Key Points
Rivaroxaban is superior to placebo for extended prevention of venous thromboembolism after laparoscopic surgery for colorectal cancer.
Rivaroxaban did not increase bleeding during extended prevention of venous thromboembolism after laparoscopic surgery for colorectal cancer.
Abstract
The clinical benefit of extended prophylaxis for venous thromboembolism (VTE) after laparoscopic surgery for cancer is unclear. The efficacy and safety of direct oral anticoagulants for this indication are unexplored. PROphylaxis of venous thromboembolism after LAParoscopic Surgery for colorectal cancer Study II (PROLAPS II) was a randomized, double-blind, placebo-controlled, investigator-initiated, superiority study aimed at assessing the efficacy and safety of extended prophylaxis with rivaroxaban after laparoscopic surgery for colorectal cancer. Consecutive patients who had laparoscopic surgery for colorectal cancer were randomized to receive rivaroxaban (10 mg once daily) or a placebo to be started at 7 ± 2 days after surgery and given for the subsequent 3 weeks. All patients received antithrombotic prophylaxis with low-molecular-weight heparin from surgery to randomization. The primary study outcome was the composite of symptomatic objectively confirmed VTE, asymptomatic ultrasonography-detected deep vein thrombosis (DVT), or VTE-related death at 28 ± 2 days after surgery. The primary safety outcome was major bleeding. Patient recruitment was prematurely closed due to study drug expiry after the inclusion of 582 of the 646 planned patients. A primary study outcome event occurred in 11 of 282 patients in the placebo group compared with 3 of 287 in the rivaroxaban group (3.9 vs 1.0%; odds ratio, 0.26; 95% confidence interval [CI], 0.07-0.94; log-rank P = .032). Major bleeding occurred in none of the patients in the placebo group and 2 patients in the rivaroxaban group (incidence rate 0.7%; 95% CI, 0-1.0). Oral rivaroxaban was more effective than placebo for extended prevention of VTE after laparoscopic surgery for colorectal cancer without an increase in major bleeding. This trial was registered at www.clinicaltrials.gov as #NCT03055026.
Introduction
The incidence of venous thromboembolism (VTE) after cancer surgery is about twofold higher than that observed after noncancer surgery, with an incidence of a fatal pulmonary embolism that is about threefold higher than that observed after noncancer surgery.1,2 In-hospital heparin prophylaxis reduces deep vein thrombosis (DVT) and fatal pulmonary embolism by about 65% after open cancer surgery.3
In patients who had open major abdominal or pelvic surgery for cancer disease, randomized studies4,5 and several meta-analyses6-9 showed that extension of antithrombotic prophylaxis to 4 weeks after surgery reduces the incidence of venographic DVT and pulmonary embolism compared with a 1-week course. Based on these data, current international guidelines recommend a 4-week course of prophylaxis with low-molecular-weight heparin after open major abdominal or pelvic cancer surgery.10,11
Abdominal and pelvic cancer surgery have substantially changed in the last 2 decades with the introduction of laparoscopic surgery, which improves functional outcomes and reduces postoperative hospitalization with similar death rates compared with open surgery.12-14 In a pilot randomized open-label study, extended prophylaxis with low-molecular-weight heparin reduced ultrasound-detected VTE at 3 months after laparoscopic surgery for colorectal cancer.15 This study led to extended prophylaxis also being recommended after laparoscopic cancer surgery.10,11,16
Direct oral anticoagulants have been shown to be effective and safe for antithrombotic prophylaxis after major orthopedic surgery, but no data are currently available on these agents in cancer surgery. Indeed, an oral agent given at fixed doses to be started at patient discharge could improve the practicality of extended prophylaxis.
The aim of the study was to assess the efficacy and safety of extended (up to day 28 ± 2 after surgery) prophylaxis for VTE with rivaroxaban compared with placebo after planned laparoscopic surgery for colorectal cancer in patients who had received prophylaxis with low-molecular-weight heparin for 7 ± 2 days.17
Methods
Trial design and oversight
The PROphylaxis of venous thromboembolism after LAParoscopic Surgery for colorectal cancer Study II (PROLAPS II) study was a randomized, double-blind, investigator-initiated, superiority trial with blinded central outcome adjudication that compared rivaroxaban with placebo for extended antithrombotic prophylaxis after laparoscopic surgery for colorectal cancer. Rivaroxaban or placebo was started at 7 ± 2 days from surgery and given for the following 3 weeks. All patients received antithrombotic prophylaxis with low molecular-weight heparin from surgery to randomization that occurred at 7 ± 2 days from surgery. The rationale and design of this study were published previously.17
The sponsor of the study was FADOI (Foundation of the Italian Scientific Society of Internal Medicine). The study was endorsed by SICO (Italian Society of Cancer Surgery), was partially supported by an unrestricted grant by Bayer, Italy, and was coordinated by the Clinical Research Unit of the University of Perugia, the Research Center of FADOI Foundation, and the Steering Committee of the study. The members of the Steering Committee were responsible for the design and oversight of the study, development of the protocol, analysis of the data, writing of the manuscript, and the decision to submit the manuscript for publication.
Data were collected and maintained by the Research Center of FADOI Foundation (Milan, Italy) and were analyzed at the University of Perugia under the supervision of the Steering Committee members. Bayer played no role in the design or conduct of the trial, the collection or analysis of the data, or the reviewing or editing of the manuscript. The Steering Committee vouch for the completeness and accuracy of the data and the adherence of the study to the protocol.
The composition of the study committees is reported in the supplemental Appendix (available on the Blood Web site).
The study was performed in accordance with the provisions of the Declaration of Helsinki and local regulations. Protocol and amendments were approved by AIFA (Italian Competent Authority) and the Institutional Review Board or Ethics Committee at each study center. All patients provided written informed consent.
Patients
Patients were eligible for inclusion in the study if they were affected by colorectal cancer (regardless of the stage), scheduled for elective laparoscopic surgery for colorectal cancer, and if they had received antithrombotic prophylaxis with low-molecular-weight heparin for 7 ± 2 days after surgery, according to local practice.
Exclusion criteria were: (1) related to surgery: surgery for noncancer disease, duration of surgery <45 min, conversion to open surgery; (2) related to an increased bleeding risk: known cerebral metastases, known hemorrhagic diseases, or high risk for bleeding, history of intracerebral bleeding or neurosurgery within 6 months; (3) related to specific clinical indications or contraindication to anticoagulant treatment: other indication for anticoagulant therapy, renal insufficiency (creatinine clearance <30 mL/min based on the Cockcroft Gault equation) or liver failure (acute hepatitis, chronic active hepatitis, liver cirrhosis; or an alanine aminotransferase level 3 times or more and/or bilirubin level 2 times or more above the upper limit of the normal range), history of heparin-induced thrombocytopenia; and (4) general criteria: age <18 years, pregnancy or lactation, and refusal of informed consent.
Neoadjuvant chemotherapy up to 3 days before surgery was not an exclusion criterion.
Randomization and study intervention
Study patients were randomized to receive rivaroxaban given orally at the dose of 10 mg once daily or matching placebo, according to the consecutive box number assigned to each study center.
Rivaroxaban or placebo was commenced within 7 ± 2 days as soon as the patient was able to eat and was continued in order to complete a 4-week period of antithrombotic prophylaxis (3 additional weeks from randomization). Prerandomization prophylaxis with low molecular weight heparin was started 12 to 24 hours after surgery and given until randomization, according to local practice.
A complete venous ultrasonography of the lower limbs was scheduled at 28 ± 2 days from surgery.18
Outcome measures
The primary study outcome was the composite of symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-confirmed DVT, or VTE-related death at 28 ± 2 days (4 weeks) after surgery.
The primary safety outcome of the study was major bleeding defined according to the criteria of the International Society of Thrombosis and Haemostasis for studies with anticoagulant agents in surgical patients.19
Secondary efficacy outcomes were symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-confirmed DVT, and major bleeding or death at 28 ± 2 days (4 weeks) from surgery; the composite of symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-confirmed DVT, and major bleeding or death at 90 days after surgery.
Nonmajor bleeding episodes occurring during the treatment period were also reported.
All study outcome events were centrally adjudicated by an independent committee whose members were unaware of study treatment allocation.
Surveillance and follow-up
The study required the following scheduled visits: at enrollment, at randomization (7 ± 2 days after surgery), at 28 ± 2 days (4 weeks), and at 3 months after surgery. Additional visits with clinical examination and diagnostic imaging were performed if new symptoms and/or signs of VTE or bleeding occurred or anytime it was deemed necessary by the investigator.
Statistical analysis
The study hypothesis was that rivaroxaban would have been able to reduce the primary outcome by 60% in comparison with placebo. A 60% reduction in the incidence of VTE was reported in a landmark meta-analysis on the role of extended vs in-hospital–only postoperative prophylaxis after major open abdominal surgery6 and further confirmed in recently updated meta-analyses.8,16 Assuming an incidence of the primary efficacy outcome of 8.0% with placebo, 646 patients (323 per group) were required to have 80% power to show the superiority of rivaroxaban in comparison with placebo (2-sided α, 0.05). The 8% rate was based on rates from previous studies taking into account a potential lower sensitivity of ultrasound in comparison with venography and the presumed lower rate of VTE in laparoscopic in comparison with open surgery.4,5,16
The primary efficacy data set (modified intention-to-treat population) and safety data set consisted of all randomized subjects who received ≥1 dose of the study drug. In case the results of compression ultrasonography at 28 ± 2 days were not available, VTE was considered present or absent according to clinical follow-up data.
The per-protocol population consisted of all randomized patients who completed the study fully compliant with the protocol and without any major deviation. Efficacy analyses based on the per-protocol population were considered supportive.
For the evaluation of the primary efficacy endpoint, the difference between rivaroxaban and placebo with respect to the incidence rate was estimated using Mantel-Haenszel weights and the corresponding asymptotic 2-sided 95% confidence interval (CI) based on the approximation to the normal distribution. Incidence rates of the secondary efficacy endpoints as well as of the primary safety endpoint between treatment groups were evaluated using the same methods as described for the primary efficacy evaluation.
A prespecified comparison was planned to compare rates of symptomatic venous thromboembolic events.
All data were analyzed with SPSS version 26.
Results
Patients and treatments
From May 2017 through June 2021, a total of 641 patients were included in the study, and 582 were randomized at 18 centers in Italy and 1 center in Switzerland (Figure 1). Patient recruitment was prematurely closed due to study drug expiry after the inclusion of 582 of the 646 planned patients. More specifically, the study had to be closed because the supply of the study drug reached the expiry date, and it was not possible to resupply. The main reasons for nonrandomization were a decline of consent (18 patients), intraoperative conversion to open surgery (13 patients), and early postoperative complications (7 patients). Demographic and clinical characteristics of randomized and not randomized patients are reported in supplemental Table 1. The modified intention-to-treat analysis included 569 patients. Demographic and clinical characteristics of patients included and excluded from the modified intention-to-treat analysis are reported in supplemental Table 2.
The characteristics of the patients included in the modified intention-to-treat analysis were similar in the 2 treatment groups (Table 1). Overall, 160 (28.1%) patients underwent surgery for rectal cancer, of whom 84 were randomized to placebo and 76 to rivaroxaban. The median time from surgery to randomization was 6.9 days in both the rivaroxaban and the placebo group. The mean duration from randomization to primary outcome assessment was 24 days (standard deviation, 6.8 days) in the rivaroxaban group and 23 days (standard deviation, 5.8 days) in the placebo group (P = .41). Reasons for study treatment discontinuation are provided in supplemental Table 3. Ultrasound examination was performed at 28 ± 2 days after surgery in 541 patients (273 in the rivaroxaban arm and 268 in the placebo arm).
| Characteristic . | Rivaroxaban (n = 287) . | Placebo (n = 282) . |
|---|---|---|
| Age (y), mean (SD) | 65.8 (11.3) | 64.5 (11.1) |
| Male sex, n (%) | 163 (56.8) | 141 (50.0) |
| Comorbidities, n (%) | ||
| Systemic arterial hypertension | 89 (31.0) | 87 (30.9) |
| Diabetes | 33 (11.5) | 27 (9.6) |
| Ischemic heart disease and/or chronic heart failure | 11 (3.8) | 12 (4.3) |
| COPD | 10 (3.5) | 6 (2.1) |
| Previous cancer | 6 (2.1) | 5 (1.8) |
| Liver disease# | 3 (1.0) | 5 (1.8) |
| Laboratory examination at randomization, mean (SD) | ||
| Hemoglobin (mg/dl), mean (SD) | 11.9 (1.6) | 11.5 (1.6) |
| Creatinine (mg/dl), mean (SD) | 0.83 (0.23) | 0.81 (0.21) |
| Neoadjuvant chemotherapy, n (%) | 50 (17.4) | 44 (15.6) |
| Neoadjuvant radiotherapy,‡ n (%) | 48 (16.7) | 46 (16.3) |
| Staging T, n (%) | ||
| T1 | 59 (20.5) | 51 (18.1) |
| T2 | 66 (23.0) | 63 (22.3) |
| T3 | 119 (41.5) | 124 (44.0) |
| T4 | 18 (6.3) | 13 (4.6) |
| TX | 25 (8.7) | 31 (11.0) |
| Staging N, n (%) | ||
| N0 | 201 (70.0) | 203 (72.0) |
| N1 | 62 (21.6) | 47 (16.7) |
| N2 | 24 (8.4) | 25 (8.8) |
| NX | — | 7 (2.5) |
| Staging M, n (%) | ||
| M0 | 284 (98.9) | 274 (97.1) |
| M1 | 3 (1.0) | 8 (2.8) |
| Type of surgery, n (%) | ||
| Right hemicolectomy | 89 (31.0) | 85 (30.1) |
| Left hemicolectomy | 81 (28.2) | 64 (22.7) |
| Rectal anterior resection | 81 (28.2) | 86 (30.5) |
| Rectal anterior resection plus Miles | 8 (2.8) | 10 (3.5) |
| Other | 28 (9.7) | 37 (13.1) |
| Duration of surgery (h), mean (SD) | 3.1 (1.3) | 3.1 (1.3) |
| Initial prophylaxis,§n (%) | ||
| Enoxaparin | 188 (65.5) | 189 (67.0) |
| Nadroparin | 77 (26.8) | 76 (26.9) |
| Other | 22 (7.7) | 17 (6.0) |
| Mechanical prophylaxis‖,¶ | 136 (47.4) | 132 (46.8) |
| Adjuvant therapy, n (%) | 52 (18.1) | 52 (18.4) |
| Characteristic . | Rivaroxaban (n = 287) . | Placebo (n = 282) . |
|---|---|---|
| Age (y), mean (SD) | 65.8 (11.3) | 64.5 (11.1) |
| Male sex, n (%) | 163 (56.8) | 141 (50.0) |
| Comorbidities, n (%) | ||
| Systemic arterial hypertension | 89 (31.0) | 87 (30.9) |
| Diabetes | 33 (11.5) | 27 (9.6) |
| Ischemic heart disease and/or chronic heart failure | 11 (3.8) | 12 (4.3) |
| COPD | 10 (3.5) | 6 (2.1) |
| Previous cancer | 6 (2.1) | 5 (1.8) |
| Liver disease# | 3 (1.0) | 5 (1.8) |
| Laboratory examination at randomization, mean (SD) | ||
| Hemoglobin (mg/dl), mean (SD) | 11.9 (1.6) | 11.5 (1.6) |
| Creatinine (mg/dl), mean (SD) | 0.83 (0.23) | 0.81 (0.21) |
| Neoadjuvant chemotherapy, n (%) | 50 (17.4) | 44 (15.6) |
| Neoadjuvant radiotherapy,‡ n (%) | 48 (16.7) | 46 (16.3) |
| Staging T, n (%) | ||
| T1 | 59 (20.5) | 51 (18.1) |
| T2 | 66 (23.0) | 63 (22.3) |
| T3 | 119 (41.5) | 124 (44.0) |
| T4 | 18 (6.3) | 13 (4.6) |
| TX | 25 (8.7) | 31 (11.0) |
| Staging N, n (%) | ||
| N0 | 201 (70.0) | 203 (72.0) |
| N1 | 62 (21.6) | 47 (16.7) |
| N2 | 24 (8.4) | 25 (8.8) |
| NX | — | 7 (2.5) |
| Staging M, n (%) | ||
| M0 | 284 (98.9) | 274 (97.1) |
| M1 | 3 (1.0) | 8 (2.8) |
| Type of surgery, n (%) | ||
| Right hemicolectomy | 89 (31.0) | 85 (30.1) |
| Left hemicolectomy | 81 (28.2) | 64 (22.7) |
| Rectal anterior resection | 81 (28.2) | 86 (30.5) |
| Rectal anterior resection plus Miles | 8 (2.8) | 10 (3.5) |
| Other | 28 (9.7) | 37 (13.1) |
| Duration of surgery (h), mean (SD) | 3.1 (1.3) | 3.1 (1.3) |
| Initial prophylaxis,§n (%) | ||
| Enoxaparin | 188 (65.5) | 189 (67.0) |
| Nadroparin | 77 (26.8) | 76 (26.9) |
| Other | 22 (7.7) | 17 (6.0) |
| Mechanical prophylaxis‖,¶ | 136 (47.4) | 132 (46.8) |
| Adjuvant therapy, n (%) | 52 (18.1) | 52 (18.4) |
COPD, chronic obstructive pulmonary disease; SD, standard deviation.
The table reports on patients included in the modified intention-to-treat analysis.
Plus–minus values are means ± SD. None of the numerical differences between the 2 groups was statistically significant at an α level of 0.05.
47 rivaroxaban patients and 42 placebo patients received combined neoadjuvant chemo and radiotherapy.
Prophylaxis was started on the evening of surgery in the majority of the patients.
Graduated compression stockings or intermittent pneumatic compression.
One rivaroxaban patient received both graduated compression stockings and intermittent pneumatic compression; 2 placebo patients received both graduated compression stockings and intermittent pneumatic compression.
Liver disease was known hepatitis infection in 5 patients, alcoholic disease in 1, primary biliary cirrhosis in 1, and other diseases in 1.
Primary efficacy and safety outcomes
The primary outcome at 28 ± 2 days from laparoscopic surgery occurred in 3 of the 287 patients (1.0%) in the rivaroxaban group and in 11 of the 282 patients (3.9%) in the placebo group (risk difference, −0.029; 95% CI, −0.054 to −0.003; P = .028; log-rank P = .032) (Table 2). None of these event was a pulmonary embolism.
Clinical outcomes in the modified intention to treat population in patients randomized to rivaroxaban or placebo
| Outcome . | Rivaroxaban (n = 287) . | Placebo (n = 282) . | Risk difference* (95% CI) . | P value . | Hazard ratio (95% CI) . | P value† . |
|---|---|---|---|---|---|---|
| Primary efficacy outcome | ||||||
| Symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-confirmed DVT or VTE-related death at 28 ± 2 d from laparoscopic surgery for colorectal cancer, n (%) | 3 (1.0) | 11 (3.9) | −0.029 (−0.054 to −0.003) | .028 | 0.27 (0.07-0.96) | .032 |
| Symptomatic VTE, n (%) | 1 (0.3) | 4 (1.4) | — | — | — | — |
| Asymptomatic ultrasonography-detected VTE | 2 (0.7) | 7 (2.5) | — | — | — | — |
| Proximal DVT, n (%)‡ | 0 | 4 (1.4) | — | — | — | — |
| PE or VTE-related deaths, n (%) | 0 | 0 | — | — | — | — |
| Primary safety outcome | ||||||
| Major bleeding, n (%)§ | 2 (0.7) | 0 | — | — | — | — |
| Secondary outcomes | ||||||
| Symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-confirmed DVT, major bleeding or death at 28 ± 2 d from surgery, n (%) | 5 (1.7) | 11 (3.9) | −0.022 (−0.049 to 0.006) | .120 | 0.44 (0.15-1.27) | .129 |
| Symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-confirmed DVT, major bleeding or death at 90 ± 2 d from surgery, n (%) | 6 (2.1) | 12 (4.2) | −0.022 (−0.050 to 0.007) | .141 | 0.49 (0.18-1.31) | .143 |
| Clinically relevant exploratory outcomes | ||||||
| Nonmajor bleedings,‖ n (%) | 3 (1.0) | 5 (1.8) | — | — | — | — |
| Death from any cause at 90 d,¶ n (%) | 0 | 1 (0.3) | — | — | — | — |
| Outcome . | Rivaroxaban (n = 287) . | Placebo (n = 282) . | Risk difference* (95% CI) . | P value . | Hazard ratio (95% CI) . | P value† . |
|---|---|---|---|---|---|---|
| Primary efficacy outcome | ||||||
| Symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-confirmed DVT or VTE-related death at 28 ± 2 d from laparoscopic surgery for colorectal cancer, n (%) | 3 (1.0) | 11 (3.9) | −0.029 (−0.054 to −0.003) | .028 | 0.27 (0.07-0.96) | .032 |
| Symptomatic VTE, n (%) | 1 (0.3) | 4 (1.4) | — | — | — | — |
| Asymptomatic ultrasonography-detected VTE | 2 (0.7) | 7 (2.5) | — | — | — | — |
| Proximal DVT, n (%)‡ | 0 | 4 (1.4) | — | — | — | — |
| PE or VTE-related deaths, n (%) | 0 | 0 | — | — | — | — |
| Primary safety outcome | ||||||
| Major bleeding, n (%)§ | 2 (0.7) | 0 | — | — | — | — |
| Secondary outcomes | ||||||
| Symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-confirmed DVT, major bleeding or death at 28 ± 2 d from surgery, n (%) | 5 (1.7) | 11 (3.9) | −0.022 (−0.049 to 0.006) | .120 | 0.44 (0.15-1.27) | .129 |
| Symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-confirmed DVT, major bleeding or death at 90 ± 2 d from surgery, n (%) | 6 (2.1) | 12 (4.2) | −0.022 (−0.050 to 0.007) | .141 | 0.49 (0.18-1.31) | .143 |
| Clinically relevant exploratory outcomes | ||||||
| Nonmajor bleedings,‖ n (%) | 3 (1.0) | 5 (1.8) | — | — | — | — |
| Death from any cause at 90 d,¶ n (%) | 0 | 1 (0.3) | — | — | — | — |
According to the Mantel-Haenszel method.
Log-rank P value.
Proximal DVT was symptomatic in 2 placebo patients.
Both major bleedings were dehiscence of surgical anastomosis occurring during study treatment: the first occurring at 11 d from randomization (17 d from transanal total mesorectal excision); the second occurring at 12 d from randomization (19 from right hemicolectomy).
Four were clinically relevant nonmajor bleeding, 2 in patients randomized to placebo and 2 in patients randomized to rivaroxaban.
One additional placebo patient died 108 d after surgery due to cancer progression.
Major bleeding occurred in 2 patients (0.7%) in the rivaroxaban group and no patients in the placebo group. In both patients, major bleeding occurred at the surgical site, was associated with a reduction in hemoglobin >20 g per liter, and led to reintervention. No fatal bleeding occurred.
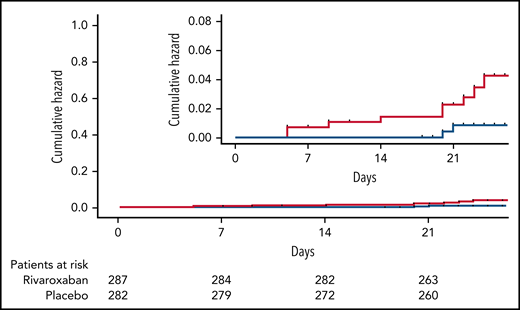
The time to primary study outcome events at 28 ± 2 days by treatment groups is shown in Figure 2.
Time from randomization to primary study outcome event in patients randomized to receive rivaroxaban (blue line) or placebo (red line).
Time from randomization to primary study outcome event in patients randomized to receive rivaroxaban (blue line) or placebo (red line).
After the exclusion of 26 patients with major violations, 13 in each treatment group, 543 patients were included in the per-protocol analysis (Figure 1). A primary study outcome event occurred in 1.2% and 4.1% of the patients randomized to rivaroxaban or placebo, respectively (risk difference, −0.030; 95% CI, −0.057 to −0.003; P = .028). Results of the analyses in the per-protocol population are shown in supplemental Table 4.
Secondary outcomes
The combined incidence of symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-detected DVT, and major bleeding or death within 28 ± 2 days after laparoscopic surgery was 1.7% in rivaroxaban patients and 3.9% in placebo patients (risk difference, −0.022; 95% CI, −0.049 to 0.006; P = .120) (Table 2).
Symptomatic objectively-confirmed VTE, asymptomatic ultrasonography-detected DVT, and/or major bleeding and/or death within 90 days from surgery occurred in 6 rivaroxaban patients and in 12 placebo patients (2.1 vs 4.2%; risk difference, −0.022; 95% CI, −0.050 to 0.007; P = .141) (Table 2). No pulmonary embolism occurred during the 90-day follow-up. The time to study outcome events at 90 ± 2 days by treatment groups is shown in supplemental Figure 1.
Nonmajor bleedings were reported in 3 patients randomized to rivaroxaban and 5 randomized to placebo during the study treatment period (from randomization to 28 ± 2 days from laparoscopic surgery). One of these events was a clinically relevant nonmajor rectorrhagia leading to study treatment discontinuation in a patient randomized to placebo.
Both symptomatic DVT and proximal DVT were numerically more common in patients randomized to receive a placebo in comparison with rivaroxaban.
Death occurred in 1 patient at 76 days from randomization in a patient randomized to placebo and was deemed to be because of cancer progression.
One placebo patient had central venous line-related symptomatic DVT of the upper limb at 80 days from surgery. This event did not qualify as a study outcome event as it occurred at the upper limb.
Discussion
Our study shows that extended prophylaxis with rivaroxaban reduces the incidence of postoperative VTE in comparison with placebo after laparoscopic surgery for colorectal cancer without a significant increase in the risk of major bleeding.
In the absence of thromboprophylaxis, the incidence of venography-detected VTE following open abdominal surgery has been reported to vary between 19% to 29% in high‐risk patients and to remain elevated for 4 to 6 weeks.5,13 Specific figures on postdischarge VTE after cancer surgery are limited to a small number of randomized studies. In a landmark randomized study in 332 patients, 4-week prophylaxis with the low-molecular-weight heparin enoxaparin significantly reduced the incidence of symptomatic or venography-detected VTE at 28 days compared with 1-week prophylaxis.4 Several meta-analyses confirmed the clinical benefit of extending antithrombotic prophylaxis to 4 weeks after major open abdominal surgery.6-8 Extended antithrombotic prophylaxis up to 4 weeks postoperatively is recommended after open cancer surgery based on the results of these randomized studies and meta-analyses.4,5,8,9
In recent years, surgery for cancer was shifted from open to laparoscopic procedures because of the evidence for improved functional outcomes with similar mortality rates compared with open surgery.12-14,20 The laparoscopic technique also allowed the implementation of enhanced recovery after surgery programs with the aim of improving clinical outcomes and quality of care and reducing the time to initiation and completion of adjuvant chemotherapy after surgery and the cost of hospitalization.21-24 A meta-analysis including 12 randomized trials comparing short-term outcomes after laparoscopic or open resection for colorectal cancer showed a similar incidence of symptomatic DVT in the 2 groups (odds ratio, 0.81; 95% CI, 0.25-2.61).25 No pulmonary embolism was reported.
The optimal regimen and duration of antithrombotic prophylaxis in patients undergoing laparoscopic surgery is unknown. In a pilot study, 225 patients who underwent laparoscopic surgery for colorectal cancer were randomly assigned to 1- or 4-week thromboprophylaxis with low molecular weight heparin.15 By 4 weeks after surgery, VTE had occurred in 9.7% of patients in the 1-week and no patients in the 4-week arm. This study was integrated into an updated meta-analysis used to inform international guidelines.26 Based on this updated evidence, current international guidelines recommend extended antithrombotic prophylaxis after laparoscopic cancer surgery as a conditional recommendation and very low certainty in the evidence of effect.10,11 The present study, the PROLAPS II study, showed the efficacy of extended 4-week vs 7-day antithrombotic prophylaxis for the prevention of VTE after laparoscopic surgery for cancer.
Direct oral anticoagulants were compared with low-molecular-weight heparin in the prevention of VTE after major orthopedic surgery, but no clinical trial has assessed the efficacy and safety of these agents in nonorthopedic surgery. The availability of an oral agent for postdischarge prophylaxis may improve the practicality of prophylaxis and patient adherence. In fact, parenteral administration may be associated with reduced adherence after hospital discharge.
In our study, rivaroxaban reduced the risk for VTE by >70% compared with placebo, with a number needed to treat 34 patients for the primary study outcome; the number needed to treat to prevent 1 symptomatic VTE was 91. The magnitude of the observed risk reduction with rivaroxaban is of the same order of magnitude as that reported with low-molecular-weight heparin for extended prophylaxis in laparoscopic15 and open surgery.26
Bleeding complications are the main tradeoff for the efficacy of antithrombotic prophylaxis. In our study, rivaroxaban given orally at a prophylactic regimen was associated with a 0.7% risk for major bleeding, similar to the 1% reported in the setting of cancer surgery with low-molecular-weight heparin26 and orthopedic surgery in patients receiving rivaroxaban.27 Both major bleedings occurred at the site of surgery and led to reintervention. The number needed to harm in the PROLAPS II study is 143 patients. These results can reassure clinicians regarding the safety of rivaroxaban for extended prophylaxis after laparoscopic surgery for cancer.
The primary study outcome for this study was a composite of symptomatic objectively-confirmed VTEs and asymptomatic, ultrasound-detected DVT. The use of surrogate endpoints (asymptomatic, screen-detected events) is common in placebo-controlled studies in the primary prevention of VTE. This approach is aimed at identifying any significant DVT that may be missed clinically, with the opportunity of early diagnosis and reduction in major potentially life-threatening VTEs. In addition, by increasing event rates, this approach allows for reduction of patient exposure to placebo and to fasten efficacy assessment of antithrombotic agents.
The rate of VTE, the primary study outcome, was lower than anticipated. The low rate of VTE overall, the low rate of VTE in placebo patients, the nonsuperiority in the combined analysis (VTE and bleeding), and the absence of pulmonary embolism and VTE-related deaths could question the need for thromboprophylaxis in these patients. As a possible explanation, both the improvements in laparoscopic technique20 and the use of ultrasonography-detected endpoint may have influenced this event rate. Reduced surgery invasiveness and tissue damage, as well as shorter hospital stay after laparoscopic compared with open surgery, may have led to a lower rate of VTE. Ultrasonography may have missed some DVT of the lower limbs at 28 days from surgery. In the past, studies in the prevention of postoperative VTE had a venography-assessed outcome. However, about 20% of the patients in these studies did not undergo venography, or this was inadequate for outcome assessment. Of note, rates of symptomatic events in our study (1.4% in the placebo group) are consistent with those reported in previous studies.15,25 Furthermore, <10% of the patients in the PROLAPS II study had locally advanced or metastatic disease. It is conceivable that the inclusion of patients with nonmetastatic disease translated into a low incidence of thromboembolic complications. Should our results regarding the low rate of thromboembolic complications be confirmed in other studies, the need for extended antithrombotic prophylaxis in this specific setting could be revised.
Our study has some limitations. The study recruitment was slower than anticipated, also due to the COVID-19 pandemic. Thus, the study drug expired when about 90% of patients had been randomized in the study, and it was not possible to replace it. Prerandomization antithrombotic prophylaxis was not standardized as it was left to the discretion of the investigators according to local practice. This was also the case for mechanical prophylaxis. Time from randomization to primary outcome assessment was longer than expected, and this was partially due to limited accessibility to study centers during the COVID-19 pandemia.
Our study also has some strengths, including the double-blind design that prevents the suspicion bias, the control arm with placebo, and the adjudication of study outcome events by an adjudication committee unaware of study treatment allocation. The proportion of patients with major protocol violations that required exclusion from the per-protocol analysis was low.
Conclusions
Rivaroxaban was more effective than placebo for the extended prevention of VTE after laparoscopic surgery for colorectal cancer without an increased risk of major bleeding. The oral administration of rivaroxaban provides the opportunity to make extended prophylaxis easier after laparoscopic surgery in cancer patients.
Acknowledgments
The authors acknowledge Bayer, Italy for their support. Bayer, Italy had no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data, preparation, review, or approval of the manuscript, and decision to submit the manuscript for publication.
The authors thank all investigators and patients for their trust and support.
The study was partially supported by an unrestricted grant by Bayer, Italy.
Authorship
Contribution: C.B. contributed to the conception and design of the study, acquisition, analysis, and interpretation of data, drafting and revising the paper critically for important intellectual content, final approval of the version to be published, and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; G.A. contributed to the conception and design of the study, interpretation of data, revising the paper critically for important intellectual content, and final approval of the version to be published; S.F. and G.G. contributed to the acquisition and interpretation of data, revising the paper critically for important intellectual content, final approval of the version to be published, and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; F.R. and P.D. contributed to the conception of the study, acquisition and interpretation of data, revising the paper critically for important intellectual content, and final approval of the version to be published; U.P., F.P., A.D., G.A., M.B., D.C., M.D.P., A.V., R.D.L., F.G., A.M., G.P., M.M., G.C., M.R., J.M., M.C.V., and R.P. contributed in acquisition and interpretation of data, revising the paper critically for important intellectual content, and final approval of the version to be published; and M.C. and F.D. contributed in revising the paper critically for important intellectual content and final approval of the version to be published.
Conflict-of-interest disclosure: C.B. received speaker and advisor fees from Daiichi Sankyo, Bayer, Pfizer, and Bristol-Myers Squibb, all outside the present study. F.D. received speaker and advisor fees from Daiichi Sankyo, Bayer, Pfizer, Bristol-Myers Squibb, Boehringer, Sanofi, Alfa Sigma, and Novartis, all outside the present study. G.A. received personal fees from Pfizer, Bayer Healthcare, and Daichi Sankyo, all outside the present study. The remaining authors declare no competing financial interests.
Correspondence: Cecilia Becattini, Internal and Cardiovascular Medicine and Stroke Unit, University of Perugia, Piazzale Menghini 1, 06129 Perugia, Italy; e-mail: cecilia.becattini@unipg.it.
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.



Comments
PROLAPS-II: risks of oral anticoagulation in extended thromboprophylaxis after colorectal surgery
Most events were asymptomatic screen-detected VTE (0.7% vs 2.5%), a surrogate endpoint without proven clinical significance.2 There was no difference in symptomatic VTE (0.3% vs 1.4%) and no pulmonary embolisms. Although unreported, failure to salvage would be a more relevant endpoint since many symptomatic VTE can be effectively treated.2 In summary, 99% of patients in the placebo group did not experience a symptomatic VTE, and there is no evidence that the few who did were unable to be salvaged.
More concerning is a potential signal for harm. Five patients in the rivaroxaban group required re-intervention compared with 1 in the placebo group, an outcome approaching statistical significance (Table S3). Of note, the PROLAPS-II study was not powered to detect rare surgical complications. Two re-interventions were for major bleeding and anastomotic dehiscence with suspiciously delayed timing: 17 days after transanal total mesorectal excision, and 19 days after right hemicolectomy.3 The hypothesis that these complications were caused by rivaroxaban is consistent with data showing its association with higher GI bleeding events versus other direct oral anticoagulants.4
While the PROLAPS-II study is an important contribution, it should give clinicians pause regarding the safety of rivaroxaban for extended prophylaxis, especially considering that current recommendations for extended thromboprophylaxis are based on low levels of evidence.5 Larger studies with omission of unproven surrogate endpoints and thorough reporting of clinical outcomes are needed before extended thromboprophylaxis with oral anticoagulation should be recommended.
References
1. Becattini C, Pace U, Pirozzi F, et al. Rivaroxaban versus placebo for extended antithrombotic prophylaxis after laparoscopic surgery for colorectal cancer. Blood. 2022;
2. Klemen ND, Feingold PL, Hashimoto B. How Strong Is the Evidence Supporting Thromboprophylaxis in Surgical Oncology? J Clin Oncol. 2021;
3. Li Y-W, Lian P, Huang B, et al. Very Early Colorectal Anastomotic Leakage within 5 Post-operative Days: a More Severe Subtype Needs Relaparatomy. Sci Rep-uk. 2017;7(1):39936.
4. Ingason AB, Hreinsson JP, Ágústsson AS, et al. Rivaroxaban Is Associated With Higher Rates of Gastrointestinal Bleeding Than Other Direct Oral Anticoagulants: A Nationwide Propensity Score–Weighted Study. Ann Intern Med. 2021;174(11):1493–1502.
5. Lyman GH, Carrier M, Ay C, et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood advances. 2021;5(4):927–974.