Abstract
Hodgkin lymphoma is considered a prime example of treatment success, with cure rates exceeding 80% using modern combined modality therapies. However, especially in adolescents and young adults, treatment-related toxicity and long-term morbidity still represent persistent challenges. Moreover, outcomes in patients with relapsed or refractory disease remain unfavorable in the era of high-dose chemotherapy and stem-cell transplantation. Hence, there is a high demand for novel and innovative alternative treatment approaches. In recent years, many new therapeutic agents have emerged from preclinical and clinical studies that target molecular hallmarks of Hodgkin lymphoma, including the aberrant phenotype of the tumor cells, deregulated oncogenic pathways, and immune escape. The antibody-drug conjugate brentuximab vedotin and immune checkpoint inhibitors have already shown great success in patients with relapsed/refractory disease, leading to US Food and Drug Administration approval and new trials testing these agents in various clinical settings. The expanding knowledge and understanding of Hodgkin lymphoma biology and disease progression, as well as the development of robust tools for biomarker-driven risk stratification and therapeutic decision making, continue to be fundamentally important for the success of these and other novel agents. We anticipate that the availability and clinical implementation of novel molecular assays will be instrumental in an era of rapid shifts in the treatment landscape of this disease. Here, we review the current knowledge of Hodgkin lymphoma pathobiology, highlighting the related development of novel treatment strategies and prognostic models that hold the promise to continually challenge and change the current standard of care in classical Hodgkin lymphoma.
Introduction
Classical Hodgkin lymphoma (cHL) accounts for 15% to 25% of all lymphomas1 and represents the most common lymphoma subtype in children and young adults in the Western world. Among lymphoid malignancies, cHL stands out because of its striking histomorphological appearance, the peculiar phenotypic features of the malignant cells, and the abundance of a predominant immune cell infiltrate. Pathological diagnosis of cHL requires the presence of characteristic tumor cells, termed Hodgkin and Reed-Sternberg (HRS) cells, which are outnumbered by reactive cells in the tumor microenvironment (TME), including T and B lymphocytes, eosinophils, macrophages, mast cells, plasma cells, and stromal cells.2 The cell of origin had been enigmatic for a long time after the disease was first described by Thomas Hodgkin 185 years ago,3 but it is today unequivocally considered to be a postgerminal center B cell with only few exceptions.4 Advancements in molecular techniques, in conjunction with various enrichment strategies such as laser microdissection and fluorescence-activated cell sorting, have contributed to the discovery of crucial pathogenic concepts, characteristic genetic lesions, pathway dependencies, and immune escape mechanisms. However, the next challenge in the field is to translate and implement this knowledge in the clinic by providing the rationale for selecting new therapeutic targets and developing innovative treatment concepts that affect patient management. Anthracycline-based chemotherapy regimens with or without radiation therapy are still the mainstay for patients with cHL and result in remarkably high cure rates, particularly in patients with low-risk or early-stage disease.5 However, patients with advanced-stage or high-risk disease are only cured in ∼70% of cases, and high-dose chemotherapy in combination with autologous stem-cell transplantation (ASCT) is successful in only half of patients with relapsed/refractory cHL,6 necessitating alternative treatment options and better risk stratification for the subsets of patients for whom first- or second-line therapies fail. It is conceivable that the most promising strategy in future clinical trials will be the testing of novel therapeutic concepts in conjunction with predictive biomarkers that are comprehensively informed by and based on underlying tumor pathobiology.7
Many excellent reviews have recently captured pathogenic concepts of cHL in great detail.8-10 Here, we will focus on directly or indirectly targetable pathobiology and highlight novel therapeutic approaches that interfere with the aberrant phenotype of HRS cells and intrinsic oncogenic pathways or that target the TME and tumor-host interface. Moreover, we will review the emerging literature aimed at the development of prognostic and predictive biomarker tools that are largely based on the comprehensive assessment of genetic driver alterations and/or the composition of the TME.
Targeting the aberrant immunophenotype of HRS cells
Histologically, cHL is characterized by a relatively low abundance of malignant cells in a quantitatively dominant environment of reactive immune cells.2 One reason for the longstanding ambiguity about the cellular origin of cHL is the nearly complete loss of classic B lineage markers in HRS cells11 and aberrant expression of antigens normally associated with T cells, myeloid cells, or dendritic cells.12-14
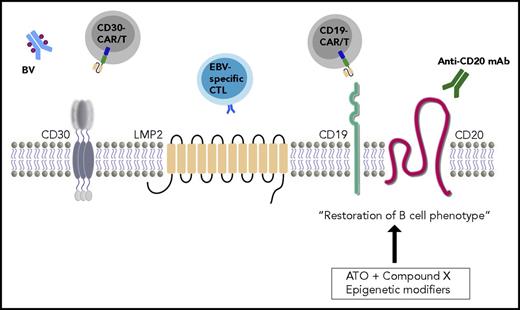
The characteristic immunophenotype of HRS cells is strongly positive for CD3015 and IRF4.2,16 CD15 shows a more variable expression pattern, but is positive in ∼75% of cases.17 In contrast, the tumor cells typically lack consistent expression of classic B-cell surface markers, such as CD20 and CD79a,18 as well as the B-cell transcription factors Oct-2, BOB.1, and PU.1,19-21 with PAX5 representing the only B cell–associated antigen that is expressed in the vast majority of cases.2,22 The widespread loss of the B-cell phenotype can be attributed to various mechanisms, which are likely to act synergistically. In addition to promoter hypermethylation, epigenetic silencing of key regulators of the B-cell program and aberrant expression patterns of polycomb group proteins23,24 have been described, and upregulation of transcriptional antagonists, such as ID2 and NOTCH1,25,26 further contributes to an altered expression of crucial B-cell transcription factors. These findings provide a rationale for treatment strategies that interfere with the epigenetic program,27 such as mocetinostat, panobinostat, and vorinostat, although these agents are also believed to have antiproliferative and immunmodulatory effects.28-30 A novel and innovative strategy was recently proposed by Du et al,31 who explored restoration of the B-cell phenotype as a therapeutic avenue in cHL. By combining a pharmacological compound screen with a CD19 reporter construct, they identified a number of molecules that were able to restore CD19 expression, likely through interference with epigenetic regulators and histone modifiers. Moreover, in combination with arsenic trioxide, reexpression of CD20 was achieved, which is widely targeted in non-Hodgkin lymphomas by monoclonal antibodies, such as rituximab or obinutuzumab.32 The use of arsenic trioxide as a sensitizer in combination with anti-CD20 antibodies or other small compounds, such as idelalisib and ibrutinib, showed encouraging antitumor activity in this proof-of-concept in vitro study.31 In addition, CD19 has emerged as a promising target for treatment of B-cell malignancies with engineered T cells expressing CD19-directed chimeric antigen receptors (CARs)33 or bispecific antibodies, such as blinatumomab (bispecific CD3/CD19 T-cell engager),34 and such concepts could be transferred to cHL if restoration of the B-cell phenotype can indeed be achieved in patients. Additional studies are needed to explore the efficaciousness in in vivo models and ultimately in the clinical setting, because the question remains whether therapeutic benefits can be overshadowed by adverse effects on the normal B-cell pool.35
The strong expression of CD30 on the tumor cell surface36 in conjunction with infrequent expression in nonmalignant immune cells represents an attractive therapeutic target (Figure 1). The antibody-drug conjugate BV is a recombinant chimeric immunoglobulin G1 monoclonal antibody covalently linked to monomethyl auristatin E, an antimicrotubule agent. Upon antibody binding, the drug is internalized and results in apoptosis of the tumor cells.37 Since the initially promising results in patients with relapsed/refractory disease that led to US Food and Drug Administration (FDA) approval in this indication,38-40 BV has been used in a variety of different second-line treatment settings, as part of salvage regimens, or as consolidation after ASCT in high-risk patients.41-43 Recent efforts have been made to move BV into frontline treatment as a substitution for bleomycin in the ABVD (doxorubicin, bleomycin, vinblastine, dacarbazine) schema.44,45 The large international randomized ECHELON-1 trial set out to compare AVD-BV with ABVD and met the primary end point of a statistically significant improvement in modified progression-free survival versus the control arm.46 CD30 has also been explored as a target antigen for CAR T cells, which are patient-derived CTLs that are ex vivo equipped with engineered receptor molecules consisting of a single-chain variable fragment fused to the signaling components of the T-cell receptor and costimulatory activation domains.47 The number of patients with cHL included in reported CAR T-cell trials is still low, but given the first results in heavily pretreated patients, with 2 complete remissions (CRs; 8%), 30% of patients achieving partial responses, and 35% achieving stable disease, future studies exploring this treatment approach seem warranted.48,49 Furthermore, CAR T cells have the advantage of recognizing surface antigens independent of the major histocompatibility complex (MHC)–based antigen processing/presenting machinery. This is of particular importance in cHL because HRS cells lack surface MHC class I and II molecules in a large proportion of cases.50-52 The most recent study, evaluating >360 cases of cHL, demonstrated MHC class I and II expression loss in 64% and 41%, respectively, with 30% of cases being negative for both.51 Of importance, Nijland et al51 added substantially to our knowledge of MHC class II deficiency by showing that in ∼50% of MHC class II–expressing cases, antigen presentation is hampered by lack of HLA-DM, an MHC class II chaperone responsible for the removal of CLIP from the antigen binding pocket. In total, 88% of cHL tumors harbor an altered expression of MHC class I, MHC class II, and/or HLA-DM, which may also have implications for immune checkpoint inhibition.
Schematic presentation of phenotypic features targetable by novel therapeutic agents. The HRS cell characteristic cell-surface antigen CD30 represents an attractive target for antibody-drug conjugates, such as brentuximab vedotin (BV), or for cellular-based therapies, such as CAR T cells. In Epstein-Barr virus (EBV)–positive cases, latent membrane protein 2 (LMP-2) is recognized by patient-derived cytotoxic T lymphocytes (CTLs), which are isolated and expanded ex vivo before reinfusion into the patient. Novel concepts aim at restoration of the B-cell phenotype by epigenetic modification of silenced B cell–related genes and/or transcription factors. For example, reexpressed CD19 and CD20 can then be targeted by monoclonal antibodies (mAbs) or CAR T cells, similar to B-cell non-HLs. ATO, arsenic trioxide.
Schematic presentation of phenotypic features targetable by novel therapeutic agents. The HRS cell characteristic cell-surface antigen CD30 represents an attractive target for antibody-drug conjugates, such as brentuximab vedotin (BV), or for cellular-based therapies, such as CAR T cells. In Epstein-Barr virus (EBV)–positive cases, latent membrane protein 2 (LMP-2) is recognized by patient-derived cytotoxic T lymphocytes (CTLs), which are isolated and expanded ex vivo before reinfusion into the patient. Novel concepts aim at restoration of the B-cell phenotype by epigenetic modification of silenced B cell–related genes and/or transcription factors. For example, reexpressed CD19 and CD20 can then be targeted by monoclonal antibodies (mAbs) or CAR T cells, similar to B-cell non-HLs. ATO, arsenic trioxide.
In ∼40% of cases, cHL is EBV associated, and numbers tend to be higher in developing countries and in patients with primary or secondary immunodeficiencies.53 Viral gene expression in EBV+ cHL follows the latency type II pattern, with positivity for EBER, LMP-1, LMP-2, and EBNA1.1 The idea of using these antigens as therapeutic targets was suggested almost 20 years ago, when EBV-specific CTL lines were expanded and infused in patients with relapsed disease.54 In subsequent studies, CTLs were reactivated and expanded ex vivo using autologous dendritic cells or EBV-transformed B-cell lines, resulting in a 100-fold increase in the frequency of LMP-specific CTLs, a high rate of complete responses (11 of 21 patients with relapsed/refractory disease), and sustained remission.55,56 This therapeutic concept can also be employed in patients with EBV− cHL, because other potential targets, such as MAGE4A,57 survivin,58 and PRAME,59 have been identified and explored.60,61 Given the logistical challenges and costs associated with cellular immunotherapies and the success of conventional agents, such as BV and immune checkpoint inhibitors, it remains to be seen if and how cell-based immunotherapy concepts will be firmly implemented in cHL care.
Interference with pathway dependencies
Constitutive activation of the nuclear factor κB (NF-κB) and Janus kinase–signal transducer and activator of transcription (JAK-STAT) signaling pathways is a long-recognized molecular hallmark of HRS cells. A large number of studies have provided evidence that various mechanisms, including gene mutations, structural/numerical chromosomal alterations, and signaling cascades via surface receptor–ligand interaction, converge and lead to exuberant activation of these oncogenic pathways (Table 1).8 In addition, expression of LMP-1 is thought to contribute to the activation of the NF-κB and JAK-STAT pathways, because LMP-1 aggregates and interacts with TRAF molecules in a fashion similar to that of tumor necrosis factor receptors (TNFRs), thereby mimicking TNFR signaling independent of external stimuli.62
Reported frequencies of genetic alterations in major hallmarks of cHL pathobiology
| Pathway/gene . | Genomic alteration . | Frequency, % . | Reference . |
|---|---|---|---|
| NF-κB | |||
| NFKBIA | SNV | 25-40 | 68,69 |
| NFKBIE | SNV | 17-27 | 70,71 |
| REL | CNV gain/amp | 28-70 | 63,65,66 |
| MAP3K14 | CNV gain/amp | 25 | 66 |
| TNFAIP3 | SNV | 40-45 | 72,73,140 |
| CNV loss | 21-60 | 65,66,74 | |
| BCL3 | CNV gain | 15-70 | 65,-67 |
| SR | 10 | 67 | |
| JAK-STAT | |||
| JAK2 | CNV gain/amp | 35-40 | 66,75,76 |
| SOCS1 | SNV | 41 | 77 |
| PTPN1 | SNV | 20 | 78 |
| STAT6 | SNV | 31-45 | 84,140 |
| Immune escape | |||
| CIITA | SR | 15 | 141 |
| CD274/PDC1LG2 | CNV gain/amp | 38-75 | 76,99 |
| B2M | SNV | 21-70 | 50,140 |
| CD58 | CNV loss | 23 | 142 |
| TNFRSF14 | CNV loss | 13-42 | 66,117 |
| Pathway/gene . | Genomic alteration . | Frequency, % . | Reference . |
|---|---|---|---|
| NF-κB | |||
| NFKBIA | SNV | 25-40 | 68,69 |
| NFKBIE | SNV | 17-27 | 70,71 |
| REL | CNV gain/amp | 28-70 | 63,65,66 |
| MAP3K14 | CNV gain/amp | 25 | 66 |
| TNFAIP3 | SNV | 40-45 | 72,73,140 |
| CNV loss | 21-60 | 65,66,74 | |
| BCL3 | CNV gain | 15-70 | 65,-67 |
| SR | 10 | 67 | |
| JAK-STAT | |||
| JAK2 | CNV gain/amp | 35-40 | 66,75,76 |
| SOCS1 | SNV | 41 | 77 |
| PTPN1 | SNV | 20 | 78 |
| STAT6 | SNV | 31-45 | 84,140 |
| Immune escape | |||
| CIITA | SR | 15 | 141 |
| CD274/PDC1LG2 | CNV gain/amp | 38-75 | 76,99 |
| B2M | SNV | 21-70 | 50,140 |
| CD58 | CNV loss | 23 | 142 |
| TNFRSF14 | CNV loss | 13-42 | 66,117 |
amp, amplification; CNV, copy number variation; SNV, single-nucleotide variants (including small deletions); SR, structural rearrangement.
Several genetic alterations cause aberrant activation of the canonical and noncanonical NF-κB pathway. Genomic gains/amplifications of REL have been described in ∼70% of cHL cases, causing protein overexpression.63-66 Similarly, the BCL3 and MAP3K14 gene loci have been shown to be affected by chromosomal gains and structural rearrangements, resulting in increased NF-κB activity.66,67 Mutations in negative regulators constitute a second important mechanism of pathway activation. NFKBIA, encoding IκBα, an inhibitor that binds NF-κB factors and prevents their nuclear translocation, is mutated in ∼20% of cases.68,69 Furthermore, deletions and missense mutations affecting NFKBIE have been found in close to 30%.70,71 TNFAIP3 (encoding A20) functions as a posttranslational modifier of NF-κB pathway members. Deletions and somatic mutations of this tumor suppressor have been described in cHL with a higher frequency in EBV− cases.72-74 Moreover, HRS cells express several TNFR family members, leading to paracrine activation of NF-κB through binding of ligands expressed by cells in the TME.8
Activation of the JAK-STAT pathway is mainly attributed to numerical aberrations (ie, gain/amplification of the JAK2 locus or the 9p24.1 amplicon)75,76 and inactivating mutations in negative regulators, such as SOCS1 and PTPN1.77,78 Recently, novel splice variants of PTPN1 have been described and characterized as being functionally inactive.79 Activation of the pathway results in increased phosphorylation of STATs (mainly STAT5A/B and STAT6) and subsequently an increased transcription of downstream targets,77,80 one of which (BATF3) has been linked to activation of MYC.81 Auto- and paracrine signaling, such as expression of interleukin-13 (IL-13) or IL-21 and their respective receptors, further contributes to the constitutive activation of the JAK-STAT pathway,82,83 and recently, activating mutations in the DNA-binding domain of STAT6 have been described in a whole-exome sequencing study of microdissected HRS cells from 36 patients.84 This provides a strong rationale for targeting this pathway, and in particular, several JAK inhibitors, such as pacritinib and ruxolitinib, have been or are currently being evaluated in clinical studies.85,86 However, response rates in patients with a history of relapsed/refractory disease were rather disappointing, with only a small number showing a response or achieving partial remission status.
Among the common downstream targets of the JAK-STAT and NF-κB pathways are PIM serine/threonine kinases, which have been shown to be highly expressed in cHL cell lines and primary HRS cells.87 Targeting of PIM kinases with a pan-PIM inhibitor resulted in tumor cell apoptosis, attenuated JAK-STAT and NF-κB signaling, and marked reduction of immunomodulatory molecules, such as galectin-1 and programmed death receptor ligands 1 and 2 (PD-L1/2), in the preclinical setting.87
Besides JAK-STAT and NF-κB, multiple additional signaling cascades are deregulated and constitutively active in HRS cells, including the PI3K-AKT pathway.88 HRS cells also show aberrant expression of multiple receptor tyrosine kinases, including platelet-derived growth factor receptor-α, epithelial discoidin domain-containing receptor 2, TRKA, and TRKB,89 which are reported to result in downstream phosphorylation and activation of AKT1. PI3K/AKT/mammalian target of rapamycin pathway activation provides many opportunities for targeted pathway interference, and AKT inhibitors, as single agents or in combination, have been used in patients with relapsed/refractory cHL.90,91 Similarly, the mammalian target of rapamycin inhibitor everolimus has been tested as monotherapy92 and in combination with panobinostat.93
A recent study reported protein expression of monoamine oxidase A (MAO A) in a large proportion of cHL cases (75%) compared to other B-cell malignancies or normal B cells.94 In vitro studies using MAO A inhibitors demonstrated impaired growth and reduced cell viability in HL cell lines. Although underlying mechanisms of MAO A upregulation and downstream effects of MAO A expression remain unclear, future preclinical and clinical studies testing MAO A inhibitors might be warranted.
Targeting the tumor-host interface
The cellular composition and functional properties of the TME in cHL can be perceived as the results of an extensive cross talk between tumor cells and immune cells, which is largely mediated by a large network of cyto- and chemokines.8 Exome sequencing studies performed on flow-sorted HRS cells have provided further evidence that the landscape of genetic alterations (eg, B2M mutations) can differ between histological subtypes.52 It is therefore tempting to assume that the pheno- and genotype of HRS cells influence the cross talk with the TME, as evidenced by the specific composition of the TME in EBV+ cases using gene expression profiling.95 Other TME-modulating variables include the overall status of the host immune system, age, and specific gene polymorphisms associated with immune response processes.96,97
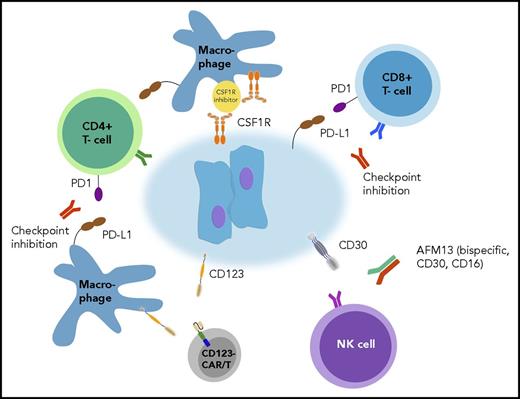
Despite the presence of reactive immune cells that comprise the majority of the tumor mass in cHL, there is no evidence of an effective immune response against the malignant HRS cells. A possible explanation is provided by the discovery that the tumor cells frequently express PD-L1 and PD-L2 through different mechanisms, including genomic gain/amplification of the 9p24.1 locus, EBV infection, and constitutive active JAK-STAT signaling.76,98-100 Current pathogenetic models assume that the interaction of PD-L1/2–expressing HRS cells with PD-1+ T cells leads to reduced T-cell activation, suppression of T-cell proliferation, and cytokine production101,102 and that this pathway plays an important role in shaping the cHL microenvironment.103 Of note, in the majority of cases, the PD-L1 “load” is relatively high, because PD-L1 is also expressed by tumor-associated macrophages (TAMs), providing a potential explanation for the poor prognosis of patients with a high number of TAMs in their tumor biopsies. A recent study using multiplex immunofluorescence in conjunction with topographical image analysis suggests that those macrophages form an immunoprotective niche (Figure 2).104,105 The seminal phase 1 trial using the PD-1 antibody nivolumab demonstrated high and durable responses in 23 heavily pretreated patients with relapsed/refractory disease, providing convincing evidence that immune checkpoint blockade is an effective treatment approach in cHL.106 The following phase 2 trial107 showed congruent, encouraging results and led to FDA approval of nivolumab for the treatment of patients with cHL for whom ASCT and BV failed. A second PD-1 inhibitor, pembrolizumab, exhibited similar effects and was also approved by the FDA for relapsed/refractory disease.108,109 The copy number (CN) status of the 9p24.1 locus was assessed in the phase 2 nivolumab trial, as described in the phase 1 study.106,107 A majority of, if not all, patients were classified as having 9p24.1 CN gains or amplifications, resulting in overexpression of PD-L1 on the tumor cell surface. Although there was a suggestive linkage between magnitude of CN alteration and response to targeted therapy, the study was not powered to provide strong statistical evidence that 9p24.1 amplification can be used as a predictive biomarker. The KEYNOTE-087 trial showed additional data with regard to PD-L1 expression levels in both HRS cells and TAMs, and responses were also seen in patients with low-level or weak ligand expression.109
Targeting the tumor-host interface. HRS cells are surrounded by microenvironmental cells, providing a tumor-supportive niche. Novel therapeutic concepts aim at reversion of immunosuppressive features by targeting immune checkpoints on tumor-infiltrating T cells and tumor-associated macrophages as well as by specifically engaging natural killer (NK) cells. CSF1R, colony-stimulating factor 1 receptor.
Targeting the tumor-host interface. HRS cells are surrounded by microenvironmental cells, providing a tumor-supportive niche. Novel therapeutic concepts aim at reversion of immunosuppressive features by targeting immune checkpoints on tumor-infiltrating T cells and tumor-associated macrophages as well as by specifically engaging natural killer (NK) cells. CSF1R, colony-stimulating factor 1 receptor.
Another checkpoint molecule that has been therapeutically explored in cHL is CTLA4, which competes with CD28 for binding of CD80 and CD86, thereby antagonizing T-cell activation.101 The literature on reported clinical trial data is sparse,110 because CTLA4 antibodies have been surpassed by PD-1/PD-L inhibitors, but they may prove useful in combination therapies with other agents.7
The paucity of the tumor cells in conjunction with the abundance of an immunosuppressive TME represents a challenge for immunotherapeutic approaches and has led to the idea of employing approaches that simultaneously target the tumor and the host. Colony-stimulating factor 1 receptor has been reported to be overexpressed in HRS cells and linked to an increased number of TAMs.111,112 Subsequently, JNJ-40346527, a colony-stimulating factor 1 receptor inhibitor, has been evaluated in a phase 1/2 trial with 20 evaluable patients; 1 patient achieved a CR, and 55% exhibited SD, suggesting limited activity when used as a single agent in the relapsed/refractory setting.113 Earlier studies have used bispecific antibodies against CD30 and CD16A (AFM13) to specifically engage natural killer cells; however, overall response rates were rather low (12% to 23%), and no CR was achieved.114,115 CD123, a dendritic cell marker and part of the IL-3 receptor, is expressed on HRS cells in up to 60% of cases and also on TAMs and myeloid-derived suppressor cells.14 Ruella et al116 developed CD123 CAR T cells and demonstrated that these cells were capable of targeting not only HRS cells but also tumor-promoting, CD123-expressing macrophages, providing an opportunity to modify the immunosuppressive TME.
Recently, recurrent losses of TNFRSF14 (herpesvirus entry mediator [HVEM]) have been described in cHL,117 and previous studies in follicular lymphoma have provided evidence that loss of this receptor results not only in B-cell activation and proliferation but also in the induction of a tumor-supportive microenvironment. An elegant study conducted by Boice et al118 showed that delivery of the HVEM ectodomain (soluble HVEM protein) by CD19 CAR T cells restored the tumor-suppressive effects of TNFRSF14 in a xenograft mouse model and that CAR T cells could be employed as “micropharmacies.”
Biomarker-driven prognostication and risk stratification in cHL
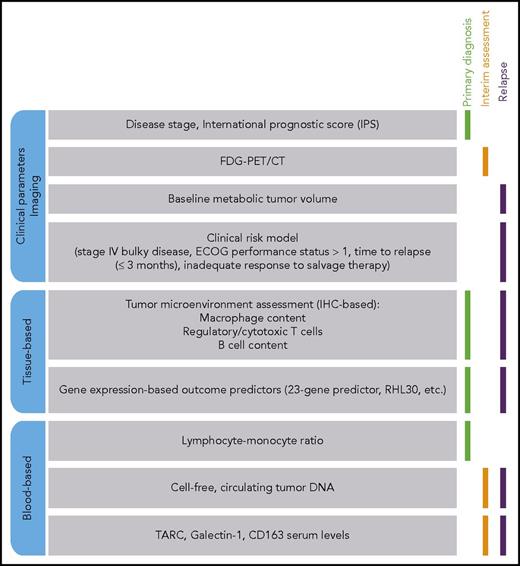
Therapeutic decision making in cHL currently relies mainly on disease stage (early/limited vs advanced) and absence or presence of risk factors, such as age, B symptoms, and extensive mediastinal tumor burden.119 The International Prognostic Score has been the gold standard for risk assessment in advanced-stage cHL for almost 2 decades and is used to identify patients at risk for recurrent disease.120 Over the last years, many clinical trials have firmly established the value of interim fluorodeoxyglucose positron emission tomography (PET)/computer tomography (CT) for interim response assessment and adaptation of patient management. However, all of these tools provide only limited information about the underlying lymphoma biology in individual patients.
The unique pathobiology of cHL offers an array of potential biomarkers, both tissue based and serum/blood based (Figure 3). Most studies investigating tissue-based biomarkers have focused on TME signatures and their association with treatment outcome, and the approaches used have ranged from single-marker IHC studies to transcriptome-wide gene expression studies. It needs to be emphasized that the relationship between TME constituents and outcome likely reflects the rather complex interaction between individual cellular elements in the TME, the tumor cells, and host immunity. Therefore, it is likely that IHC-based single biomarkers incompletely describe the complex pathobiology and capture only limited prognostic and predictive information, providing a rationale for multifeature biomarker approaches. Moreover, with increasing evidence that tumor cells actively shape their microenvironment, in part through acquisition of genomic alterations121 and altered cytokine/chemokine networks,8,122 future studies must provide a more comprehensive link between genetic alterations and TME composition in cHL.
Landscape of emerging biomarkers in cHL. Established and emerging biomarkers in cHL are grouped according to the context in/from which they can be derived, and their utility in various clinical scenarios is indicated. ECOG, Eastern Cooperative Oncology Group; FDG, fluorodeoxyglucose; IHC, immunohistochemistry.
Landscape of emerging biomarkers in cHL. Established and emerging biomarkers in cHL are grouped according to the context in/from which they can be derived, and their utility in various clinical scenarios is indicated. ECOG, Eastern Cooperative Oncology Group; FDG, fluorodeoxyglucose; IHC, immunohistochemistry.
The development of technologies that allow robust gene expression profiling from archival formalin-fixed, paraffin-embedded tissue has significantly advanced the field and led to the creation of gene expression–based prognostic models.123-126 Because of the paucity of HRS cells, gene expression profiles derived from whole-tissue sections largely reflect the cellular composition of the TME,104,123-125 whereas only a few studies have investigated the gene expression profiling of isolated tumor cells.112,127 From most of these studies, macrophages emerged as the most promising and potent cellular compartment104,125 to predict treatment outcomes in cHL, a concept that was proposed >30 years ago.128 Many subsequent studies used IHC to investigate the association of macrophage content with outcome across ethnicities, treatment concepts, and a range of different end points.129 Although a vast majority confirmed the association of high macrophage content with worse prognosis, there are also a handful of studies that did not report this relationship.129 Of note, the prognostic properties of macrophage content were also evaluated in the relapse/refractory setting, where a high number of macrophages in relapse biopsies was associated with inferior post-ASCT survival.126,130
To integrate prognostic information from a multitude of different cell types and individual genes, a number of groups have developed prognostic models using quantitative reverse transcription polymerase chain reaction assays or digital gene expression platforms in cohorts of adult patients with cHL. However, early studies in childhood and adolescent/young adult cHL indicate that the 23-gene predictor developed by Scott et al123 is not predictive of poor outcome in this patient population,131 supporting the concept that cHL, despite similar morphology, represents different biology across the age spectrum. Preliminary results further suggest that the robustness of such predictors is in question when being applied to cohorts exposed to different treatment strategies, such as BEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, prednisone) or response-adapted therapies.132,133
Patients with relapsed/refractory disease for whom initial therapy fails have a comparably guarded prognosis. Using standard-of-care salvage regimens and high-dose chemotherapy followed by ASCT, a substantial number of patients still relapse and die as a result of their disease even with BV consolidation therapy.43 However, the landscape of robust prognostic and predictive biomarkers available at the time point of relapse is sparse. Importantly, with emerging treatment alternatives in this setting (such as BV or checkpoint inhibitors), the development of relapse biomarkers and related clinical assays seems to be an attractive objective to guide treatment decisions. Specifically, a multinational study evaluated clinical risk factors in a cohort comprising >1000 patients. According to the developed and validated risk score, patients with stage IV and bulky disease, Eastern Cooperative Oncology Group performance status >1, short time to relapse (≤3 months), and inadequate response to salvage therapy were at highest risk for progression.134 In a small cohort of 65 patients enrolled in a phase 2 study of PET-adapted salvage therapy with BV and augmented ifosfamide, carboplatin, and etoposide, baseline metabolic tumor volume emerged as an independent prognostic factor for event-free survival.135 More recently, a gene expression–based predictor (RHL30) was developed using the biological information from tissue biopsies obtained at relapse to provide information on post-ASCT outcomes.126 This predictor is built on the rationale that in a proportion of cases, the biology at relapse, as measured by digital gene expression profiling, is substantially different from the biology at first diagnosis and that relapse biopsies are the superior specimens to predict post-ASCT survival. RHL30 identified a high-risk group of patients with significantly inferior post-ASCT failure-free survival (5-year failure-free survival: 23.8% high risk vs 77.5% low risk) as well as inferior post-ASCT overall survival (5-year overall survival: 28.7% high risk vs 85.4% low risk) compared with the low-risk group. Importantly, the prognostic power of RHL30 was reproduced in 2 separate cohorts and was statistically independent of previously described prognostic markers, including post–salvage therapy response assessment by PET/CT. Thus, RHL30 has the potential to identify patients at high risk of second-line treatment failure, for whom alternative strategies such as BV or checkpoint inhibitors should be considered. In a next step, the performance of RHL30 needs to be tested in the context of clinical trials incorporating PET/CT-guided response assessments and novel therapeutic agents.
Driven by considerations around feasibility and material access, the future of the biomarker field is also projected to rely on techniques that allow sensitive, specific, and reproducible assessment of predictive and response markers that capture disease dynamics during the course of lymphoma progression and treatment. Ideally, such dynamic biomarkers will allow determination of response to therapy and detection of minimal residual disease. Blood-based biomarkers are ideally suited to provide answers to those questions; for example, serum TARC, galectin-1, and CD163 have emerged as promising tools to assess interim response to chemotherapy in addition to PET.136,137 Moreover, detection of tumor-specific mutations or CN variations in cell-free circulating tumor DNA by next-generation sequencing techniques or digital droplet polymerase chain reaction have been shown to be feasible in patients with cHL and provide unique opportunities for real-time disease monitoring and quantitative assessment of minimal residual disease.138-140
Conclusion
Since the first description of Hodgkin disease, the recognition as a malignant neoplasm, and the discovery of the cell of origin, the landscape of described genetic alterations and aberrantly activated molecular pathways has continuously evolved, leading to a myriad of potential drugable targets in a disease with already encouraging cure rates. The recognition of the TME as an important contributor to the pathogenesis of cHL as well as its role in the development of treatment resistance phenotypes has paved the way for the implementation of therapeutic strategies targeting the tumor-host interface. Checkpoint inhibition has already generated significant benefits for patients with relapsed/refractory cHL, and deeper insights into microenvironment biology and clinical trials testing these drugs will likely lead to additional improvements in treatment outcomes. In addition, evaluation of novel agents in different clinical/therapeutic settings and in various combinations with conventional chemotherapy or other novel drugs will provide an expanded armamentarium of treatment concepts (Table 2).
Selection of ongoing phase 2/3 trials evaluating novel therapeutic approaches in cHL
| Target . | Agent/intervention . | Phase . | Clinical setting . | Trial identifier . |
|---|---|---|---|---|
| CD30 | BV + A(VR) | 2 | First line, AYAs | NCT02398240 |
| CD30 | BV + AD | 2 | First line, limited stage | NCT02505269 |
| CD30 | BV + AVD or ABVD | 2 | First line | NCT02292979 |
| CD30 | BV + AVD | 2 | First line, HIV+ | NCT02298257 |
| CD30 | BV consolidation after escBEACOPP | 2 | First line, PET+ after 2 cycles ABVD | NCT02298283 |
| CD30 | BV | 2 | First line, elderly | NCT01716806 |
| CD30 | BV | 2 | R/R, elderly | NCT02227433 |
| CD30 | BV + DHAP | 2 | R/R, second line | NCT02280993 |
| CD30 | AFM13 | 2 | R/R | NCT02321592 |
| CD30 + BTK | BV + ibrutinib | 2 | R/R, third line | NCT02744612 |
| CD30 | BV + bendamustine | 2 | R/R, third line | NCT01657331 |
| CD30/PD-1 | BV or pembrolizumab | 3 | Third line | NCT02684292 |
| CD30/PD-1 | BV and nivolumab vs BV | 3 | R/R or transplantation ineligible | NCT03138499 |
| CD30 | CAR T cells | 1/2 | R/R after ASCT | NCT02259556 |
| CD30 | CAR T cells | 1/2 | R/R | NCT02690545 |
| CD30 | CAR T cells | 1/2 | R/R | NCT02259556 |
| PD-1 | Nivolumab + AVD | 2 | First line, early stage, unfavorable | NCT03004833 |
| PD-1 + CD30 | Nivolumab + BV | 2 | First line, elderly | NCT02758717 |
| PD-1 + CD30 | Nivolumab + BV | 2 | R/R, AYAs | NCT02927769 |
| PD-1 + CD30 | Nivolumab + BV after ASCT | 2 | R/R | NCT03057795 |
| PD-1 + BTK | Nivolumab + ibrutinib | 2 | R/R | NCT02940301 |
| PD-1 | Pembrolizumab after ASCT | 2 | R/R, second line | NCT02362997 |
| PD-1 | Pembrolizumab + radiation therapy | 2 | Early stage, R/R | NCT03179917 |
| PD-1 | Pembrolizumab + ICE | 2 | R/R | NCT03077828 |
| PD-1 | BGB-A317 | 2 | R/R | NCT03209973 |
| PD-L1 | Atezolizumab | 2 | R/R | NCT03120676 |
| JAK | Ruxolitinib | 2 | R/R | NCT02164500 |
| BTK | Ibrutinib | 2 | R/R | NCT02824029 |
| BTK | Ibrutinib | 2 | R/R, after ASCT | NCT02869633 |
| EBV (LMP) | Allogeneic SCT + donor-derived CTL | 2 | R/R | NCT01636388 |
| EBV | CMD-003 | 2 | Second line | NCT02763254 |
| EBV, PD-1 | PD-1–ko EBV CTL | 1/2 | Advanced stage, EBV+ | NCT03044743 |
| Target . | Agent/intervention . | Phase . | Clinical setting . | Trial identifier . |
|---|---|---|---|---|
| CD30 | BV + A(VR) | 2 | First line, AYAs | NCT02398240 |
| CD30 | BV + AD | 2 | First line, limited stage | NCT02505269 |
| CD30 | BV + AVD or ABVD | 2 | First line | NCT02292979 |
| CD30 | BV + AVD | 2 | First line, HIV+ | NCT02298257 |
| CD30 | BV consolidation after escBEACOPP | 2 | First line, PET+ after 2 cycles ABVD | NCT02298283 |
| CD30 | BV | 2 | First line, elderly | NCT01716806 |
| CD30 | BV | 2 | R/R, elderly | NCT02227433 |
| CD30 | BV + DHAP | 2 | R/R, second line | NCT02280993 |
| CD30 | AFM13 | 2 | R/R | NCT02321592 |
| CD30 + BTK | BV + ibrutinib | 2 | R/R, third line | NCT02744612 |
| CD30 | BV + bendamustine | 2 | R/R, third line | NCT01657331 |
| CD30/PD-1 | BV or pembrolizumab | 3 | Third line | NCT02684292 |
| CD30/PD-1 | BV and nivolumab vs BV | 3 | R/R or transplantation ineligible | NCT03138499 |
| CD30 | CAR T cells | 1/2 | R/R after ASCT | NCT02259556 |
| CD30 | CAR T cells | 1/2 | R/R | NCT02690545 |
| CD30 | CAR T cells | 1/2 | R/R | NCT02259556 |
| PD-1 | Nivolumab + AVD | 2 | First line, early stage, unfavorable | NCT03004833 |
| PD-1 + CD30 | Nivolumab + BV | 2 | First line, elderly | NCT02758717 |
| PD-1 + CD30 | Nivolumab + BV | 2 | R/R, AYAs | NCT02927769 |
| PD-1 + CD30 | Nivolumab + BV after ASCT | 2 | R/R | NCT03057795 |
| PD-1 + BTK | Nivolumab + ibrutinib | 2 | R/R | NCT02940301 |
| PD-1 | Pembrolizumab after ASCT | 2 | R/R, second line | NCT02362997 |
| PD-1 | Pembrolizumab + radiation therapy | 2 | Early stage, R/R | NCT03179917 |
| PD-1 | Pembrolizumab + ICE | 2 | R/R | NCT03077828 |
| PD-1 | BGB-A317 | 2 | R/R | NCT03209973 |
| PD-L1 | Atezolizumab | 2 | R/R | NCT03120676 |
| JAK | Ruxolitinib | 2 | R/R | NCT02164500 |
| BTK | Ibrutinib | 2 | R/R | NCT02824029 |
| BTK | Ibrutinib | 2 | R/R, after ASCT | NCT02869633 |
| EBV (LMP) | Allogeneic SCT + donor-derived CTL | 2 | R/R | NCT01636388 |
| EBV | CMD-003 | 2 | Second line | NCT02763254 |
| EBV, PD-1 | PD-1–ko EBV CTL | 1/2 | Advanced stage, EBV+ | NCT03044743 |
AYA, adolescent and young adult; BTK, Bruton tyrosine kinase; DHAP, dexamethasone, high-dose cytarabine, cisplatin; esc, escalated; ICE, ifosfamide, carboplatin, etoposide; ko, knockout; R/R, relapsed/refractory.
In light of the recent success of immunotherapies, many studies have focused on associations of TME composition and blood/serum-based biomarkers with patient outcomes. The underlying biology of these relationships is only in part understood, and importantly, despite the demonstrated outcome associations, no biomarker has yet penetrated clinical practice to guide treatment strategy selection. In particular, the paucity of biomarker considerations is most evident for specific treatment groups with the greatest need for outcome improvement, such as elderly patients and patients with acquired immunodeficiency. With the emergence and widespread use of novel compounds, integration of predictive biomarker testing into clinical trial designs is urgently needed to select the best approach for patients before commencement of therapy to avoid treatment failure and unnecessary toxicity.
Acknowledgments
This work was supported by fellowships from the Mildred Scheel Cancer Foundation, the Michael Smith Foundation for Health Research, and Lymphoma Canada (A.M.).
Authorship
Contribution: A.M. and C.S. reviewed the literature and wrote the paper.
Conflict-of-interest disclosure: C.S. has a consulting or advisory role with Affimed Therapeutics has provided expert testimony for Juno Therapeutics. A.M. declares no competing financial interests.
Correspondence: Christian Steidl, Department for Lymphoid Cancer Research, British Columbia Cancer Agency, 675 West 10th Ave, Vancouver, BC V5Z 1L3, Canada; e-mail: csteidl@bccancer.bc.ca.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal