In this issue of Blood, Zhang et al report on the treatment of newly diagnosed idiopathic multicentric Castleman disease (iMCD) with the combination of oral thalidomide, cyclophosphamide, and prednisone (TCP), providing an alternative to anti–interleukin-6 (IL-6) monoclonal antibodies (mAbs), especially when these are not readily available.1
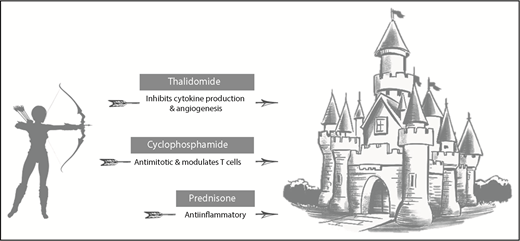
The TCP regimen assails idiopathic Castleman disease through multiple mechanisms of action.
The TCP regimen assails idiopathic Castleman disease through multiple mechanisms of action.
Significant progress has been made in recent years in the field of multicentric Castleman disease (MCD). The Castleman Disease Collaborative Network (CDCN) classified MCD into distinct clinic-pathological entities, which are either human herpesvirus-8–associated or idiopathic in nature, whereas a form of MCD associated with POEMS (polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes) syndrome has also been recognized.2 Next, the first formal consensus diagnostic criteria for iMCD were published, which helps the physician to distinguish iMCD from a variety of other disorders and permits a confident and accurate diagnosis.3 iMCD spans a wide clinical spectrum with some patients being mildly afflicted, whereas others have a life-threatening course. Choosing the correct therapy can therefore be challenging, especially because a myriad of agents are reported to have efficacy in iMCD. The lack of uniformity in therapy prompted the CDCN to publish treatment guidelines based on the severity of the iMCD. Recommendations included therapeutic intervention with mAbs targeting the IL-6 signaling cascade, including siltuximab and tocilizumab, with the anti-CD20 mAb rituximab as an alternative for milder disease. The consensus criteria note that combination chemotherapy is reserved for those with severe and unresponsive disease.4 The most comprehensive dataset exists for the IL-6 neutralizing mAb, siltuximab, which is presently approved for iMCD in the United States and the European Union. Siltuximab has been studied in a phase 1 study, a randomized placebo-controlled phase 2 trial, and a long-term safety study.5,6 Treatment with anti–IL-6 mAb is not curative and is in principle life long because relapses have been reported on cessation of therapy. Anti–IL-6 mAb therapy is also expensive and is not available in all parts of the world.
It is in this context that the study by Zhang et al is especially welcome and comprises an important contribution to the field by offering an all-oral and less cost-prohibitive treatment option in areas of the world where access to anti–IL-6 mAb is more limited. The individual components of the TCP regimen, thalidomide, prednisone, and cyclophosphamide, used by Zhang et al in this single-center phase 2 study of 25 patients, have all been reported to have efficacy in iMCD (see figure). Thalidomide is well known for its immunomodulatory properties and inhibits the production of cytokines, such IL-6, as well as vascular endothelial growth factor and tumor necrosis factor-α. Case reports have documented activity in iMCD, including tocilizumab-refractory disease. Cyclophosphamide has been used as part of combination chemotherapy regimens, such as R-CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone, plus rituximab), has antimitotic properties, and modulates T-cell function. Prednisone and other corticosteroids induce responses when used as monotherapy, but relapses are frequent on tapering doses.7 Zhang et al combined all 3 drugs in the present study, which produced responses in nearly half of the subjects (48%) with shrinkage in lymphadenopathy and significant improvement in iMCD-related symptomatology using objective response criteria very similar to those used in the randomized siltuximab study. This latter study found a response rate of 34%, with 59% of patients staying on drug at the time of analysis. The 1-year overall (OS) and progression-free survival (PFS) were 88% and 60%, respectively, in the study by Zhang et al; this outcome is promising and parallels the findings of the randomized siltuximab trial, which reported an OS of 100% and PFS of 60%.
Despite these encouraging results, it is also appropriate to mention that TCP therapy was delivered for a significant period of time: thalidomide and cyclophosphamide were administered for 2 and 1 year each, whereas prednisone was given either for 2 years or until treatment failure. The median follow-up was 14 months with the responders being followed for at least 24 weeks. It is therefore not clear how durable the responses will be, especially when off therapy. The present study is the first clinical trial in iMCD that does not specifically target IL-6, but uses agents with a broader range of action. It has become clear that IL-6 is not the main driver of iMCD in all patients as is exemplified by the siltuximab data. This notion is complemented by recent proteomic findings, which reported elevation of a large number of chemokines and cytokines, including CXCL13.8 Other studies suggest that beneficiaries of siltuximab exhibit a marked inflammatory syndrome and abnormal laboratory markers indicated by increased immunoglobulin levels, anemia, hypoalbuminemia, and elevated C-reactive protein. This is supported by analysis of the proteome of iMCD patients showing that these responders fall into a distinct cluster.9,10 The present study raises the hope that the TCP regimen may prove to have efficacy beyond the population of iMCD patients with IL-6–driven disease. Future studies will have to address the question of whether TCP is a good therapeutic alternative for siltuximab failures, especially for patients with more severe disease or for those with a very mild clinical phenotype who are unlikely to respond to siltuximab.
It is exciting to see a widely available, new treatment option for iMCD emerge; however, many questions remain. These questions especially center around the as-yet poorly understood pathogenesis of this rare and complex disorder. Ultimately, a thorough understanding of the disease is needed to develop more effective and better-targeted therapies for all iMCD patients.
Conflict-of-interest disclosure: The authors declare no competing financial interests.