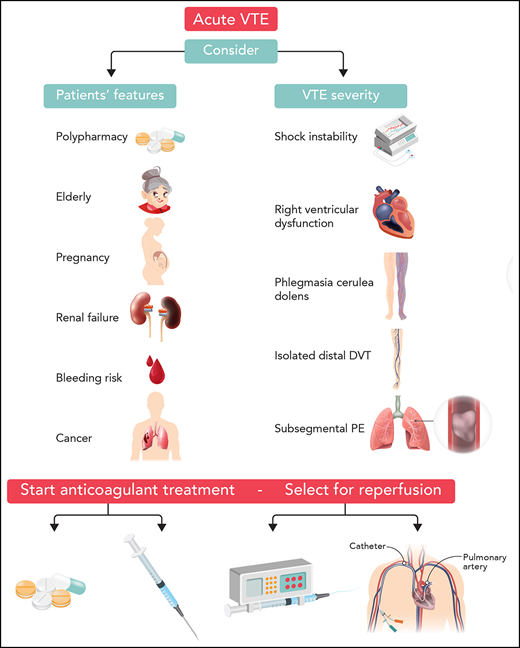
Visual Abstract
Professional illustration by Somersault18:24.
Abstract
All patients with venous thromboembolism (VTE) should receive anticoagulant treatment in the absence of absolute contraindications. Initial anticoagulant treatment is crucial for reducing mortality, preventing early recurrences, and improving long-term outcome. Treatment and patient disposition should be tailored to the severity of clinical presentation, to comorbidities, and to the potential to receive appropriate care in the outpatient setting. Direct oral anticoagulants (DOACs) used in fixed doses without laboratory monitoring are the agents of choice for the treatment of acute VTE in the majority of patients. In comparison with conventional anticoagulation (parenteral anticoagulants followed by vitamin K antagonists), these agents showed improved safety (relative risk [RR] of major bleeding, 0.61; 95% confidence interval [CI], 0.45-0.83) with a similar risk of recurrence (RR, 0.90; 95% CI, 0.77-1.06). Vitamin K antagonists or low molecular weight heparins are still alternatives to DOACs for the treatment of VTE in specific patient categories such as those with severe renal failure or antiphospholipid syndrome, or cancer, respectively. In addition to therapeutic anticoagulation, probably less than 10% of patients require reperfusion by thrombolysis or interventional treatments; those patients are hemodynamically unstable with acute pulmonary embolism, and a minority of them have proximal limb-threatening deep vein thrombosis (DVT). The choice of treatment should be driven by the combination of evidence from clinical trials and by local expertise. The majority of patients with acute DVT and a proportion of selected hemodynamically stable patients with acute pulmonary embolism can be safely managed as outpatients.
Introduction
Venous thromboembolism (VTE) is a common disease with an average annual age- and sex-adjusted incidence of 123 per 100 000 person-years in the United States.1 According to recent estimates, the incidence of VTE is 131 per 100 000 person-years in Europe.2 The clinical manifestation of VTE is deep vein thrombosis (DVT) in the majority of the patients; pulmonary embolism (PE) with or without concomitant DVT accounts for 30% to 40% of the cases.3 The incidence of PE seems to have increased in recent years,4 probably because of a heightened awareness of the disease, around-the-clock availability of computed tomography (CT) angiography, and greater sensitivity of imaging techniques.5
When left untreated, VTE was associated with early recurrences (29%) and death (26%) in landmark studies.6,7 On the basis of this evidence, early anticoagulant treatment should be started in patients with suspected VTE who are estimated to not be at high risk for bleeding while they wait for diagnostic confirmation.8,9 Treatment for VTE is usually divided into 3 phases: initial or acute (5 to 7 days), long term (up to 3 months), and extended (beyond the initial 3 months). This review will focus on treatment during the initial or acute phase. In this phase, the aims of treatment are to reduce mortality and early recurrence or proximal extension of DVT and to relieve symptoms. Thus, treatment of VTE should be tailored to the estimated risk for death or serious adverse events (AEs).8,10,11
DVT and PE: stratification for adverse outcomes in the acute phase
The clinical course of acute VTE is strictly dependent on its manifestation as DVT or PE. In a nationwide cohort study in Denmark, the 30-day mortality rate was 3% for patients with DVT and 31% for patients with PE.12 According to administrative data from the United States, during the 8-year period between 1998 and 2005, the in-hospital fatality rates in patients with PE decreased but remained as high as 8.2%.13 The decrease in 30-day and in-hospital mortality is probably related to increased awareness of evidence-based management strategies, improvements in antithrombotic therapies, and increased diagnosis of segmental and subsegmental PEs.14,15 In fact, the latest generation of CT scanners can diagnose PEs that are associated with a lower risk for death compared with more proximal PEs.16
Among patients with acute PEs, about 10% to 15% will present with shock or hemodynamic instability at the initial clinical evaluation.17,18 Mortality in these patients may be as high as 50% in the first days after diagnosis, the cause of death being acute decompensated heart failure with or without right ventricle infarction. Conversely, about 30% of the patients with acute PEs are asymptomatic or have mild symptoms and low prevalence of comorbidities at diagnosis. These patients may be identified by simple clinical models and have an expected 30-day mortality as low as 1%.19,20 The majority of patients with PE (about 60%) are between the 2 previous categories and may have various degrees of respiratory failure, impending hemodynamic compromise, evidence of right ventricle dysfunction at echocardiography or CT angiography, and/or increased troponin.21 Short-term mortality in these patients may vary between 3% and 12%.20-22 Patients who are in different categories for risk for death may benefit from different management strategies (Figure 1).8,10,11
Patient management based on risk of death or VTE-related complications at presentation. (°) If available and feasible, extracorporeal membrane oxygenation (ECMO) can be used to support hemodynamics in patients with cardiac arrest. In this case, percutaneous or surgical embolectomy should be preferred over systemic thrombolysis to avoid bleeding. In patients not managed by ECMO, systemic thrombolysis offers the opportunity for rapid reperfusion. (§) catheter-directed therapy to be considered for patients with contraindications for or failure of systemic thrombolysis. (*) Clinical risk assessed by validated models (Pulmonary Embolism Severity Index [PESI], simplified PESI) or based on the combination of vital status and comorbidities. (**) Heparin lead-in stands for initial 5 to 9 days of heparin treatment. (°°) Right ventricle dysfunction (RVD) assessed at echocardiography or computed tomography. (^) Early discharge is defined as occurring within 48 hours from admission. (^^) Treatment should be considered in patients with cancer who have symptoms or are at high risk for VTE. DOAC, direct oral anticoagulant; LMWH, low molecular weight heparin; UFH, unfractionated heparin; iv, intravenous.
Patient management based on risk of death or VTE-related complications at presentation. (°) If available and feasible, extracorporeal membrane oxygenation (ECMO) can be used to support hemodynamics in patients with cardiac arrest. In this case, percutaneous or surgical embolectomy should be preferred over systemic thrombolysis to avoid bleeding. In patients not managed by ECMO, systemic thrombolysis offers the opportunity for rapid reperfusion. (§) catheter-directed therapy to be considered for patients with contraindications for or failure of systemic thrombolysis. (*) Clinical risk assessed by validated models (Pulmonary Embolism Severity Index [PESI], simplified PESI) or based on the combination of vital status and comorbidities. (**) Heparin lead-in stands for initial 5 to 9 days of heparin treatment. (°°) Right ventricle dysfunction (RVD) assessed at echocardiography or computed tomography. (^) Early discharge is defined as occurring within 48 hours from admission. (^^) Treatment should be considered in patients with cancer who have symptoms or are at high risk for VTE. DOAC, direct oral anticoagulant; LMWH, low molecular weight heparin; UFH, unfractionated heparin; iv, intravenous.
In patients with acute DVT, thrombosis extension, embolization to the lung, or persistence of symptoms are the most common early adverse events. A minority of DVT patients will present with signs of limb-threatening disease such as cold and pulseless extremities, likely related to venous obstruction, that may evolve into venous gangrene. These events seem to be more common in patients treated for iliofemoral DVT compared with those treated for popliteal or isolated distal DVTs.23-26
Initial anticoagulation
All patients with acute PE or proximal DVT should receive anticoagulant treatment.8,10,11 Pivotal studies showed that failure to rapidly receive therapeutic anticoagulation27,28 and time spent while receiving subtherapeutic anticoagulation are both associated with recurrent VTEs.29 Thus, the availability of anticoagulants with rapid onset of action and predictable dose-effect response are essential for reducing early AEs. A meta-analysis of randomized studies showed that weight-adjusted low molecular weight heparin (LMWH) reduces the risk of recurrent VTEs in either the initial treatment period (odds ratio [OR], 0.69; 95% confidence interval [CI], 0.49-0.98) or at 3 months (OR, 0.71; 95% CI, 0.56-0.90) in comparison with unfractionated heparin.30 The predictable pharmacokinetics of LMWH could explain these results.
Direct oral anticoagulants (DOACs) have a good pharmacodynamic profile and a favorable dose-response curve, although they are not evaluable with standard coagulation tests.31 These agents were developed according to 2 different regimens for the treatment of VTE (Table 1).32-37 The single-drug approach consists of an initial treatment period with high-dose DOACs followed by a maintenance dose of the same agent with no need for parenteral anticoagulation. The sequential approach includes an initial treatment with LWMH or fondaparinux for 5 to 10 days followed by a maintenance dose of DOACs. Apixaban and rivaroxaban have been developed according to the single-drug approach, and dabigatran and edoxaban have been developed according to the sequential approach.38 Randomized clinical trials compared fixed doses of DOACs with conventional anticoagulation (LMWH followed by vitamin K antagonists) in the treatment of VTEs in almost 27 000 patients.32-37 These phase 3 trials showed that each of the DOACs is non-inferior to conventional treatment. In a meta-analysis of randomized trials, treatment with DOACs was confirmed to be non-inferior to conventional treatment (relative risk [RR], 0.90; 95% CI, 0.77-1.06) with a significant reduction in the risk of major bleeding (RR, 0.61; 95% CI, 0.45-0.83), intracranial bleeding (RR, 0.37; 95% CI, 0.21-0.68), and fatal bleeding (RR, 0.36; 95% CI, 0.15-0.84).39 Improved efficacy in the safety profile of DOACs together with improved practicality makes DOACs the first choice for treating the majority of VTE patients.8,11
Anticoagulants for the treatment of VTE
| . | Dosage . | Practical issues . |
|---|---|---|
| Parenteral agents | ||
| Unfractionated heparin | Sodium heparin: 80 IU/kg bolus dose followed by 18 IU/kg per hour by continuous infusion | aPTT ratio maintained between 1.5 to 2.0 per normal value. No issue with renal failure. |
| Calcium heparin: first dose 333 IU/kg followed by 250 IU/kg SC twice per day or body weight–adjusted with initial IV bolus* | No monitoring required. No issue with renal failure. No data on use with thrombolysis or embolectomy. | |
| Enoxaparin SC | 1.0 mg/kg every 12 hours or 1.5 mg/kg once per day | To be reduced in case of renal failure. No evidence for dose adjustment based on coagulation tests. |
| Tinzaparin SC | 175 IU/kg once per day | To be reduced in case of renal failure. No evidence for dose adjustment based on coagulation tests. |
| Dalteparin SC | 100 IU/kg every 12 hours or 200 IU/kg once per day | To be reduced in case of renal failure. No evidence for dose adjustment based on coagulation tests. |
| Nadroparin SC | 86 IU/kg every 12 hours or 171 IU/kg once per day | No adjustment in case of renal failure. |
| Fondaparinux SC | Once per day: 5 mg (body weight <50 kg); 7.5 mg (body weight 50-100 kg); 10 mg (body weight >100 kg) | Avoid in case of renal failure. No evidence for dose adjustment based on coagulation tests. |
| Oral compounds | ||
| Rivaroxaban | 15 mg twice per day for 3 weeks followed by 20 mg once per day | No data if creatinine clearance <30 mL/min. Reduced dose (rivaroxaban 10 mg once per day) effective for secondary prevention. |
| Apixaban | 10 mg twice per day for 1 week followed by 5 mg twice per day | Reduced dose (apixaban 2.5 mg twice per day) effective for secondary prevention. |
| Edoxaban | 60 mg once per day following 5 to 7 days of parenteral treatment | Reduce to 30 mg according to predefined criteria.† |
| Dabigatran | 150 mg twice per day following 5 to 7 days of parenteral treatment | No data if creatinine clearance <30 mL/min. |
| Vitamin K antagonists | To be overlapped with parenteral anticoagulants and INR adjusted | No issue with renal failure. Target INR, 2.0 to 3.0. |
| . | Dosage . | Practical issues . |
|---|---|---|
| Parenteral agents | ||
| Unfractionated heparin | Sodium heparin: 80 IU/kg bolus dose followed by 18 IU/kg per hour by continuous infusion | aPTT ratio maintained between 1.5 to 2.0 per normal value. No issue with renal failure. |
| Calcium heparin: first dose 333 IU/kg followed by 250 IU/kg SC twice per day or body weight–adjusted with initial IV bolus* | No monitoring required. No issue with renal failure. No data on use with thrombolysis or embolectomy. | |
| Enoxaparin SC | 1.0 mg/kg every 12 hours or 1.5 mg/kg once per day | To be reduced in case of renal failure. No evidence for dose adjustment based on coagulation tests. |
| Tinzaparin SC | 175 IU/kg once per day | To be reduced in case of renal failure. No evidence for dose adjustment based on coagulation tests. |
| Dalteparin SC | 100 IU/kg every 12 hours or 200 IU/kg once per day | To be reduced in case of renal failure. No evidence for dose adjustment based on coagulation tests. |
| Nadroparin SC | 86 IU/kg every 12 hours or 171 IU/kg once per day | No adjustment in case of renal failure. |
| Fondaparinux SC | Once per day: 5 mg (body weight <50 kg); 7.5 mg (body weight 50-100 kg); 10 mg (body weight >100 kg) | Avoid in case of renal failure. No evidence for dose adjustment based on coagulation tests. |
| Oral compounds | ||
| Rivaroxaban | 15 mg twice per day for 3 weeks followed by 20 mg once per day | No data if creatinine clearance <30 mL/min. Reduced dose (rivaroxaban 10 mg once per day) effective for secondary prevention. |
| Apixaban | 10 mg twice per day for 1 week followed by 5 mg twice per day | Reduced dose (apixaban 2.5 mg twice per day) effective for secondary prevention. |
| Edoxaban | 60 mg once per day following 5 to 7 days of parenteral treatment | Reduce to 30 mg according to predefined criteria.† |
| Dabigatran | 150 mg twice per day following 5 to 7 days of parenteral treatment | No data if creatinine clearance <30 mL/min. |
| Vitamin K antagonists | To be overlapped with parenteral anticoagulants and INR adjusted | No issue with renal failure. Target INR, 2.0 to 3.0. |
aPTT, activated partial thromboplastin time; INR, international normalized ratio; IU, international units; SC, subcutaneously.
Or body weight <50 kg: 4000 IU IV bolus plus 12 500 IU SC twice per day; body weight 50-70 kg: 5000 IU IV bolus plus 15 000 IU SC twice per day; body weight >70 kg: 6000 IU IV bolus plus 17 500 IU SC twice per day.
At least one among patient body weight ≤60 kg; creatinine clearance ≤50 mL/min; concomitant potent P-glycoprotein inhibitors.
No randomized head-to-head comparisons between the single-drug approach and the sequential regimen are currently available. Thus, the need for parenteral treatment with heparin in the initial phase of VTE treatment remains undefined. This issue is a concern mainly in patients with severe presentations of PE or DVT who may have been excluded from clinical trials and in whom LMWH might be preferred over DOACs in the event of a need for treatment upgrade to reperfusion strategies.40
A landmark subanalysis of the Amplify study assessed the efficacy and safety of apixaban given as a single drug compared with conventional treatment with enoxaparin or warfarin at each time point: 7 days, 21 days, and 90 days from acute VTE. In that analysis, apixaban was non-inferior to conventional treatment at each time point, with no excess of early recurrences or bleeding, specifically at 7 days of treatment when the comparison was between apixaban and LMWH.41 These results were consistent in patients treated for both acute DVT and acute PE. However, it should be noted that limited information is available on the severity of VTE in patients included in phase 3 studies of DOACs. This may raise some concern on the generalizability of the results from these trials in the overall spectrum of VTE patients, mainly regarding the acute phase of treatment. Overall, more than 10 000 patients with acute PEs were included in DOAC trials. The efficacy of DOACs in patients with PE is consistent, regardless of the burden of emboli at diagnosis32,33,35-37 ; however, no association exists between the burden of emboli at CT angiography and mortality in the short term after a PE.8,16 In a subanalysis of the Hokusai study,42 LMWH followed by edoxaban was more effective than conventional treatment in preventing 6-month recurrences of VTEs in patients with PEs and right ventricle dysfunction as assessed by measuring levels of NT-pro-brain natriuretic peptide. However, in that study, all patients received initial parenteral anticoagulation. In the Einstein PE study,35 the single-drug approach with rivaroxaban was compared with conventional treatment in almost 5000 PE patients. However, almost 54% of patients included in that study had a low risk for death according to the simplified Pulmonary Embolism Severity Index (PESI) score, and no assessment of right ventricle dysfunction was reported. Further evidence is awaited on the need for heparin lead-in in hemodynamically stable patients with acute PE and signs of right ventricle dysfunction and injury (Figure 2). Concerning patients with DVT, the efficacy-to-safety profile of DOACs was confirmed in patients with thrombosis at the iliac level compared with femoral or popliteal thrombosis.
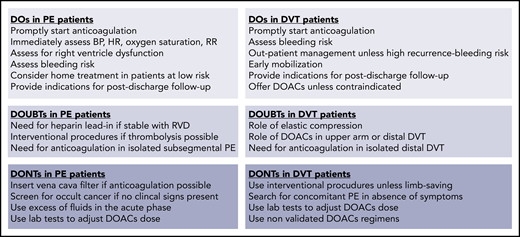
Practical indications on actions to do (DOs) or to not do (DONTs) in patients with acute VTE. BP, blood pressure; HR, heart rate; RR, respiratory rate.
Practical indications on actions to do (DOs) or to not do (DONTs) in patients with acute VTE. BP, blood pressure; HR, heart rate; RR, respiratory rate.
Patients who required reperfusion were excluded from the trials on DOACs for the treatment of VTE. Thus, initial anticoagulation with heparin should be preferred in candidates for revascularization.8,10,11 Currently recommended thrombolytic regimens for the treatment of acute PE have been evaluated in combination with unfractionated heparin given as an initial bolus dose followed by a continuous infusion started after the completion of thrombolysis.8,10,11 A shift to LMWH was allowed early after completion of thrombolysis in recent clinical trials on thrombolytic therapy for acute PE. Only limited and mainly uncontrolled data are currently available on the use of thrombolytic treatment in association with LMWH, fondaparinux, or DOACs in PE patients.43-45 In randomized studies on the treatment of DVT, unfractionated heparin was usually continued during infusion of thrombolytic agents.46,47 Contemporary studies in DVT patients also allowed the use of LMWH during infusion of thrombolytic agents.48 While waiting for further evidence, initiation of DOACs should probably be delayed for at least 24 hours after thrombolysis or mechanical reperfusion in VTE patients.
Reperfusion: candidates and strategies
Reperfusion strategies are currently used in a minority of patients with VTE and are reserved specifically for those with severe presentations (about 4.5% of patients with DVT and 6.2% of patients with acute PE) to rapidly restore vascular patency and potentially improve clinical outcome.49 These treatments can be lifesaving and are warranted whenever there is an indication, specifically in patients with acute PE and hemodynamic instability or with DVT and impending venous gangrene. Currently recommended agents and strategies for reperfusion in VTE patients are provided in Table 2.
Drugs and devices for pharmacologic and interventional reperfusion treatment of VTE
| . | Systemic thrombolysis for acute PE (approved regimens) . | |
|---|---|---|
| Dose regimen . | Practical issues or device used for reperfusion . | |
| Thrombolytic agent | ||
| Recombinant tissue-type plasminogen activator | 100 mg over 2 hours or 0.6 mg/kg over 15 minutes (maximum dose, 50 mg) | Absolute contraindications: History of hemorrhagic stroke, stroke at ≤6 months, central nervous system tumor, major trauma, surgery, or head injury at ≤3 weeks, bleeding diathesis, active bleeding |
| Streptokinase | 250 000 IU loading dose over 30 minutes, followed by 100 000 IU/h over 12 to 24 hours; accelerated regimen: 1.5 million IU over 2 hours | Relative contraindications: Transient ischemic attack at ≤6 months, oral anticoagulation, pregnancy or first postpartum week, non-compressible puncture sites, traumatic resuscitation, refractory hypertension (systolic blood pressure >180 mmHg), advanced liver disease, infective endocarditis, active peptic ulcer |
| Urokinase | 4400 IU/kg loading dose over 10 minutes followed by 4400 IU/kg per hour over 12 to 24 hours; accelerated regimen: 3 million IU over 2 hours | |
| Catheter interventions | ||
| With thrombolysis for acute PE | ||
| Catheter-directed thrombolysis | Alteplase 25 mg | UniFuse, Cragg-McNamara |
| Ultrasound-assisted catheter-directed thrombolysis | Alteplase 24 mg (1 mg/h for 24 hours if unilateral; 1 mg/h via catheter for 12 hours if bilateral) | EkoSonic 5.2F 12-cm treatment zone device |
| Rheolytic thrombectomy plus catheter-directed thrombolysis | 4 to 12 mg alteplase per lung and infusion duration from 2 to 6 hours | AngioJet thrombectomy with Power Pulse thrombolysis |
| Combined techniques | Urokinase 250 000 to 500 000 U or alteplase 25 mg | Pigtail fragmentation plus AngioJet thrombectomy |
| Without thrombolysis for acute PE | ||
| Aspiration thrombectomy (suction pump or manual) | Start UFH bolus and delay continuous infusion until the completion of the procedure (additional unfractionated heparin boluses to be given during the procedure at the physician’s discretion) | Angiovac suction cannula: Indigo Mechanical Sheath with detachable hemostatic valve, multipurpose guide catheter, aspiration syringe. |
| Mechanical thrombectomy | Flowtriever, AngioJet catheter, Pigtail catheter | |
| Rheolytic thrombectomy | ||
| Thrombus fragmentation combined techniques | ||
| With thrombolysis for acute DVT | ||
| Catheter-directed thrombolysis | Alteplase 0.5-1.0 mg/h or 0.01 mg/kg per hour | AngioJet device |
| Ultrasound-assisted catheter-directed thrombolysis | Concomitant intravenous infusion of unfractionated heparin at subtherapeutic levels | EkoSonic treatment zone device |
| Isolated thrombolysis power pulse technique | Need for vena cava filter insertion debated | Trellis Peripheral Infusion System, Angiojet Rheolytic Thrombectomy Catheter |
| . | Systemic thrombolysis for acute PE (approved regimens) . | |
|---|---|---|
| Dose regimen . | Practical issues or device used for reperfusion . | |
| Thrombolytic agent | ||
| Recombinant tissue-type plasminogen activator | 100 mg over 2 hours or 0.6 mg/kg over 15 minutes (maximum dose, 50 mg) | Absolute contraindications: History of hemorrhagic stroke, stroke at ≤6 months, central nervous system tumor, major trauma, surgery, or head injury at ≤3 weeks, bleeding diathesis, active bleeding |
| Streptokinase | 250 000 IU loading dose over 30 minutes, followed by 100 000 IU/h over 12 to 24 hours; accelerated regimen: 1.5 million IU over 2 hours | Relative contraindications: Transient ischemic attack at ≤6 months, oral anticoagulation, pregnancy or first postpartum week, non-compressible puncture sites, traumatic resuscitation, refractory hypertension (systolic blood pressure >180 mmHg), advanced liver disease, infective endocarditis, active peptic ulcer |
| Urokinase | 4400 IU/kg loading dose over 10 minutes followed by 4400 IU/kg per hour over 12 to 24 hours; accelerated regimen: 3 million IU over 2 hours | |
| Catheter interventions | ||
| With thrombolysis for acute PE | ||
| Catheter-directed thrombolysis | Alteplase 25 mg | UniFuse, Cragg-McNamara |
| Ultrasound-assisted catheter-directed thrombolysis | Alteplase 24 mg (1 mg/h for 24 hours if unilateral; 1 mg/h via catheter for 12 hours if bilateral) | EkoSonic 5.2F 12-cm treatment zone device |
| Rheolytic thrombectomy plus catheter-directed thrombolysis | 4 to 12 mg alteplase per lung and infusion duration from 2 to 6 hours | AngioJet thrombectomy with Power Pulse thrombolysis |
| Combined techniques | Urokinase 250 000 to 500 000 U or alteplase 25 mg | Pigtail fragmentation plus AngioJet thrombectomy |
| Without thrombolysis for acute PE | ||
| Aspiration thrombectomy (suction pump or manual) | Start UFH bolus and delay continuous infusion until the completion of the procedure (additional unfractionated heparin boluses to be given during the procedure at the physician’s discretion) | Angiovac suction cannula: Indigo Mechanical Sheath with detachable hemostatic valve, multipurpose guide catheter, aspiration syringe. |
| Mechanical thrombectomy | Flowtriever, AngioJet catheter, Pigtail catheter | |
| Rheolytic thrombectomy | ||
| Thrombus fragmentation combined techniques | ||
| With thrombolysis for acute DVT | ||
| Catheter-directed thrombolysis | Alteplase 0.5-1.0 mg/h or 0.01 mg/kg per hour | AngioJet device |
| Ultrasound-assisted catheter-directed thrombolysis | Concomitant intravenous infusion of unfractionated heparin at subtherapeutic levels | EkoSonic treatment zone device |
| Isolated thrombolysis power pulse technique | Need for vena cava filter insertion debated | Trellis Peripheral Infusion System, Angiojet Rheolytic Thrombectomy Catheter |
Reperfusion in acute PE
In patients with acute PE, thrombolytic therapy given either in an intrapulmonary manner or by a systemic route rapidly reduces pulmonary artery systolic pressure and anatomical extension of emboli.50 Regimens of accelerated infusions were developed in clinical studies on the basis of evidence that short infusions of high-dose alteplase may reduce bleeding risk.51 In studies of acute PE, systemic thrombolysis reduced mortality by about 50% (OR, 0.59; 95% CI, 0.36-0.96).52 The main alternative to thrombolysis is major bleeding (OR for major bleeding, 2.91; 95% CI, 1.95-4.36; OR for fatal or intracranial bleeding, 3.18; 95% CI, 1.25-8.11).52 To manage such a high bleeding risk, thrombolysis should be used in hemodynamically unstable patients with PEs, that is, those who are at high risk for death (Figure 1).8,10,11
Whether thrombolysis can be beneficial for patients with acute PE who are hemodynamically stable but have right ventricle dysfunction and increased troponin and those at an intermediate-high risk of death according to the European Society of Cardiology and with impending hemodynamic impairment according to North American guidelines, is still debated. In more than 1000 of these patients, bolus tenecteplase reduced the incidence of death at 7 days or hemodynamic deterioration compared with heparin alone (5.6% vs 2.6%; OR, 0.44; 95% CI, 0.23 to 0.87) at the cost of a 10-fold increase in intracranial bleeding.53 On the basis of these results, current guidelines discourage the use of thrombolytic treatment in hemodynamically stable PE patients because of bleeding concern. In addition, based on previous results, a drug-specific bleeding risk for tenecteplase cannot be excluded,54 and the drug has not been approved for patients with acute PE.
To overcome the bleeding issue associated with systemic thrombolysis, 2 alternative strategies for reperfusion are under evaluation in hemodynamically stable patients with acute PE and right ventricle dysfunction (Table 3). The first is local reperfusion by catheter-directed thrombolysis or mechanical thrombus debulking via fragmentation or aspiration (Table 2). Catheter-based local infusion of thrombolytic agents close to the pulmonary emboli allows the use of low-dose thrombolytics infused over 2 to 12 hours, depending on the burden of emboli and on the specific technique.55 The most recent randomized study showed that with very low doses of alteplase (4 to 12 mg per lung; infusion duration of 2 to 6 hours), the risk for bleeding is not negligible (4% major bleeding, 2% intracranial bleeding).56 Mechanical thrombus fragmentation, debulking, and aspiration of occlusive thrombi were associated with favorable outcome in 87% of the patients from registries and case series, but the risk for publication bias, the lack of procedure standardization, and the variability in definition of efficacy outcomes make these results difficult to be translated into general clinical practice.55,57 Moreover, the learning curve for all these procedures is not trivial, and the risk for complications outside expert centers is not negligible.
Ongoing studies in the antithrombotic treatment of adult patients who have acute PE with or without concomitant DVT
| Setting . | Intervention . | Study design . | ClinicalTrials.gov identifier . |
|---|---|---|---|
| Massive and submassive PE | Recombinant human prourokinase vs alteplase | Phase 2a randomized | NCT03108833 |
| High and intermediate-high risk PE with emboli in the pulmonary trunk or in the main pulmonary arteries | Surgical pulmonary embolectomy vs catheter-directed thrombolysis | Randomized, phase 2, non-inferiority | NCT03218410 |
| Acute submassive PE (radiologic extension) | Thrombin-activatable fibrinolysis inhibitor (DS-1040b) | Phase 1b, single ascending dose, randomized, double-blind, placebo-controlled | NCT02923115 |
| Normotensive right ventricular dysfunction | Percutaneous mechanical thrombectomy by indigo aspiration system | Prospective, single group | NCT03218566 |
| Intrapulmonary thrombolysis by Bashir endovascular catheter | Prospective, single group | NCT03927508 | |
| Catheter-directed thrombolysis vs ultrasound-assisted thrombolysis | Randomized controlled | NCT02758574 | |
| Diuretic vs vascular filling | Randomized controlled | NCT02531581 | |
| Supplemental oxygen added to conventional anticoagulant treatment vs standard management | Randomized, open label | NCT04003116 | |
| Nitric oxide (inhaled) vs placebo | Randomized, triple blind | NCT01939301 | |
| Sildenafil + apixaban vs apixaban | Randomized, open label | NCT02946944 | |
| Isolated subsegmental PE | No anticoagulant treatment of patients with isolated subsegmental emboli and negative serial bilateral lower extremity ultrasound | Prospective cohort | NCT01455818 |
| Hemodynamically stable symptomatic PE | HESTIA vs PESI scores for acute management concerning home treatment | Randomized, open label | NCT02811237 |
| Normotensive right ventricular dysfunction and/or increased biomarkers | LMWH for 72 hours followed by dabigatran | Prospective, single-group assignment | NCT02596555 |
| Intermediate-high risk PE | Alteplase + UFH followed by apixaban vs placebo + UFH followed by apixaban | Randomized, quadruple blind | NCT03988842 |
| Setting . | Intervention . | Study design . | ClinicalTrials.gov identifier . |
|---|---|---|---|
| Massive and submassive PE | Recombinant human prourokinase vs alteplase | Phase 2a randomized | NCT03108833 |
| High and intermediate-high risk PE with emboli in the pulmonary trunk or in the main pulmonary arteries | Surgical pulmonary embolectomy vs catheter-directed thrombolysis | Randomized, phase 2, non-inferiority | NCT03218410 |
| Acute submassive PE (radiologic extension) | Thrombin-activatable fibrinolysis inhibitor (DS-1040b) | Phase 1b, single ascending dose, randomized, double-blind, placebo-controlled | NCT02923115 |
| Normotensive right ventricular dysfunction | Percutaneous mechanical thrombectomy by indigo aspiration system | Prospective, single group | NCT03218566 |
| Intrapulmonary thrombolysis by Bashir endovascular catheter | Prospective, single group | NCT03927508 | |
| Catheter-directed thrombolysis vs ultrasound-assisted thrombolysis | Randomized controlled | NCT02758574 | |
| Diuretic vs vascular filling | Randomized controlled | NCT02531581 | |
| Supplemental oxygen added to conventional anticoagulant treatment vs standard management | Randomized, open label | NCT04003116 | |
| Nitric oxide (inhaled) vs placebo | Randomized, triple blind | NCT01939301 | |
| Sildenafil + apixaban vs apixaban | Randomized, open label | NCT02946944 | |
| Isolated subsegmental PE | No anticoagulant treatment of patients with isolated subsegmental emboli and negative serial bilateral lower extremity ultrasound | Prospective cohort | NCT01455818 |
| Hemodynamically stable symptomatic PE | HESTIA vs PESI scores for acute management concerning home treatment | Randomized, open label | NCT02811237 |
| Normotensive right ventricular dysfunction and/or increased biomarkers | LMWH for 72 hours followed by dabigatran | Prospective, single-group assignment | NCT02596555 |
| Intermediate-high risk PE | Alteplase + UFH followed by apixaban vs placebo + UFH followed by apixaban | Randomized, quadruple blind | NCT03988842 |
A second strategy is systemic safe thrombolysis either by low-dose alteplase or by newer agents. On the basis of favorable preliminary data,58,59 a randomized trial is ready to start that is aimed at assessing the efficacy and safety of low-dose alteplase vs placebo in hemodynamically stable patients with acute PE, all receiving anticoagulant treatment (Table 3). Injectable versions of thrombin activatable fibrinolysis inhibitors are under evaluation in the treatment of patients with acute PE along with anticoagulant treatment (Table 3).60 While waiting for new evidence, systemic thrombolysis should be reserved for hemodynamically unstable patients with acute PE, and percutaneous reperfusion should be reserved for those with absolute contraindications for systemic thrombolysis or those who are admitted to medical centers that have specific expertise in the procedure.8,10,11,55
Reperfusion in acute DVT
Randomized controlled trials compared catheter-directed reperfusion strategies plus anticoagulation with anticoagulation alone in reducing postthrombotic syndrome (PTS) in patients with acute DVT.61-64 Reperfusion techniques vary on the basis of their association with local thrombolysis or the type of mechanical strategy used. A randomized controlled study found a modest advantage for catheter-directed in situ thrombolysis plus anticoagulation over anticoagulation alone with regard to occurrence of PTS up to 2 years after diagnosis.61 In the largest of these trials, the addition of pharmaco-mechanical catheter-directed thrombolysis to anticoagulation did not reduce the incidence of PTS (47% vs 48%; risk ratio, 0.96; 95% CI, 0.82-1.11) and resulted in a higher risk of major bleeding (1.7% vs 0.3% of patients; P = .049) compared with anticoagulation alone.46 Patients treated with catheter-directed thrombolysis had lower rates of moderate-to-severe PTS at 6, 12, 18, and 24 months. However, quality of life did not differ significantly between groups. Although a potential benefit in patients with more extensive ilio-femoral thrombosis cannot be excluded in this study, no advantage was shown in patients with femoropopliteal DVT.65 On the basis of these results, reperfusion techniques should be reserved for highly selected patients with limb-threatening disease and those with ilio-femoral acute DVT and local severe symptoms (eg, phlegmasia) with low bleeding risk.10,11,66 Studies are currently ongoing that aim to assess the efficacy and safety of reperfusion strategies in DVT patients (Table 4). While awaiting the results of these studies, it should be noted that the use of thrombolytics to treat DVT either by systemic or locoregional infusion is off label because none of these agents have been approved by the US Food and Drug Administration for this indication.
Ongoing studies on acute antithrombotic treatment of adult patients with acute DVT
| Study setting . | Interventions . | Study design . | ClinicalTrials.gov identifier . |
|---|---|---|---|
| Symptomatic isolated distal DVT | Rivaroxaban vs placebo for 6 weeks duration after a standard 6-week treatment with rivaroxaban | Randomized, double-blind | NCT02722447 |
| Isolated calf DVT | Apixaban vs placebo | Phase 4, randomized, double-blind | NCT03590743 |
| Symptomatic acute VTE (proximal lower extremity DVT or segmental or greater PE) | Apixaban vs rivaroxaban | Phase 4, randomized, open-label | NCT03266783 |
| VTE treatment in patients with renal impairment | Apixaban (10 mg twice per day for 7 days followed by 2.5 mg twice per day) or rivaroxaban (15 mg twice per day followed by 15 mg once per day) vs standard of care (LMWH/VKA or UFH/VKA) | Randomized, open-label non-inferiority | NCT02664155 |
| Acute common and/or external iliac or common femoral DVT | Pharmaco-mechanical thrombolysis with or without stenting | Prospective cohort | NCT03901872 |
| Study setting . | Interventions . | Study design . | ClinicalTrials.gov identifier . |
|---|---|---|---|
| Symptomatic isolated distal DVT | Rivaroxaban vs placebo for 6 weeks duration after a standard 6-week treatment with rivaroxaban | Randomized, double-blind | NCT02722447 |
| Isolated calf DVT | Apixaban vs placebo | Phase 4, randomized, double-blind | NCT03590743 |
| Symptomatic acute VTE (proximal lower extremity DVT or segmental or greater PE) | Apixaban vs rivaroxaban | Phase 4, randomized, open-label | NCT03266783 |
| VTE treatment in patients with renal impairment | Apixaban (10 mg twice per day for 7 days followed by 2.5 mg twice per day) or rivaroxaban (15 mg twice per day followed by 15 mg once per day) vs standard of care (LMWH/VKA or UFH/VKA) | Randomized, open-label non-inferiority | NCT02664155 |
| Acute common and/or external iliac or common femoral DVT | Pharmaco-mechanical thrombolysis with or without stenting | Prospective cohort | NCT03901872 |
VKA, vitamin K antagonist.
Vena cava filters
Insertion of a vena cava filter is not a treatment for VTE; instead, it is an attempt to block emboli from migrating from the lower limbs to the lung. Having inserted a vena cava filter does not eliminate the need for anticoagulant treatment.67 In fact, insertion of a vena cava filter is associated with increased risk for proximal extension of DVT, and there is the potential for increased mortality if therapeutic anticoagulation is not started in patients with either initial DVT or PE.68,69 In patients with absolute contraindications to anticoagulant treatment, a vena cava filter may reasonably reduce the risk of PE until anticoagulation can be started. Careful reassessment of bleeding risk should be scheduled in patients who had a vena cava filter inserted so that anticoagulation can be started as soon as possible.8,11 Whether the insertion of a vena cava filter is beneficial in hemodynamically unstable PE patients and before catheter-directed thrombolysis in patients with DVT requires additional study.
Home treatment and patient disposition
Considerable variability is reported worldwide in the disposition of VTE patients, probably as a result of health system organization and locally available expertise. In general, home treatment is the standard of care for the majority of patients with acute DVT, whereas hospitalization is the standard of care for the majority of patients with acute PE.70 It is conceivable that the availability of DOACs for treating VTE will help increase the feasibility of home treatment and short hospitalizations, although this should not lead to considering the disease and its treatment as trivial.
Comorbidities and advanced age are probably the major determinants of hospitalization in addition to the severity of VTE. An updated meta-analysis of randomized controlled trials showed that in patients with DVT, home treatment is associated with reduced recurrences of VTE (risk ratio, 0.58; 95% CI, 0.39-0.86) with similar risk for major bleeding (risk ratio, 0.67; 95% CI, 0.33-1.36) or mortality (risk ratio, 0.69; 95% CI, 0.44-1.09) compared with standard hospitalization.71 The main limits of these analyses are the high numbers of excluded patients, partial hospital treatment of many patients in the home treatment arms, and comparison of unfractionated heparin given in the hospital vs LMWH at home in the majority of the included studies.
Regarding patients with PE, home treatment is limited by the potential need for oxygen therapy or parenteral analgesia but also by the life-threatening nature of the disease. One randomized trial compared home treatment or early discharge (hospitalization <24 hours) with standard hospitalization in patients at low risk for death according to the PESI score.72 No significant difference was observed between the 2 management groups in terms of recurrent VTE (0.6% vs 0%), death (0.6% vs 0.6%), or major bleeding (1.8% vs 0%).The use of pragmatic criteria (Hestia criteria) to select patients with acute PE for home treatment resulted in acceptable rates of recurrent VTE (2%; 95% CI, 0.75%-4.3%), death (1.0%; 95% CI, 0.21%-2.9%), and major bleeding (0.67%; 95% CI, 0.082%-2.4%) at 3 months.73 An international study has explored the feasibility of home treatment or early discharge (<48 hours) in 525 patients with acute PE at low risk for death based on Hestia criteria and on the absence of right ventricle dysfunction, all treated with rivaroxaban according to the single-drug approach.74 Symptomatic recurrent VTE occurred in 0.6% of patients (95% CI upper limit, 2.1%), major bleeding in 1.2%, and PE-related death in none of the patients. Overall, these studies together with all the others on this issue, confirmed that home treatment or early discharge are feasible and safe in selected patients with acute PE. Whether the assessment of right ventricle dysfunction is required to select PE patients for home treatment is a matter of debate. In fact, although the presence of right ventricle dysfunction is associated with a fourfold risk for death, the absolute risk for death is as low as 1.8% (95% CI, 0.9%-3.5%) in patients at low risk for death according to clinical models.75 Thus, right ventricle assessment would preclude about 34% of low-risk patients from early discharge (95% CI, 30%-39%) to potentially identify 1.8% that will die or 3.5% that will experience a PE-related adverse outcome. Moreover, the unblinded and non-randomized design of the studies included in the meta-analysis could limit the quality of the evidence in favor of an adverse prognosis.
Intermediate-risk PE patients with signs of right ventricle dysfunction who have a non-negligible risk for death or hemodynamic deterioration at 7 days may benefit from close observation. However, whether hospitalization in acute care units improves the clinical outcome of these patients has yet to be explored. For hemodynamically stable or unstable VTE patients who are candidates for reperfusion, the optimal disposition depends on local health system organization. These patients should be admitted to units that can offer prompt reperfusion, monitoring, and eventual treatment upgrading. As an example, extracorporeal membrane oxygenation (ECMO) has been proposed to assist hemodynamics and allow further attempts at treatment for patients admitted to the hospital who are in cardiac arrest as a result of PE.8 However, the clinical value of ECMO is being debated because the procedure could exclude patients from rapid and effective pharmacologic reperfusion, it requires that either a surgical or an intervention team are immediately available for embolectomy,76 and it is associated with a high incidence of bleeding complications.77 Moreover, ECMO is currently available only in a minority of hospitals and may be impractical or even infeasible in many clinical settings. PE response teams have been designed and activated in many hospitals worldwide to help overcome the quandary that practicing physicians face in weighing different management options for PE, improving access to advanced therapies, and streamlining individual patient care.78 These teams merge the expertise of a variety of specialists in real time and enhance clinical decision making. However, PE may require rapid decision-making, mainly in unstable patients. Thus, whether activating such teams except for very complicated or extreme patient cases is associated with improved patient outcome remains to be determined.79 Ad hoc multidisciplinary pathways should also be planned for DVT patients who are candidates for reperfusion.
Role of patients’ characteristics in decision-making regarding anticoagulant treatment
The mean age of patients included in recent registries dedicated to VTE is about 60 years (standard deviation ± 19 years; interquartile range, 46.1-71.7 years)50,80 similar to that of patients included in administrative data set studies dedicated to VTE.81-83 Patients included in phase 3 trials of treatment for VTE were 5 to 10 years younger, which may mean that the reproducibility of the results of phase 3 studies in different populations is questionable.32-37 In a meta-analysis of phase 3 randomized controlled trials, DOACs were more effective (risk ratio, 0.56; 95% CI, 0.38-0.82) and safer (risk ratio, 0.49; 95% CI, 0.25-0.96) than conventional treatment in 3665 patients age 75 years or older (about 14% of the entire study population).39 In the same meta-analysis, DOACs were non-inferior (risk ratio, 0.70; 95% CI, 0.43-1.15) and safer (risk ratio, 0.51; 95% CI, 0.26-0.99) compared with conventional treatment in 1789 patients who had creatinine clearance between 50 and 39 mL per minute (about 6.6% of the entire study population). Different from the clinical development in patients with atrial fibrillation, no dose adjustment was scheduled in clinical trials that used DOACs (except for edoxaban) to treat patients with acute VTE.38 The efficacy-to-safety profile of edoxaban was consistent in patients randomly assigned to 30 or 60 mg compared with conventional treatment.37 The prevalence of renal failure in VTE patients differs on the basis of study designs, settings, and definition of renal failure and could reach 16%.80 Dose adjustments are recommended by the European Medical Agency for dabigatran in patients age 80 years or older or those between age 75 and 80 years if creatinine clearance is between 50 and 30 mL per minute, and for rivaroxaban if creatinine clearance is between 50 and 30 mL per minute. These adjustments are based on pharmacokinetics simulations more than clinical data and have not been endorsed by other medical agencies or international guidelines.8 The absence of clinical data generates some concern for the risk of downgrading to potentially ineffective treatment.84,85 In fact, the use of DOAC regimens noncompliant with those evaluated in clinical trials could be associated with increased risk for both recurrent VTE and bleeding complications.84 High-quality data are awaited for adjusted doses of DOACs before these can be used in clinical practice (Table 5).
Management of anticoagulant treatment in specific patient categories
| Clinical setting . | Patients subgroups . | Limitations . | Recommended strategies . |
|---|---|---|---|
| Renal function | Stage I-II KDOQI (GFR ≥60) | None | DOACs |
| Stage III KDOQI (GFR 59-30) | Dose reduction not tested in VTE | DOACs | |
| Stage IV KDOQI (GFR 29-15) | Avoid DOACs | VKAs or halved-dose LMWH | |
| Dialysis | Avoid DOACs & LMWH | VKAs | |
| Elderly | Over 75 years | Very limited data available | DOACs |
| Comorbidities & concomitant therapies | Adapt accordingly | ||
| Consider bleeding risk | Consider to avoid thrombolysis | ||
| Polypharmacotherapy | Strong inhibitors/competitors | Potential DOACs overdosing | Consider to avoid DOACs |
| Strong inducers/competitors | Potential DOACs underdosing | Consider to avoid DOACs | |
| Moderate inhibitors/inducers | Consider potential interactions | Consider DOACs at standard dose | |
| Dual antiplatelet | Consider to stop ≥1 antiplatelet | Consider DOACs (with ASA) | |
| Pregnancy & breast-feeding | Pregnancy I trimester | Avoid DOACs & VKAs | LMWH |
| Pregnancy II-III trimesters | Avoid DOACs | LMWH | |
| Breast-feeding | Avoid DOACs & VKAs | LMWH | |
| Cancer | Oral route not feasible | Avoid DOACs | LMWH |
| Gastrointestinal cancer | Avoid DOACs | LMWH (DOACs second choice) | |
| On chemotherapy | Assess for DOACs interactions | Edoxaban/rivaroxaban or LMWH | |
| Isolated Distal DVT | Asymptomatic DVT | Limited data available | Consider US surveillance |
| Cancer or previous VTE | Treat as proximal | LMWH or VKAs (or DOACs) | |
| All symptomatic distal DVT | Limited observational data with DOACs | LMWH or VKAs (or DOACs) | |
| Isolated Subsegmental PE | Asymptomatic incidental PE | Limited data available | Consider clinical surveillance or DOACs |
| Concomitant cancer | Treat as PE | Edoxaban/rivaroxaban or LMWH | |
| Symptomatic PE | Treat as PE | DOACs | |
| Vena cava filter | Absolute contraindications for anticoagulant treatment | Limited data available with DOACs | Start anticoagulant treatment as soon as possible |
| Clinical setting . | Patients subgroups . | Limitations . | Recommended strategies . |
|---|---|---|---|
| Renal function | Stage I-II KDOQI (GFR ≥60) | None | DOACs |
| Stage III KDOQI (GFR 59-30) | Dose reduction not tested in VTE | DOACs | |
| Stage IV KDOQI (GFR 29-15) | Avoid DOACs | VKAs or halved-dose LMWH | |
| Dialysis | Avoid DOACs & LMWH | VKAs | |
| Elderly | Over 75 years | Very limited data available | DOACs |
| Comorbidities & concomitant therapies | Adapt accordingly | ||
| Consider bleeding risk | Consider to avoid thrombolysis | ||
| Polypharmacotherapy | Strong inhibitors/competitors | Potential DOACs overdosing | Consider to avoid DOACs |
| Strong inducers/competitors | Potential DOACs underdosing | Consider to avoid DOACs | |
| Moderate inhibitors/inducers | Consider potential interactions | Consider DOACs at standard dose | |
| Dual antiplatelet | Consider to stop ≥1 antiplatelet | Consider DOACs (with ASA) | |
| Pregnancy & breast-feeding | Pregnancy I trimester | Avoid DOACs & VKAs | LMWH |
| Pregnancy II-III trimesters | Avoid DOACs | LMWH | |
| Breast-feeding | Avoid DOACs & VKAs | LMWH | |
| Cancer | Oral route not feasible | Avoid DOACs | LMWH |
| Gastrointestinal cancer | Avoid DOACs | LMWH (DOACs second choice) | |
| On chemotherapy | Assess for DOACs interactions | Edoxaban/rivaroxaban or LMWH | |
| Isolated Distal DVT | Asymptomatic DVT | Limited data available | Consider US surveillance |
| Cancer or previous VTE | Treat as proximal | LMWH or VKAs (or DOACs) | |
| All symptomatic distal DVT | Limited observational data with DOACs | LMWH or VKAs (or DOACs) | |
| Isolated Subsegmental PE | Asymptomatic incidental PE | Limited data available | Consider clinical surveillance or DOACs |
| Concomitant cancer | Treat as PE | Edoxaban/rivaroxaban or LMWH | |
| Symptomatic PE | Treat as PE | DOACs | |
| Vena cava filter | Absolute contraindications for anticoagulant treatment | Limited data available with DOACs | Start anticoagulant treatment as soon as possible |
ASA, low-dose aspirin; GFR, glomerular filtration rate in mL/min/1.73 m2; KDOQI, Kidney Disease Outcomes Quality Initiative.
Women represent an unusual population when dealing with the safety of DOACs. Increased risk for uterine bleeding has been reported with rivaroxaban (hazard ratio, 2.13; 95% CI, 1.57-2.89) and edoxaban (OR, 1.6; 95% CI, 1.0-2.4), and in terms of relative occurrence, apixaban has been compared with warfarin (OR, 3.4; 95% CI, 1.8-6.7).86-88 Dabigatran was associated with a 41% (95% CI, 10%-61%) reduction in the risk of abnormal uterine bleeding compared with warfarin .89 Whether these findings should discourage physicians from using some of the DOACs in young women is a matter of debate. In fact, the majority of abnormal uterine bleeding occurrences did not reach the criteria for a major AE and were managed without hospitalization. All DOACs pass through the placenta, although there is no clear evidence of embryopathy or fetal toxicity at this time. The prevalence of abnormalities was 5.1% in 233 cases of pregnant women being exposed to DOACs, of which 3 (2.2%) abnormalities were interpreted as embryopathies.90 DOACs also transfer to breast milk. Vitamin K antagonists are associated with malformations when used during the first trimester of pregnancy and are secreted in breast milk. For these reasons, LMWHs are the agents of choice for treatment of VTE in this context because these agents do not cross the placenta (Table 5).8,11,66 Case reports for 215 pregnant women, suggest a lower incidence of maternal and fetal complications with systemic thrombolysis (183 women) compared with catheter-directed thrombolysis (19 women), but no complications were observed with mechanical thrombectomy (13 women).91 The non-randomized nature of these observations and the limited number of patients managed with interventional procedures do not allow any conclusion to be drawn regarding the feasibility of such treatments in emergency situations.
LMWHs are more effective than warfarin with a similar safety profile (RR for recurrent VTE, 0.58; 95% CI, 0.43-0.77; RR for major bleeding, 1.09; 95% CI, 0.55-2.12) when used to treat VTE in patients with cancer.92 To overcome the limit of prolonged parenteral administration and to search for safer agents, randomized studies have been conducted with DOACs in patients with cancer-associated VTE.93,94 Overall, these studies suggested an improved efficacy of edoxaban and rivaroxaban at the cost of an increased incidence of bleeding complications, mainly at the gastrointestinal site, compared with LMWH. A trial is ongoing comparing apixaban with dalteparin in this setting.95 It is conceivable that the available and ongoing studies, together with other randomized studies with smaller sample size, will not provide enough evidence for the treatment of cancer-associated VTE in specific types of cancer such as brain cancer or brain metastases. In these patients, anticoagulant treatment is associated with an almost twofold increase in the risk for intracranial hemorrhage that is mainly accounted for by patients with gliomas.96 The role of a vena cava filter in these patients and in patients with severe thrombocytopenia should be evaluated on an individual patient basis. The need for anticoagulant therapy in patients with cancer and incidental VTE is uncertain because limited data are available on the incidence of recurrent VTE in untreated patients, and there is limited evidence from randomized studies. Whether clinical surveillance can be safe in isolated incidental distal DVT and isolated incidental subsegmental PE requires further investigation in ad hoc clinical trials (Table 5).
The role of anticoagulant treatment in patients with isolated distal DVT or isolated subsegmental PE is controversial.8,10,11,66 In a randomized study in low-risk patients (without active cancer or previous VTE) who have isolated distal DVT, the incidence of symptomatic VTE was similar with either LMWHs or placebo (3.3% vs 5.4%) whereas bleeding occurred more frequently with LMWHs (5 vs 0 patients).97 In a meta-analysis, anticoagulation (either therapeutic or prophylactic) was associated with reduction of recurrent VTEs (OR, 0.50; 95% CI, 0.31-0.79) and PE (OR, 0.48; 95% CI, 0.25-0.91) without an increase in the risk of major bleeding (OR, 0.64; 95% CI, 0.15-2.73).98 These results were confirmed when the analysis was limited to randomized studies. However, there is no consensus that distal DVT requires anticoagulant treatment.11,66 The presence of symptoms and the patient’s bleeding risk and comorbidities should also be taken into account when making decisions on type of anticoagulant treatment in this setting (Table 5). Results of ongoing studies with DOACs are awaited in patients with isolated distal DVT (Table 4). Similarly, the need for anticoagulant treatment in patients with isolated subsegmental PE is matter of debate (Table 5).8,11,15 Evidence from high-quality clinical studies is needed to confirm the safety of withholding anticoagulation in patients with isolated subsegmental PE, mainly in the absence of symptoms.
Compression therapy for DVT
The role of compression therapy in the management of patients with acute DVT is debated because of the overall low methodologic quality of existing trials, which leads to conflicting results.99 Use of early compression (<24 hours from diagnosis) associated with early walking exercise has been shown to be beneficial in controlling symptoms of acute proximal DVT (swelling, pain, hyperpigmentation, induration, venous enlargement). No difference was found in the incidence of PTS in studies that evaluate compression vs no compression treatment in the acute phase of DVT (RR, 0.76; 95% CI, 0.49-1.16). In a recent study in 865 patients with proximal DVT, early compression therapy reduced residual vein obstruction (OR, 0.46; 95% CI, 0.27-0.80), which is a predictor of PTS.100
In conclusion, acute treatment of VTE has an essential role in reducing the risk for adverse outcome events. Therapeutic anticoagulation should be used in all VTE patients in the absence of absolute contraindications. Reperfusion therapies should be reserved for hemodynamically unstable patients with PE and/or patients with limb-threatening DVT. The role of interventional procedures should also be based on their availability and the availability of local expertise. The results of ongoing studies could further refine the treatment of acute VTE.
Authorship
Contribution: C.B. designed and wrote the paper; and G.A. designed the paper and contributed to critical review of the paper.
Conflict-of-interest disclosure: C.B. has received lecturer’s fees and served as a consultant for Bayer HealthCare, Bristol-Myers Squibb, and Daiichi Sankyo. G.A. has received lecturer’s fees from Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, and Daiichi Sankyo.
Correspondence: Cecilia Becattini, Internal and Cardiovascular Medicine–Stroke Unit, University of Perugia, Piazzale Menghini 1, 06129 Perugia, Italy; e-mail: cecilia.becattini@unipg.it

![Patient management based on risk of death or VTE-related complications at presentation. (°) If available and feasible, extracorporeal membrane oxygenation (ECMO) can be used to support hemodynamics in patients with cardiac arrest. In this case, percutaneous or surgical embolectomy should be preferred over systemic thrombolysis to avoid bleeding. In patients not managed by ECMO, systemic thrombolysis offers the opportunity for rapid reperfusion. (§) catheter-directed therapy to be considered for patients with contraindications for or failure of systemic thrombolysis. (*) Clinical risk assessed by validated models (Pulmonary Embolism Severity Index [PESI], simplified PESI) or based on the combination of vital status and comorbidities. (**) Heparin lead-in stands for initial 5 to 9 days of heparin treatment. (°°) Right ventricle dysfunction (RVD) assessed at echocardiography or computed tomography. (^) Early discharge is defined as occurring within 48 hours from admission. (^^) Treatment should be considered in patients with cancer who have symptoms or are at high risk for VTE. DOAC, direct oral anticoagulant; LMWH, low molecular weight heparin; UFH, unfractionated heparin; iv, intravenous.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/135/5/10.1182_blood.2019001881/5/m_bloodbld2019001881cf1.png?Expires=1769098267&Signature=oplDgidqK4UiLOmWh0Grjzi~u97mZv8CQYtySKOPmkTzOipmh6~rvwvCb4DbecYpN~xw8cLEztLcCcTNJ~ujVpk5DqlQCtYhlUyI9~Az6Y7LYntMAw~yxDl5-AmCzHDleqPTpAaIsHIldS85eTsfZjg5ohK-ki6hfXjW-1Rw3IVhzZRiKmRUSXetJ9rFcJz4Y4Y306eG81x7Vm8clrNcuZcxLMiKeBBDVupRoptuLRTDag336JUdxn7rx7d2iXisPfR-aHJpHk4STkxDlIt~d6c1ocmI7mcdPtIYHr3d~5qR7F39iFg0vccR9yhW3aUipgPoqh1gt~S0~BUI9yf6dQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)