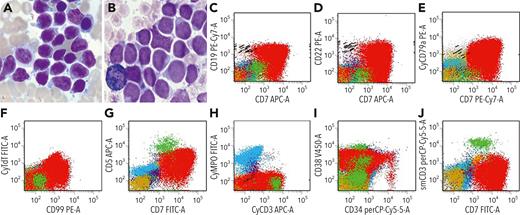
A 43-year-old man presented with erythema. A complete blood cell count showed leukocytosis (16.74 × 109/L), thrombocytopenia, and normal hemoglobin. Bone marrow aspiration showed 86% blasts (panel A; Wright-Giemsa stain, 400× lens objective); cytochemistry showed negative myeloperoxidase (MPO) (panel B; 400× lens objective). Flow cytometry (panels C-J) demonstrated that the blasts (red) were CD7+ (bright)/cytoplasmic CD3+/cytoplasmic terminal deoxynucleotidyltransferase–positive (part)/CD99+ (part bright)/CD5+ (dim)/CD19+ (strong)/cytoplasmic CD79a+/CD22+ (strong)/CD38+, CD34–, and MPO–. Cytogenetic studies revealed a normal karyotype. Next-generation sequencing detected mutations for SETD2 (c.7516–7517insGGGGGTGGGTA [p.Lys2506Argfs∗11], allele frequency [AF]: 38.00%); JAK3 (c.2716C>T [p.Pro906Ser], AF: 38.10%); PHF6 (c.862G>A [p.Ala288Thr], AF: 82.00%). RNA-sequencing detected fusion for NAP1L1::MLLT10 and a new fusion for MLLT10::ASUN. A diagnosis of T/B-cell mixed phenotypic acute leukemia (MPAL) with fusion of MLLT10::ASUN was rendered.
T/B MPAL is a rare disease with a poor prognosis. PHF6 mutations have been identified in T-cell acute lymphoblastic leukemia (ALL), and recently implicated as having an oncogenic effect in B-cell ALL. The high frequency of PHF6 mutation in this case may be the cause of lineage promiscuity, leading to T/B MPAL. NAP1L1::MLLT10 has been identified in T-cell ALL but not in T/B MPAL. The fusion for MLLT10::ASUN has not been reported in hematological diseases. These findings suggest that PHF6 and MLLT10 may play a role in the pathogenesis of this case and the function of MLLT10::ASUN is worth exploring.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal