Systemic glucocorticoids are the principal treatment for acute graft-versus-host disease (GVHD), which remains the major cause of non-relapse mortality (NRM) after allogeneic hematopoietic cell transplantation (HCT). However, there are no validated biomarkers that measure a patient's response to glucocorticoid therapy, and thus response is evaluated by the change in clinical symptom severity. A major weakness in the predictive power of clinical responses is that changes to all organs are weighted equally even though the major driver of NRM is irreversible damage to the crypts of the GI tract. Recent studies from the Mount Sinai Acute GVHD International Consortium (MAGIC) have validated an algorithm probability (MAP) that combines serum concentrations of two biomarkers of GVHD (REG3α and ST2) to generate an estimated probability of 6 month NRM for individual patients. The MAP has been considered a "liquid biopsy" that estimates the damage caused by GVHD to crypts throughout the lower GI tract (Hartwell et al., JCI Insight, 2017; Major-Monfried et al., Blood, 2018). We hypothesized that the change in MAP between start of treatment and 28 days later could serve as a response biomarker for GVHD and might compare favorably to the change in clinical symptoms that measures response to GVHD treatment, which is widely used as a surrogate for long term survival and is the primary endpoint in most GVHD treatment trials (Martin et al., BBMT, 2009; MacMillan et al., Blood, 2010).
We prospectively collected serum samples and clinical staging from 368 sequential HCT patients who received systemic treatment for acute GVHD in one of 20 MAGIC centers between January 2016 and February 2018. We measured the serum concentrations of REG3α and ST2 before and after systemic therapy for acute GVHD and computed MAPs, the changes in MAPs, and clinical responses for each patient.
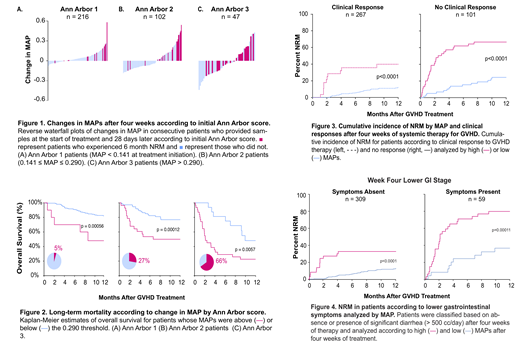
MAPs of patients who experienced 6 month NRM showed significantly greater increases than MAPs of patients who survived (p=0.0004). In patients whose MAPs at the start of treatment were low (Ann Arbor 1, MAP < 0.141) or intermediate (Ann Arbor 2, 0.141 ≤ MAP ≤ 0.290), 6 month NRM clustered among those who had the greatest increases in MAP after 28 days (Fig 1A,B). In patients with high MAPs at the start of treatment (Ann Arbor 3, MAP > 0.290), those who survived tended to have the largest decreases in MAP (Fig 1C). These changes in MAP suggested crossing a single threshold could predict risk of mortality. We found that patients whose MAPs rose above a threshold MAP of 0.290 (5% of Ann Arbor 1, 27% of Ann Arbor 2) had significantly worse survival compared to those who remained below it, whereas the large number patients with initially high MAPs that remained above the threshold (66% of Ann Arbor 3) had a large increases in mortality (Fig 2).
When measured at day 28, the MAP was significantly more accurate in predicting NRM than the gold standard of the clinical response, with areas under the receiver operating characteristic curve (AUC) of 0.86 and 0.70, respectively (p<0.0001). An algorithm that combined clinical response with biomarkers generated the same AUC as the MAP alone (0.83 v 0.86, p = NS). We next tested whether the same MAP threshold of 0.290 could predict risk within clinical response subsets. A significant minority (10%) of clinical responders had high MAPs and experienced three-fold greater NRM than those with low MAPs (40% v 12%, p<0.0001) whereas the majority (57%) of non-responders had low MAPs and experienced almost three-fold lower NRM than those with high MAPs (24% v 65%, p<0.0001) (Fig 3). Thus the MAP provides important prognostic information over and above the change in clinical symptoms, further stratifying both responders and non-responders at four weeks of treatment. The MAP threshold classified patients both with and without significant lower GI symptoms because the MAP is a more specific measure of irreversible cryptic damage in patients with copious diarrhea and more sensitive in patients with less than 0.5 liters of daily diarrhea (Fig 4).
We conclude that the MAP is, to our knowledge, the first validated laboratory test to serve as response biomarker for the treatment for acute GVHD and a more accurate predictor of survival than clinical response after four weeks of treatment. The MAP may serve as a novel endpoint and an important complement to changes in clinical symptom severity in future trials of GVHD treatment.
Srinagesh:National Institutes of Health: Research Funding. Ozbek:Viracor: Patents & Royalties: Biomarker Patent. Ayuk:Novartis: Honoraria, Other: Advisory Board, Research Funding. Aziz:Doris Duke Charitable Foundation: Research Funding. Defilipp:Incyte: Research Funding. Grupp:Novartis: Consultancy, Research Funding; Roche: Consultancy; GSK: Consultancy; CBMG: Consultancy; Novartis: Research Funding; Kite: Research Funding; Servier: Research Funding; Jazz: Other: study steering committees or scientific advisory boards; Adaptimmune: Other: study steering committees or scientific advisory boards; Cure Genetics: Consultancy; Humanigen: Consultancy. Hexner:novartis: Research Funding. Kitko:Mallinckrodt: Honoraria; Novartis: Consultancy, Honoraria. Mielke:EBMT/EHA: Other: Travel support; ISCT: Other: Travel support; Miltenyi: Consultancy, Honoraria, Other: Travel and speakers fee (via institution), Speakers Bureau; Jazz Pharma: Honoraria, Other: Travel support, Speakers Bureau; IACH: Other: Travel support; Kiadis Pharma: Consultancy, Honoraria, Other: Travel support (via institution), Speakers Bureau; DGHO: Other: Travel support; Bellicum: Consultancy, Honoraria, Other: Travel (via institution); GILEAD: Consultancy, Honoraria, Other: travel (via institution), Speakers Bureau; Celgene: Honoraria, Other: Travel support (via institution), Speakers Bureau. Merli:Sobi: Consultancy; Amgen: Honoraria; Novartis: Honoraria; Bellicum: Consultancy. Pulsipher:Amgen: Other: Lecture; Miltenyi: Research Funding; Bellicum: Consultancy; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Jazz: Other: Education for employees; CSL Behring: Membership on an entity's Board of Directors or advisory committees; Adaptive: Membership on an entity's Board of Directors or advisory committees, Research Funding; Medac: Honoraria. Qayed:Bristol-Myers Squibb: Honoraria. Reshef:Pfizer: Consultancy; Magenta: Consultancy; Kite: Consultancy, Research Funding; Atara: Consultancy, Research Funding; BMS: Consultancy; Pharmacyclics: Consultancy, Research Funding; Incyte: Consultancy, Research Funding; Celgene: Research Funding; Shire: Research Funding. Levine:Incyte: Consultancy, Research Funding; Biogen: Other: non-financial support; Viracor: Patents & Royalties: biomarker patent; Ironwood: Honoraria; bluebird bio: Consultancy; National Cancer Institute: Research Funding; Novartis: Honoraria; Kamada: Research Funding. Ferrara:National Institutes of Health: Research Funding; ViraCor: Consultancy; Incyte: Consultancy; Kamada: Consultancy; Mallinckrodt: Consultancy; Enlivex: Consultancy; Xenikos: Consultancy; CSL Behring: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal