based on its titer in the ELISA. This antiserum did not cross-react with FAK and was specific for RAFTK. Antibodies to the VEGF receptor FLK-1, the FLT-4 receptor, paxillin, and JNK and to the recombinant GST-c-Jun amino terminal protein (1-79 amino acids) were obtained from Santa Cruz Biotechnology (Santa Cruz, CA). Monoclonal antiphosphotyrosine antibody (4G10) was obtained from Upstate Biotechnology, Inc (Lake Placid, NY). Electrophoresis reagents were obtained from Bio-Rad Laboratories (Hercules, CA). Phorbol 12-myristate 13-acetate (PMA); the protease inhibitors leupeptin, aprotinin, and α1 anti-trypsin; and all other reagents were obtained from Sigma Chemical Co (St Louis, MO). The recombinant cytokines basic fibroblast growth factor (bFGF ) and OSM were obtained from R&D Systems (Minneapolis, MN). Recombinant VRP, the ligand for the FLT-4 receptor, was expressed and purified from a glioblastoma cell line as previously reported.14 Recombinant VEGF was obtained from Genentech, Inc (South San Francisco, CA). Recombinant OSM was obtained from the AIDS Reagent Bank (Bethesda, MD).
Indirect immunofluorescence.TrHBMEC were cultured on Chamber Slides (LabTek, Naperville, IL) to 90% confluency and then washed twice with ice-cold phosphate-buffered saline (PBS) and fixed for 30 minutes in 4% paraformaldehyde. Cells were next washed 3× with ice-cold PBS and blocked for nonspecific staining using 10% FCS in PBS for 30 minutes on ice. FLT-4 and FLK-1 expression were determined using purified antiserum at a 1:100 dilution for 1 hour on ice. Normal rabbit serum (NRS) was used as a control for nonspecific staining. After washing cells 3× with PBS, cells were stained with secondary antibody conjugated to fluorescein isothiocyanate (FITC; Boehringer Mannheim, Indianapolis, IN) at a 1:500 dilution for 1 hour on ice. After washing 3× with PBS, proteins were visualized and photographed using an inverted fluorescence microscope.
Stimulation of cells.TrHBMEC grown to 80% confluency were serum-starved for 16 to 18 hours and washed twice with Hank's balanced salt solution (GIBCO BRL, Gaithersburg, MD) before PMA or cytokine treatments. TrHBMEC were first treated with PMA to assess the effects of this chemical stimulus known to phosphorylate RAFTK in other cell systems. After a time course of stimulation with PMA was established, the effects of the various cytokines were studied. We treated cells with 100 ng/mL of VEGF, bFGF, and VRP, adding 10 IU/mL of heparin in each case. Treatment with 100 ng/mL OSM was performed in the absence of heparin. Cytokines were added to cultures singly for different time periods. Controls included media with or without 10 IU/mL heparin in the absence of cytokines. After stimulation, the plates were washed and cell lysates were prepared by adding 500 μL modified RIPA buffer (50 mmol/L Tris-HCl, pH 7.4; 1% NP-40; 0.25% sodium deoxycholate; 150 mmol/L NaCl; 1 mmol/L phenylmethyl sulfonyl fluoride [PMSF ]; 10 mg/mL of aprotinin, leupeptin, and pepstatin; 10 mmol/L sodium vanadate; 10 mmol/L sodium fluoride; and 10 mmol/L sodium pyrophosphate) to each dish at various time points. Total cell lysates (TCL) were clarified by centrifugation at 10,000g for 10 minutes. Protein concentrations were determined by protein assay (Bio-Rad Laboratories).
Immunoprecipitation and Western blot analysis.For the immunoprecipitation studies, identical amounts of protein from each sample were clarified by incubation with protein A-Sepharose CL-4B (Pharmacia Biotech, Piscataway, NJ) for 1 hour at 4°C. After the removal of the protein A-Sepharose by brief centrifugation, the samples were incubated with different primary antibodies as detailed below for each experiment for 4 hours or overnight at 4°C. The immunoprecipitations of the antibody-antigen complexes were performed by incubation for 2 hours at 4°C with 75 μL of protein A-Sepharose (10% suspension). Nonspecific bound proteins were removed by washing the Sepharose beads 3× with the modified RIPA buffer and 1× with PBS. Bound proteins were solubilized in 40 μL of 2× Laemmli buffer and further analyzed by immunoblotting. Equal amounts of protein were prepared and samples were separated on 7.5% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and then transferred to nitrocellulose membranes. The membranes were blocked with 5% nonfat milk protein and probed with primary antibody for 2 hours at room temperature (RT) or 4°C overnight. Immunoreactive bands were visualized using horseradish peroxidase-conjugated secondary antibody and the enhanced chemiluminescent system (Amersham Corp, Arlington Heights, IL).
In vitro GST-fusion protein RAFTK C-terminal association assay.The GST fusion protein of the RAFTK C-terminal domain (amino acids 681 through 1,009) was amplified using the polymerase chain reaction technique and cloned into the pGEX-2T expression vector (Pharmacia Biotech, Inc) as previously described. The GST-fusion protein was produced by 1 mmol/L isopropyl β-thiogalactopyranoside induction and purified by affinity chromatography on a glutathione-sepharose column according to the manufacturer's recommendations (Pharmacia Biotech).
For the in vitro association experiments, TCL (1 mg) of the stimulated TrHBMEC were mixed with 5 mg of the purified GST-fusion protein of the RAFTK C-terminal domain and incubated for 1 hour at 4°C on a rotatory shaker. Fifty microliters of the glutathione sepharose 4B beads (Pharmacia Biotech) was added to preabsorb the complex. After incubation for 3 hours at 4°C on a rotatory shaker, the beads were centrifuged and washed 3× with the modified RIPA buffer. The bound proteins were eluted by boiling in Laemmli sample buffer and subjected to SDS-PAGE on a 7.5% gel and to Western blot analysis.
JNK kinase assay.Cell lysates were immunoprecipitated with JNK antibody (Santa Cruz Biotechnology). The immune complexes were washed twice with RIPA buffer and once in kinase buffer (50 mmol/L HEPES, pH 7.4, 10 mmol/L MgCl2 , 100 mmol/L ATP). The complex was then incubated in kinase buffer containing recombinant GST c-Jun 0.2 μg/μL (1-79 amino acids; Santa Cruz Biotechnology) and 5 μCi γ32P-ATP for 30 minutes at RT. The reaction was terminated by adding 2× SDS sample buffer and boiling the sample for 5 minutes at 100°C. Proteins were separated on 12% SDS-PAGE and detected by autoradiography. Rabbit IgG was used as a negative control.
In vitro kinase assay.Cell lysates were immunoprecipitated with RAFTK antiserum. The immunoprecipitated complexes were washed twice with RIPA buffer and once in kinase buffer (20 mmol/L HEPES, pH 7.4, 50 mmol/L NaCl, 5 mmol/L MgCl2 , 5 mmol/L MnCl2 , and 100 mmol/L Na3VO4 ). The immune complex was incubated in kinase buffer containing 25 μg of poly ([Glu:Tyr] [4:1], 20 to 50 kD; Sigma) and 5 μCi γ32P-ATP at RT for 30 minutes. The reaction was stopped by adding 2× SDS sample buffer and boiling the sample for 5 minutes at 100°C. Proteins were then separated on 7.5% SDS-PAGE and detected by autoradiography. Normal rabbit serum was used as a negative control.
RESULTS
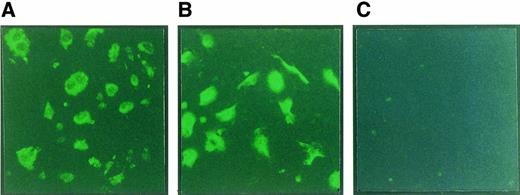
TrHBMEC express FLK-1 and FLT-4 receptors.To characterize the effects of different growth factors on signal transduction pathways in TrHBMEC, we first examined these cells for the expression of different VEGF-type receptors. We focused on the recently identified FLT-4 receptor, which has been reported to be predominantly expressed in lymphatic endothelium, as well as the more ubiquitous VEGF receptor FLK-1. Using indirect immunofluorescence, we observed expression of both the FLK-1 and FLT-4 receptors (Fig 1).
Immunofluorescence staining of FLT-4 and FLK-1 in TrHBMEC. TrHBMEC were cultured in chamber slides and fixed with 4% paraformaldehyde. After blocking, the cells were immunostained with antibodies to FLT-4 (A) or FLK-1 (B), followed by secondary antibodies conjugated with FITC. Normal rabbit IgG was used as a negative control (C). HUVEC were used as a positive control for FLK-1 expression (data not shown).
Immunofluorescence staining of FLT-4 and FLK-1 in TrHBMEC. TrHBMEC were cultured in chamber slides and fixed with 4% paraformaldehyde. After blocking, the cells were immunostained with antibodies to FLT-4 (A) or FLK-1 (B), followed by secondary antibodies conjugated with FITC. Normal rabbit IgG was used as a negative control (C). HUVEC were used as a positive control for FLK-1 expression (data not shown).
These observations were confirmed by immunoprecipitation studies using specific antibodies to each of these receptors (Fig 2A and B). Human umbilical vein endothelial cells (HUVEC) were used as a positive control for FLK-1 expression. HEL cells were used as a positive control for FLT-4 expression.27 NRS and second antibody alone were used as negative controls.
Expression of FLT-4 and FLK-1 in TrHBMEC. TCL (1 mg) from TrHBMEC were immunoprecipitated with the anti–FLK-1 antibody or FLT-4 antibody. Immunoprecipitates were size-fractionated on 7.5% SDS-PAGE, transferred onto a nitrocellulose membrane, and then immunoblotted with FLK-1 or FLT-4 antibodies. For FLK-1 expression, positive controls consisted of the same amounts of TCL from HUVEC. For FLT-4 expression, HEL-JW cells were used as a positive control. Normal rabbit serum and antibody alone were used as negative controls.
Expression of FLT-4 and FLK-1 in TrHBMEC. TCL (1 mg) from TrHBMEC were immunoprecipitated with the anti–FLK-1 antibody or FLT-4 antibody. Immunoprecipitates were size-fractionated on 7.5% SDS-PAGE, transferred onto a nitrocellulose membrane, and then immunoblotted with FLK-1 or FLT-4 antibodies. For FLK-1 expression, positive controls consisted of the same amounts of TCL from HUVEC. For FLT-4 expression, HEL-JW cells were used as a positive control. Normal rabbit serum and antibody alone were used as negative controls.
RAFTK is expressed in TrHBMEC and phosphorylated upon cytokine treatment.We further characterized TrHBMEC for expression of the novel signal transduction molecule RAFTK. This recently identified member of the FAK family is activated in brain and hematopoietic cells and appears to link receptor-mediated signals to the cytoskeleton and JNK signaling pathways.16,17,21,22,28 As shown in Fig 2C, TrHBMEC expressed significant amounts of RAFTK protein as detected by immunoprecipitation and immunoblotting. CMK cells were used as a positive control.21
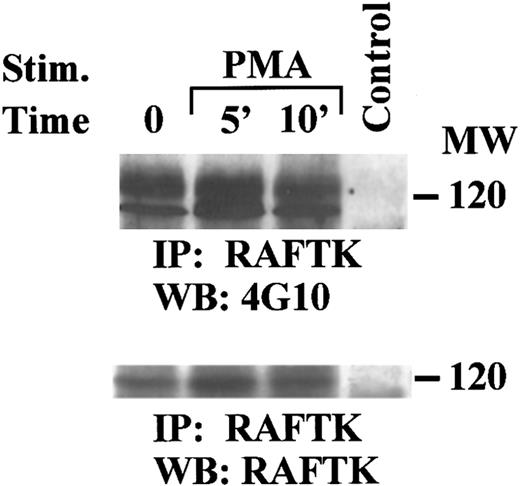
The chemical inducer PMA results in the phosphorylation of RAFTK in human megakaryocytic cells.29 Having observed that RAFTK is expressed in TrHBMEC, we studied whether treatment of these cells with PMA resulted in the phosphorylation of this novel kinase. As shown in Fig 3, there was a time-dependent phosphorylation of RAFTK in response to PMA.
Tyrosine phosphorylation of RAFTK in TrHBMEC by PMA stimulation. Serum-starved TrHBMEC were treated with 20 nmol/L of PMA for 5 or 10 minutes. TCL from treated and untreated cells were immunoprecipitated with the anti-RAFTK antibody. Immunoprecipitates were size-fractionated on 7.5% SDS-PAGE and subjected to serial immunoblotting with antiphosphotyrosine antibody 4G10 (top panel) and anti-RAFTK (bottom panel). NRS was used as a negative control. There was a 200% estimated increase in phosphorylation after PMA treatment.
Tyrosine phosphorylation of RAFTK in TrHBMEC by PMA stimulation. Serum-starved TrHBMEC were treated with 20 nmol/L of PMA for 5 or 10 minutes. TCL from treated and untreated cells were immunoprecipitated with the anti-RAFTK antibody. Immunoprecipitates were size-fractionated on 7.5% SDS-PAGE and subjected to serial immunoblotting with antiphosphotyrosine antibody 4G10 (top panel) and anti-RAFTK (bottom panel). NRS was used as a negative control. There was a 200% estimated increase in phosphorylation after PMA treatment.
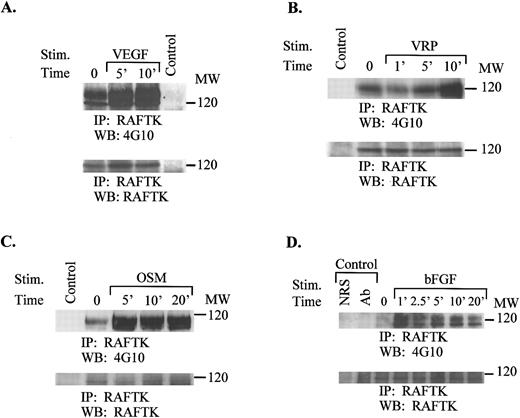
This result prompted us to examine whether treatment of TrHBMEC with cytokines previously reported to modulate endothelial cell growth and function might result in the tyrosine phosphorylation of RAFTK. TrHBMEC were treated with VEGF, VRP, OSM, or bFGF for the time periods shown in Fig 4A through D. Each of these cytokines resulted in the phosphorylation of RAFTK. As seen in Fig 4A through D, the observed changes in RAFTK phosphorylation occurred without altering RAFTK protein levels. As we have observed in other studies, RAFTK was detected as a single or double band depending on the resolution of the gels.
Tyrosine phosphorylation of RAFTK in TrHBMEC after cytokine treatment. Cells were serum-starved overnight and then treated with VEGF (A), VRP (B), OSM (C), or bFGF (D) for the indicated time periods. TCL (1 mg) from treated or untreated cells were immunoprecipitated with anti-RAFTK antibody. Immunoprecipitates were resolved on 7.5% SDS-PAGE and subjected to serial immunoblotting with the antiphosphotyrosine antibody 4G10 (top panel) and anti-RAFTK antibody (bottom panel). NRS was used as a negative control. There was a 200% to 500% estimated increase in phosphorylation after cytokine treatment.
Tyrosine phosphorylation of RAFTK in TrHBMEC after cytokine treatment. Cells were serum-starved overnight and then treated with VEGF (A), VRP (B), OSM (C), or bFGF (D) for the indicated time periods. TCL (1 mg) from treated or untreated cells were immunoprecipitated with anti-RAFTK antibody. Immunoprecipitates were resolved on 7.5% SDS-PAGE and subjected to serial immunoblotting with the antiphosphotyrosine antibody 4G10 (top panel) and anti-RAFTK antibody (bottom panel). NRS was used as a negative control. There was a 200% to 500% estimated increase in phosphorylation after cytokine treatment.
RAFTK activation and its association with the cytoskeletal protein paxillin in TrHBMEC after cytokine treatment.After observing expression of RAFTK in TrHBMEC and its phosphorylation upon various cytokine treatments, we inquired whether the kinase was activated in addition to being phosphorylated. To that end, we performed an in vitro kinase assay as described in the Materials and Methods. The kinase activity of RAFTK moderately increased after cytokine treatment (data not shown).
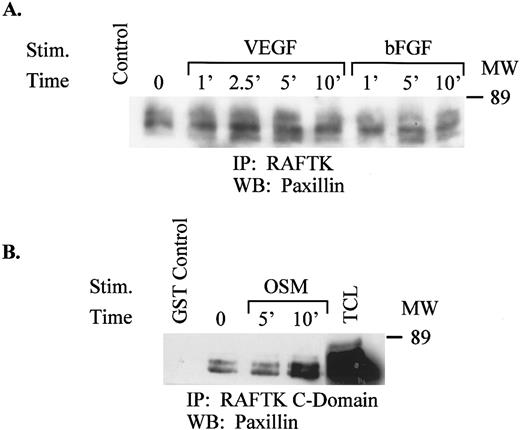
Because RAFTK has previously been reported to coordinate signals between various receptors and cytoskeletal elements such as vinculin or paxillin,21,29 30 we addressed whether this function was also mediated in TrHBMEC. We therefore performed an immunoprecipitation with RAFTK followed by immunoblotting with anti-paxillin antibodies and found an association of these two molecules that was enhanced after treatment with VEGF, bFGF (Fig 5A), or OSM (data not shown). To map the region of RAFTK that associates with paxillin, we immunoprecipitated the lysates with the C-terminal domain of the RAFTK GST-fusion protein and then immunoblotted with anti-paxillin antibodies. As shown in Fig 5B, paxillin did associate with the C-terminus of RAFTK, and this association increased after treatment of endothelial cells with OSM.
(A) Association of RAFTK with paxillin in cytokine-treated TrHBMEC. Similar amounts of TCL from TrHBMEC treated with VEGF or bFGF were immunoprecipitated with the anti-RAFTK antibody. The immunoprecipitates were resolved on 7.5% SDS-PAGE, transferred onto a nitrocellulose membrane, and then immunoblotted with anti-paxillin antibody. NRS was used as a negative control. (B) Association of the GST-fusion protein RAFTK C-terminal domain with paxillin. Unstimulated or stimulated TrHBMEC lysates were immunoprecipitated with the GST-fusion protein RAFTK C-terminal domain, separated on 7.5% SDS-PAGE, transferred onto a nitrocellulose membrane, and immunoblotted with the antipaxillin antibody. GST alone was used as a negative control.
(A) Association of RAFTK with paxillin in cytokine-treated TrHBMEC. Similar amounts of TCL from TrHBMEC treated with VEGF or bFGF were immunoprecipitated with the anti-RAFTK antibody. The immunoprecipitates were resolved on 7.5% SDS-PAGE, transferred onto a nitrocellulose membrane, and then immunoblotted with anti-paxillin antibody. NRS was used as a negative control. (B) Association of the GST-fusion protein RAFTK C-terminal domain with paxillin. Unstimulated or stimulated TrHBMEC lysates were immunoprecipitated with the GST-fusion protein RAFTK C-terminal domain, separated on 7.5% SDS-PAGE, transferred onto a nitrocellulose membrane, and immunoblotted with the antipaxillin antibody. GST alone was used as a negative control.
Activation of the JNK pathway in TrHBMEC after cytokine treatment.JNK is an important member of the mitogen-activated protein kinase (MAPK) family, which acts to facilitate transcriptional activation through elements such as AP-1.23 Recently, RAFTK/Pyk2 has been shown to interact with JNK as a downstream molecule.22 We examined whether cytokine treatment, which activated RAFTK in TrHBMEC, was also able to activate the JNK pathway. As shown in Fig 6, treatment of TrHBMEC with VEGF, VRP, or OSM resulted in the activation of JNK as determined by the phosphorylation of GST-c-Jun (amino acids 1-79).
VEGF, VRP, and OSM activate the JNK kinase in TrHBMEC. Unstimulated or stimulated TrHBMEC lysates were immunoprecipitated with anti-JNK antibody. The immune complex was incubated with kinase buffer containing 5 μCi γ32P-ATP and 0.2 μg/mL GST-c-Jun at RT for 30 minutes. The reaction products were resolved on 12% SDS-PAGE and detected by autoradiography.
VEGF, VRP, and OSM activate the JNK kinase in TrHBMEC. Unstimulated or stimulated TrHBMEC lysates were immunoprecipitated with anti-JNK antibody. The immune complex was incubated with kinase buffer containing 5 μCi γ32P-ATP and 0.2 μg/mL GST-c-Jun at RT for 30 minutes. The reaction products were resolved on 12% SDS-PAGE and detected by autoradiography.
DISCUSSION
Although the bone marrow endothelium has long been recognized to be an important element within the stroma by providing structure as well as growth factors for developing hematopoietic cells, relatively little information is available regarding its signal transduction pathways. We therefore sought to characterize such signaling pathways with particular emphasis on cytokines that have previously been reported to modulate endothelium in terms of cell growth and function.6,9 31
The FLT-4 receptor has recently been identified as a member of the protein kinase family and is known to be expressed in normal proliferating lymphatic endothelium.11 The ligand for the FLT-4 receptor, termed VRP or VEGF-C, was recently discovered.14,15 We examined TrHBMEC for expression of the FLK-1 receptor for VEGF and the FLT-4 receptor for VRP. We found both receptors expressed on these cells and proceeded to characterize some of the signaling pathways induced after treatment with these ligands. We focused on the recently identified RAFTK molecule because of the accruing information on its multifaceted functions in coordinating integrin and cytokine-mediated surface signals with downstream regulators of cell growth.16,17,21,22,28 30
We observed potent phosphorylation and activation of RAFTK after treatment with VEGF or VRP as well as two previously reported cytokines, bFGF and OSM, that stimulate other types of endothelium.9 32-34 This finding then led us to question whether RAFTK interacted with cytoskeletal elements in TrHBMEC after its activation. We observed that RAFTK was associated with paxillin. This association was enhanced by cytokine treatment and appeared to be mediated via the C-terminus of the kinase. These studies suggest that RAFTK may act partly in pathways of endothelial growth and function by transmitting cytokine signals to the cytoskeleton.
Because of the recent observation that RAFTK/Pyk2 can couple with the downstream JNK signaling pathway in PC-12 neuronal cells after its activation by stress signals,22 we studied JNK activation in TrHBMEC after treatment with cytokines. Each of the cytokines examined (VEGF, VRP, OSM, and bFGF ) led to the activation of JNK. JNK activation is known to be a pivotal step in the modulation of several transcriptional mediators, including AP-1, that leads to the expression of several growth-promoting genes.24-26
Taken together, our studies indicate that bone marrow endothelium along with other cells including human megakaryocytes share certain common features in signal transduction pathways induced by cytokines.21 There is considerable literature on the similarities between endothelium and megakaryocytes with regard to receptor expression as well as gene expression.35 The characterization of signal transduction pathways in bone marrow endothelial cells may provide insights into regulating growth and function in these cells.
ACKNOWLEDGMENT
The authors thank our colleagues William C. Hatch and Mel A. Ona for their technical assistance. We are very thankful to Dr Hava Avraham for her helpful discussions. We also thank Dr James Lee and William I. Wood from Genentech, Inc for providing VRP and VEGF. We are grateful to Janet Delahanty for her editing and for the preparation of the figures for this manuscript, as well as Evelyn Gould for her assistance with the figures. We also thank Eun-Young Kim for her assistance with cell culture. Finally, we appreciate Youngsun Jung for her typing assistance and Delroy Heath for facilitating our receipt of the needed reagents for the experiments.
Supported in part by National Institutes of Health Grants No. HL 53745-02, HL 43510-07, HL 55187-01, HL 51456-02, HL 55445-01, and HL 18828.
Address reprint requests to Jerome E. Groopman, MD, Divisions of Experimental Medicine and Hematology/Oncology, Harvard Institutes of Medicine-BIDMC, 4 Blackfan Circle, Boston, MA 02115.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal