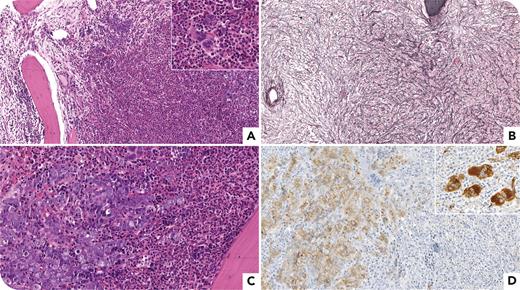
A 76-year-old man presented with leukocytosis (52 × 109/L) and anemia (10.2 g/dL); peripheral blood sample revealed left-shifted granulopoiesis without blasts. Physical examination was unremarkable. Bone marrow (BM) biopsy specimen showed increased cellularity due to granulopoiesis with eosinophils (panel A, hematoxylin and eosin [H&E], 10× objective), and megakaryocytes displayed myeloproliferative neoplasm–like features (panel A [inset], H&E, 40× objective; panel D [inset], factor VIII immunostain, 40× objective); MF-3 fibrosis was also seen (panel B, reticulin, 10× objective). Erythroid precursors were arranged in clusters (panel C, H&E, 20× objective), highlighted by E-cadherin immunostain (panel D, 20× objective). BM aspiration resulted in a dry tap. BCR::ABL1 was negative, whereas JAK2 V617F tested positive with a variant allele frequency (VAF) of 1%. Next-generation sequencing (NGS) analysis demonstrated EZH2 p.D136V (VAF 36%) and ZRSR2 p.K17Sfs∗6 (VAF 78%) mutations. The clinical and molecular picture aroused the suspicion of myelofibrosis, and histological BM features suggested myeloid/lymphoid neoplasm with eosinophilia (M/LN-eo) and JAK2 fusion. An NGS panel addressing M/LN-eo gene fusions showed PCM1::JAK2 rearrangement (in-frame fusion between exon 36 of PCM1 and exon 9 of JAK2). The patient started ruxolitinib but discontinued it after 6 months due to anemia and thrombocytopenia.
To our knowledge, this is the first report of a case with coexistence of PCM1::JAK2 and JAK2 V617F mutation and underlines (1) the clinical heterogeneity of JAK2 rearranged M/LN-eo cases and (2) the central role of BM histopathology in establishing this diagnosis.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal