Key Points
G-CSF-induced sympathetic tone provokes fever and modulates microenvironment via PGE2 production by bone marrow Gr-1high neutrophils.
Abstract
Granulocyte colony-stimulating factor (G-CSF) is widely used for peripheral blood stem/progenitor mobilization. G-CSF causes low-grade fever that is ameliorated by nonsteroidal anti-inflammatory drugs (NSAIDs), suggesting the activation of arachidonic acid (AA) cascade. How G-CSF regulated this reaction was assessed. G-CSF treatment in mice resulted in fever, which was canceled in prostaglandin E synthase (mPGES-1)-deficient mice. Mobilization efficiency was twice as high in chimeric mice lacking mPGES-1, specifically in hematopoietic cells, suggesting that prostaglandin E2 (PGE2) from hematopoietic cells modulated the bone marrow (BM) microenvironment. Neutrophils from steady-state BM constitutively expressed mPGES-1 and significantly enhanced PGE2 production in vitro by β-adrenergic stimulation, but not by G-CSF, which was inhibited by an NSAID. Although neutrophils expressed all β-adrenergic receptors, only β3-agonist induced this phenomenon. Liquid chromatography–tandem mass spectrometry traced β-agonist-induced PGE2 synthesis from exogenous deuterium-labeled AA. Spontaneous PGE2 production was highly efficient in Gr-1high neutrophils among BM cells from G-CSF-treated mice. In addition to these in vitro data, the in vivo depletion of Gr-1high neutrophils disrupted G-CSF-induced fever. Furthermore, sympathetic denervation eliminated both neutrophil priming for PGE2 production and fever during G-CSF treatment. Thus, sympathetic tone-primed BM neutrophils were identified as one of the major PGE2 producers. PGE2 upregulated osteopontin, specifically in preosteoblasts, to retain progenitors in the BM via EP4 receptor. Thus, the sympathetic nervous system regulated neutrophils as an indispensable PGE2 source to modulate BM microenvironment and body temperature. This study provided a novel mechanistic insight into the communication of the nervous system, BM niche components, and hematopoietic cells.
Introduction
Granulocyte colony-stimulating factor (G-CSF) induces neutrophil expansion and is an indispensable supporting agent for myelosuppressive chemotherapy. G-CSF is also widely used for the mobilization of hematopoietic stem/progenitor cells (HSCs/HPCs) from the bone marrow (BM) to harvest the transplantable source via peripheral blood. Low-grade fever and back (bone) pain are relatively common complications of G-CSF treatment. In particular, in mobilization in which a high dose of G-CSF is administered for several consecutive days, a vast majority of healthy donors complain of these symptoms.1 Given the clinical experience that these G-CSF-associated symptoms are ameliorated by the usual dose of nonsteroidal anti-inflammatory drugs (NSAIDs), we speculated the activation of arachidonic acid (AA) cascade and enhanced production of prostaglandin E2 (PGE2) in the BM microenvironment on G-CSF stimulation.
The importance of PGE2 function in the BM has recently emerged. It is reported that PGE2 protects or expands the HSC/HPC pool.2-6 The inhibition of PGE2 degradation may support BM hematopoiesis by enhancing certain niche factors.7 In contrast, PGE2 is also known to have an anabolic effect by osteoblastic recruitment from BM stromal cells.8 Among the 4 PGE receptors (EP1-EP4), recent studies have revealed PGE2-mediated hematopoietic niche regulation via EP4.4,9 Thus, the action of PGE2 has been regarded as one of the key pathways to maintain the BM microenvironment.
Several cell types have been identified as PGE2 producers. It is well known that endotoxin/lipopolysaccharide (LPS) is a strong inducer of PGE2 from macrophages via Toll-like receptor 4.10 Mesenchymal stromal cells are reported to produce PGE2 for the modulation of macrophages to prevent organ damage in sepsis.11 It is also reported that PGE2 from a distinct monocyte/macrophage population that expresses α-smooth muscle actin prevents HSCs/HPCs from exhaustion by reactive oxygen species.12 However, despite these extensive investigations of PGE2 function, the regulatory mechanism of PGE2 production in the BM remains largely unclear.
BM is highly innervated with sympathetic nerves13 that regulate hematopoietic homeostasis.14 It has also been shown that G-CSF induces high sympathetic tone in the BM,15 mainly by inhibiting the reuptake of norepinephrine (NE) by nerve terminals on the stimulation of G-CSF receptor expressed on sympathetic neurons.16 Sympathetic denervation diminishes the reaction of mesenchymal lineage cells on G-CSF stimulation.15,17,18 Here, we have identified neutrophils as a major PGE2 source in the BM on G-CSF stimulation. We also found that G-CSF not only expanded BM neutrophils but also activated the AA cascade in these cells via the sympathetic nervous system (SNS).
Methods
Animals
mPGES-1−/− mice10 were backcrossed more than 9 generations into C57BL/6 background, and the experiments were carried out using littermates obtained by mating heterozygous breeding pairs. Wild-type (WT) C57BL/6 mice were purchased from CLEA Japan (Chiba, Japan) at 1 to 2 weeks before the experiments. C57BL/6-CD45.1 congenic mice were purchased from the Jackson Laboratory (Bar Harbor, ME). Because EP4−/− mice19 perished as a result of patent ductus arteriosus when fully backcrossed into C57BL/6 background, we used EP4+/− breeding pairs after backcrossing 2 generations into C57BL/6 from the original. All experiments with EP4−/− mice were performed in littermates. Generation of chimeric mice and measurement of body temperature are described in the supplemental Methods, available on the Blood Web site. Animals were maintained under specific pathogen-free conditions and on 12 hour light/12 hour darkness cycles, and used for experiments at 6 to 8 weeks of age. Only male mice were used for mobilization experiments. In vivo treatments for G-CSF-induced mobilization and its modulation by PGE28 and anti-osteopontin (OPN) antibody 35B6,20 sympathetic denervation by 6-hydroxydopamine (6OHDA), and neutrophil depletion by anti-Gr-1 antibody were performed as described in supplemental Methods. All animal studies were approved by the Animal Care and Use Committee of Kobe University.
Flow cytometry, cell sorting, cell culture, and evaluation of mRNA, protein, and lipid levels
A detailed description of these experiments is provided in supplemental Methods.
Statistical analysis
All data were pooled from at least 3 independent experiments. Histograms of flow cytometry, western blot, reverse transcription polymerase chain reaction (RT-PCR), and immunofluorescence staining were shown as representative data of 3 independent experiments that showed similar trends. All values were reported as mean ± standard error of the mean (mean ± SEM). Statistical analysis was conducted using unpaired 2-tailed Student t test, Mann-Whitney U test, and 1-way ANOVA test with Dunnett’s or Tukey’s post hoc procedure. Statistical significance was defined as P < .05.
Results
Hematopoietic cell-derived PGE2 modulated G-CSF-induced fever and mobilization
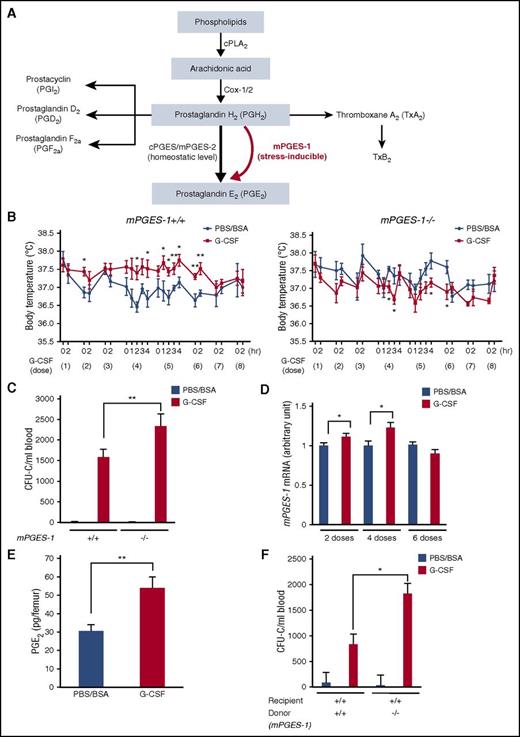
PGE2 synthesis is mediated by 3 catalytic enzymes: cytosolic PGE synthase (cPGES), microsomal PGE synthase-1 (mPGES-1), and microsomal PGE synthase-2 (mPGES-2). Both cPGES and mPGES-2 maintain the physiological level of PGE2, whereas mPGES-1 is inducible and functions to generate additional PGE2 in excess of the physiological level on various stress stimulations (Figure 1A).21 To assess whether PGE2 endogenously produced in response to G-CSF treatment affected body temperature and mobilization efficiency, we used mPGES-1−/− mice. No hematopoietic or skeletal phenotype has been reported in mPGES-1−/− mice, with the exception of the impaired fracture healing.22
mPGES-1-mediated PGE2production from hematopoietic cells modulates G-CSF-induced fever and mobilization. (A) Pathway of PGE2 synthesis. (B) Body temperature in mPGES-1+/+ and mPGES-1−/− mice during G-CSF treatment (n = 4-6). The x axes show the G-CSF dose (every 12 hours) and the timing to measure the body temperature after each dose of G-CSF. (C) CFU-Cs mobilized in mPGES-1+/+ and mPGES-1−/− mice (n = 8-10 for PBS/BSA group and n = 26-28 for G-CSF group). (D) qRT-PCR analysis of mPGES-1 mRNA in BM cells during G-CSF treatment (n = 9-10 per group). (E) PGE2 levels assessed by LC-MS/MS in whole BM (BM cells and extracellular fluids) at 2 hours after 4 doses of G-CSF (n = 8). (F) CFU-Cs mobilized in mPGES-1 chimeric mice (n = 3-5 for PBS/BSA group and n = 6 for G-CSF group). Data are represented as mean ± SEM. *P < .05; **P < .01.
mPGES-1-mediated PGE2production from hematopoietic cells modulates G-CSF-induced fever and mobilization. (A) Pathway of PGE2 synthesis. (B) Body temperature in mPGES-1+/+ and mPGES-1−/− mice during G-CSF treatment (n = 4-6). The x axes show the G-CSF dose (every 12 hours) and the timing to measure the body temperature after each dose of G-CSF. (C) CFU-Cs mobilized in mPGES-1+/+ and mPGES-1−/− mice (n = 8-10 for PBS/BSA group and n = 26-28 for G-CSF group). (D) qRT-PCR analysis of mPGES-1 mRNA in BM cells during G-CSF treatment (n = 9-10 per group). (E) PGE2 levels assessed by LC-MS/MS in whole BM (BM cells and extracellular fluids) at 2 hours after 4 doses of G-CSF (n = 8). (F) CFU-Cs mobilized in mPGES-1 chimeric mice (n = 3-5 for PBS/BSA group and n = 6 for G-CSF group). Data are represented as mean ± SEM. *P < .05; **P < .01.
G-CSF was administered at 125 μg/kg/dose every 12 hours for 8 doses.17 The increase of body temperature was mainly observed during the fourth to sixth doses of G-CSF in WT mice, but G-CSF was not effective in increasing or, rather, lowered, the body temperature in mPGES-1−/− littermates (Figure 1B). Furthermore, there was no increase of body temperature during G-CSF treatment in chimeric mice that lacked mPGES-1 only in hematopoietic cells, whereas chimeric mice that harbored mPGES-1 only in hematopoietic cells showed fever exactly as observed in the control mice that possessed mPGES-1 in both hematopoietic cells and microenvironment (supplemental Figure 1). This indicates that fever during G-CSF treatment is mediated by stress-induced PGE2, likely from hematopoietic cells.
The number of HPCs as assessed by colony-forming units in culture (CFU-Cs) and lineage−Sca-1+c-kit+ cells mobilized from the BM into the circulation was significantly higher in mPGES-1−/− mice compared with in WT littermates (Figure 1C; supplemental Figure 2A), whereas it was comparable in the BM (supplemental Figure 2B). Consistent with this, treatment of WT mice for 14 days with exogenous PGE2, a known protocol for induction of osteoblast increase,8 significantly suppressed HPC mobilization without alteration of the HPC number in the BM (supplemental Figure 2C-E). These results suggest that G-CSF induces supplementary production of PGE2, which leads to the suppression of mobilization.
In the early phase of G-CSF treatment (at the second and fourth doses of every-12-hours administration), the mRNA level of mPGES-1 was upregulated in BM cells, followed by its return to baseline after 6 doses (Figure 1D). Consistently, PGE2 level in whole BM at the fourth dose of G-CSF was assessed by liquid chromatography–tandem mass spectrometry (LC-MS/MS) and found to be significantly increased (Figure 1E). Cytosolic phospholipase A2 (cPLA2) mRNA showed an alteration similar to that of mPGES-1, and cyclooxygenase-2 (cox-2) mRNA tended to be upregulated as the number of G-CSF doses advanced, whereas nuclear factor-κ B (NF-κB; p50/p105) mRNA was downregulated at all points (supplemental Figure 2F). These results suggest that the AA cascade, including mPGES-1, is stimulated in BM cells during G-CSF treatment. Consistently, G-CSF-induced fever was mainly observed in the period between the fourth and sixth doses (Figure 1B). Furthermore, WT mice reconstituted with mPGES-1−/− BM displayed significantly greater mobilization than control mice reconstituted with mPGES-1+/+ BM (Figure 1F; supplemental Figure 2G).
These results indicate that hematopoietic cells are, at least partially, responsible for mPGES-1-mediated supplementary PGE2 synthesis by G-CSF stimulation, which causes fever and the subsequent suppression of mobilization.
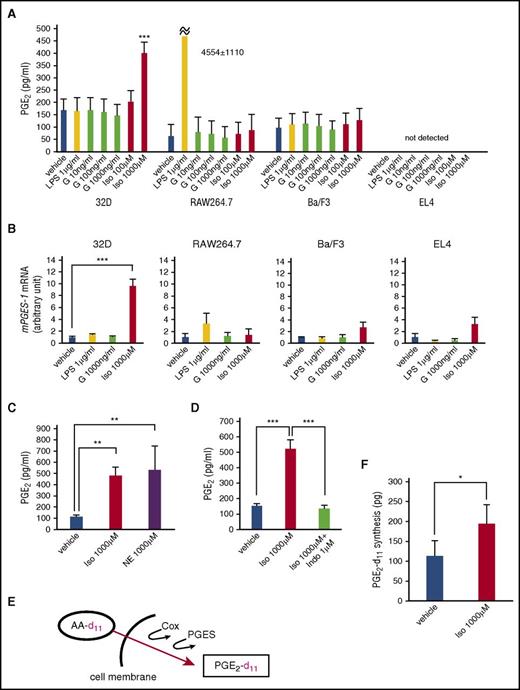
BM neutrophils produced PGE2 in vitro on stimulation by β-adrenergic signal, but not by G-CSF
Next, we tried to identify the producers of PGE2 among hematopoietic cells and the triggering signal for this activity. LPS is an inducer of PGE2 production from macrophages,10 but the BM microenvironment is aseptic during mobilization by G-CSF. It is also shown that G-CSF induces a high sympathetic tone in the BM microenvironment.15 Thus, we examined the in vitro production of PGE2 by stimulation with LPS, G-CSF, and isoproterenol, a known pan-β-adrenergic receptor (AR) agonist, in various hematopoietic cell lines, such as 32D (neutrophil precursor), RAW264.7 (monocyte/macrophage), Ba/F3 (B lymphoid), and EL4 (T lymphoid) (Figure 2A). At the mRNA level, G-CSF receptor was expressed in 32D, RAW264.7, and Ba/F3, but not in EL4, and all 4 cell lines expressed β2- and β3-ARs but not β1-AR (supplemental Figure 3). LPS induced drastic PGE2 production only in RAW264.7 cells. Importantly, no increase in PGE2 level was observed by stimulation with G-CSF in any cell line. Notably, isoproterenol significantly induced PGE2 production only in 32D neutrophil precursors, with a drastic increase in mPGES-1 mRNA (Figure 2A-B). In a like manner, NE displayed a similar effect in 32D cells (Figure 2C). PGE2 production enhanced by isoproterenol was completely blocked by an NSAID, indomethacin (Figure 2D). Enhanced PGE2 synthesis from exogenous substrate stimulated by isoproterenol in 32D cells was confirmed by the incorporation of deuterium-labeled AA (AA-d11) supplemented in the culture media into deuterium-PGE2 (PGE2-d11), as assessed by LC-MS/MS (Figure 2E-F). Collectively, our data suggest the possibility that neutrophils, a major cell population in G-CSF-treated BM, can be the candidate for PGE2 producer.
Neutrophil precursor cell line produces PGE2by β-adrenergic stimulation. (A) PGE2 levels in culture supernatants of hematopoietic cell lines (8 hours after stimulation with indicated reagents; n = 3-4). Vehicle: PBS. G, G-CSF; Iso, isoproterenol. (B) qRT-PCR analysis of mPGES-1 mRNA in cell lines in A (n = 3). (C, D) PGE2 levels in culture supernatants of 32D cells (8 hours after stimulation with indicated reagents; n = 3-4). NE, norepinephrine; Indo, indomethacin. (E) Schema of deuterium-labeled arachidonic acid (AA-d11) assay. (F) Deuterium-PGE2 (PGE2-d11) levels in 32D culture (n = 14). Data are represented as mean ± SEM. *P < .05; **P < .01; ***P < .001.
Neutrophil precursor cell line produces PGE2by β-adrenergic stimulation. (A) PGE2 levels in culture supernatants of hematopoietic cell lines (8 hours after stimulation with indicated reagents; n = 3-4). Vehicle: PBS. G, G-CSF; Iso, isoproterenol. (B) qRT-PCR analysis of mPGES-1 mRNA in cell lines in A (n = 3). (C, D) PGE2 levels in culture supernatants of 32D cells (8 hours after stimulation with indicated reagents; n = 3-4). NE, norepinephrine; Indo, indomethacin. (E) Schema of deuterium-labeled arachidonic acid (AA-d11) assay. (F) Deuterium-PGE2 (PGE2-d11) levels in 32D culture (n = 14). Data are represented as mean ± SEM. *P < .05; **P < .01; ***P < .001.
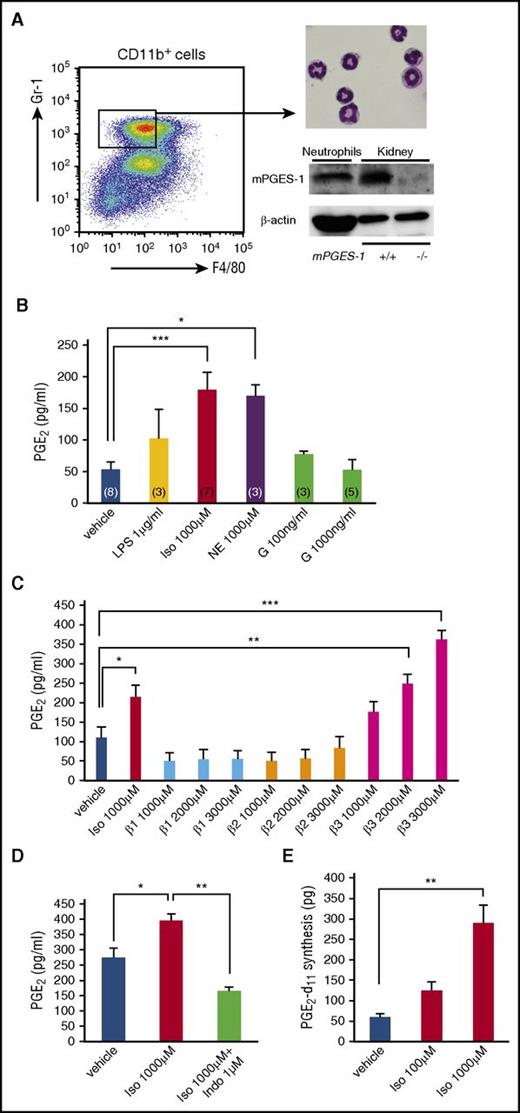
In correlation with these results, we next examined the β-adrenergic response in freshly isolated BM neutrophils. CD11b+F4/80dimGr-1high cells with segmented nuclei sorted from steady-state BM indeed constitutively possessed mPGES-1 protein (Figure 3A) and showed enhanced production of PGE2 in response to isoproterenol and NE, but not to G-CSF (Figure 3B). We confirmed that these cells expressed all 3 β-ARs at the protein and mRNA levels (supplemental Figure 4A-B). Among these 3 β-ARs, only the β3-AR signal promoted PGE2 production, whereas β1- and β2-AR signals showed no effect when stimulated with the selective agonist for each β-AR (Figure 3C). Isoproterenol-stimulated PGE2 production from neutrophils was clearly blocked by indomethacin (Figure 3D). This could not be attributed to cell death because dead cells assessed by 7-amino-actinomycin D staining were less than 5% in both vehicle- and isoproterenol-treated cells (data not shown). Furthermore, enhanced PGE2 synthesis from an exogenous substrate stimulated by isoproterenol was confirmed by the incorporation of AA-d11 supplemented in the culture media into PGE2-d11, as assessed by LC-MS/MS (Figure 3E). Cox-2 mRNA was upregulated over time in isoproterenol-stimulated BM neutrophils, whereas mPGES-1, cPLA2, and NF-κB mRNAs showed a slight, but not significant, increase, followed by a decrease when cox-2 mRNA was dramatically increased (supplemental Figure 4C).
BM neutrophils produce PGE2by β-adrenergic stimulation. (A) Dot-plot profile for BM neutrophil sorting, May-Giemsa staining of cytospin preparation, and protein expression of mPGES-1 in BM neutrophils by western blot. Control proteins were obtained from kidneys of mPGES-1+/+ and mPGES-1−/− mice. Loaded protein: neutrophils 100 μg and kidneys 15 μg/lane. (B) PGE2 levels in culture supernatants of BM neutrophils (4 h after stimulation with indicated reagents). Vehicle: PBS. Iso, isoproterenol; NE, norepinephrine; G, G-CSF. The number of each group is shown in each bar. (C) PGE2 levels in culture supernatants of BM neutrophils (4 hours after stimulation with indicated reagents). Vehicle: PBS. β1 agonist, dobutamine; β2 agonist, clenbuterol; and β3 agonist, BRL37344 (n = 5). (D) PGE2 levels in culture supernatants of BM neutrophils (4 hours after stimulation with indicated reagents; n = 3). Vehicle: PBS. Indo, indomethacin. (E) Deuterium-PGE2 (PGE2-d11) levels in neutrophil culture (n = 3). Data are represented as mean ± SEM. *P < .05; **P < .01; ***P < .001.
BM neutrophils produce PGE2by β-adrenergic stimulation. (A) Dot-plot profile for BM neutrophil sorting, May-Giemsa staining of cytospin preparation, and protein expression of mPGES-1 in BM neutrophils by western blot. Control proteins were obtained from kidneys of mPGES-1+/+ and mPGES-1−/− mice. Loaded protein: neutrophils 100 μg and kidneys 15 μg/lane. (B) PGE2 levels in culture supernatants of BM neutrophils (4 h after stimulation with indicated reagents). Vehicle: PBS. Iso, isoproterenol; NE, norepinephrine; G, G-CSF. The number of each group is shown in each bar. (C) PGE2 levels in culture supernatants of BM neutrophils (4 hours after stimulation with indicated reagents). Vehicle: PBS. β1 agonist, dobutamine; β2 agonist, clenbuterol; and β3 agonist, BRL37344 (n = 5). (D) PGE2 levels in culture supernatants of BM neutrophils (4 hours after stimulation with indicated reagents; n = 3). Vehicle: PBS. Indo, indomethacin. (E) Deuterium-PGE2 (PGE2-d11) levels in neutrophil culture (n = 3). Data are represented as mean ± SEM. *P < .05; **P < .01; ***P < .001.
Although mature neutrophils are the obvious major population in the BM, we also tested isoproterenol stimulation in other cells such as B220+ B cells and CD11b+F4/80highGr-1low monocytes/macrophages sorted from steady-state BM. PGE2 was not detected from primary B cells even after isoproterenol stimulation, whereas primary monocytes/macrophages showed an enhancement of PGE2 production by isoproterenol (supplemental Figure 4D-E). However, enhanced incorporation of AA-d11 by isoproterenol stimulation was not prominent in primary monocytes/macrophages (supplemental Figure 4F). Considering a substantial cell population of CD11b+F4/80dimGr-1high neutrophils compared with CD11b+F4/80highGr-1low monocytes/macrophages in the BM, these results suggest that BM Gr-1high neutrophils stimulated by β-adrenergic signals are the strong candidate as a major cell source for PGE2 during G-CSF treatment.
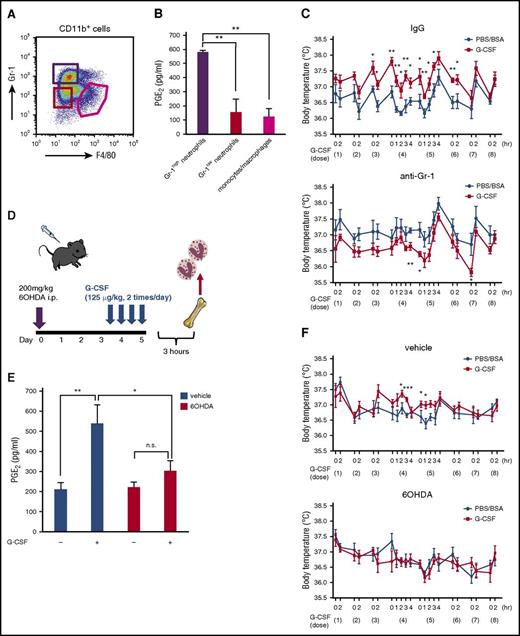
BM neutrophils were primed to produce PGE2 by the SNS during G-CSF treatment in vivo
After 4 doses of G-CSF administration when mPGES-1 mRNA was increased in BM cells (Figure 1D), CD11b+F4/80dimGr-1low neutrophils and CD11b+F4/80highGr-1low monocytes/macrophages showed a trend toward the expansion, and the number of CD11b+F4/80dimGr-1high neutrophils was unchanged in the BM (Figure 4A; supplemental Table 1). Among these fractions, F4/80dimGr-1high neutrophils were selectively primed to spontaneously produce a high amount of PGE2 (Figure 4B). A morphological study revealed that cells in all these fractions became larger by G-CSF, and Gr-1high neutrophils were hypersegmented (supplemental Figure 5). These results suggest that Gr-1high neutrophils after G-CSF treatment are highly activated to produce PGE2.
G-CSF-induced sympathetic tone provokes fever via PGE2production by neutrophils. (A) Dot-plot profile of G-CSF (4 doses)-primed BM CD11b+ cells. (B) PGE2 levels in culture supernatants of each fraction (Gr-1high neutrophils: CD11b+F4/80dimGr-1high, Gr-1low neutrophils: CD11b+F4/80dimGr-1low, monocytes/macrophages: CD11b+F4/80highGr-1low; 4-hour incubation with no stimulation; n = 3). (C) Body temperature during G-CSF treatment with or without neutrophil depletion by anti-Gr-1 antibody (1A8; n = 5). (D) Protocol for chemical denervation by 6OHDA followed by 4 doses of G-CSF. (E) PGE2 levels in culture supernatants of sorted BM neutrophils after 4 doses of G-CSF with or without chemical denervation by 6OHDA. Vehicle: 0.1% ascorbic acid (n = 7). (F) Body temperature during G-CSF treatment with or without chemical denervation by 6OHDA (n = 7). Data are represented as mean ± SEM. *P < .05; **P < .01; ***P < .001. n.s., not significant.
G-CSF-induced sympathetic tone provokes fever via PGE2production by neutrophils. (A) Dot-plot profile of G-CSF (4 doses)-primed BM CD11b+ cells. (B) PGE2 levels in culture supernatants of each fraction (Gr-1high neutrophils: CD11b+F4/80dimGr-1high, Gr-1low neutrophils: CD11b+F4/80dimGr-1low, monocytes/macrophages: CD11b+F4/80highGr-1low; 4-hour incubation with no stimulation; n = 3). (C) Body temperature during G-CSF treatment with or without neutrophil depletion by anti-Gr-1 antibody (1A8; n = 5). (D) Protocol for chemical denervation by 6OHDA followed by 4 doses of G-CSF. (E) PGE2 levels in culture supernatants of sorted BM neutrophils after 4 doses of G-CSF with or without chemical denervation by 6OHDA. Vehicle: 0.1% ascorbic acid (n = 7). (F) Body temperature during G-CSF treatment with or without chemical denervation by 6OHDA (n = 7). Data are represented as mean ± SEM. *P < .05; **P < .01; ***P < .001. n.s., not significant.
We also assessed the body temperature of mice after in vivo treatment with anti-Gr-1 antibody, which led to the depletion of Gr-1high neutrophils (supplemental Figures 6-9). Control mice displayed higher body temperature for a few hours after G-CSF administration, mainly at the fourth and fifth doses compared with the phosphate-buffered saline (PBS)/bovine serum albumin (BSA)-treated group; however, this alteration of body temperature induced by G-CSF disappeared in neutrophil-depleted mice (Figure 4C), which further confirmed that Gr-1high neutrophils were the regulator of body temperature during G-CSF treatment.
We evaluated next the contribution of the SNS to prime BM neutrophils in vivo. After chemical denervation of the SNS by the administration of 6OHDA, followed by 4 doses of G-CSF, CD11b+F4/80dimGr-1high neutrophils in the BM were sorted and examined for spontaneous PGE2 production (Figure 4D). As shown in Figure 4E, G-CSF primed PGE2 production in neutrophils in nondenervated mice, whereas SNS denervation did not alter the baseline level of PGE2 and clearly blocked the neutrophil priming effect of PGE2 production by G-CSF. We also assessed the body temperature of mice with or without denervation. Nondenervated mice displayed higher body temperature for a few hours after G-CSF administration at the fourth and fifth doses compared with the PBS/BSA-treated group; however, this alteration of body temperature induced by G-CSF disappeared in denervated mice (Figure 4F).
Collectively, our data indicate that G-CSF-induced high sympathetic tone stimulates BM Gr-1high neutrophils to produce PGE2 and modulates body temperature during G-CSF treatment.
Potential target of PGE2 in the BM microenvironment to modulate mobilization
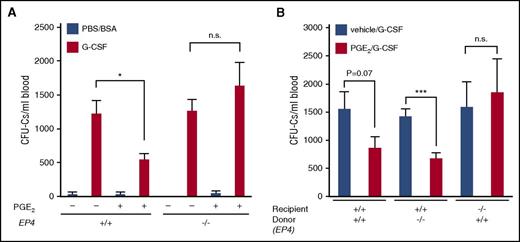
Among the 4 PGE receptors (EP1-EP4), the PGE2–EP4 pair has been identified as an important pathway to modulate the endosteal microenvironment.4,9 In particular, the suppression of PGE2 by NSAIDs or the conditional deletion of EP4 was reported to reduce the number of osteolineage cells together with the suppression of the bone matrix protein OPN, which led to the enhanced mobilization by G-CSF,9 as OPN is known to anchor immature hematopoietic cells in the BM.23 In line with this, we found that the suppression of HPC mobilization by exogenous PGE2 was completely abolished in EP4−/− mice (Figure 5A; supplemental Figure 10A), and this effect was attributable to the absence of EP4 in the microenvironment, but not in hematopoietic cells, as assessed in chimeric mice generated by the reciprocal transplantation between EP4+/+ and EP4−/− mice (Figure 5B; supplemental Figure 10B). Furthermore, we confirmed that OPN protein expression in the endosteal area was enhanced by PGE2 treatment mainly in diaphysis in an EP4-dependent manner (supplemental Figure 10C), and the administration of anti-OPN antibody canceled the inhibitory effect of PGE2 on HPC mobilization in WT mice (supplemental Figure 10D). Although these assays are not the direct evaluation of endogenous PGE2 produced by neutrophils during G-CSF treatment, we could confirm that PGE2 had a great potential to induce OPN protein in the endosteal area through the EP4 receptor to anchor HPCs in the BM.
Regulation of mobilization by PGE2/EP4 signal. (A) CFU-Cs mobilized in EP4+/+ and EP4−/− mice treated with PGE2 (n = 3 for PBS/BSA group and n = 6-10 for G-CSF group). (B) CFU-Cs mobilized in EP4 chimeric mice treated with PGE2 (n = 6-12). Data are represented as mean ± SEM. *P < .05; ***P < .001. n.s., not significant.
Regulation of mobilization by PGE2/EP4 signal. (A) CFU-Cs mobilized in EP4+/+ and EP4−/− mice treated with PGE2 (n = 3 for PBS/BSA group and n = 6-10 for G-CSF group). (B) CFU-Cs mobilized in EP4 chimeric mice treated with PGE2 (n = 6-12). Data are represented as mean ± SEM. *P < .05; ***P < .001. n.s., not significant.
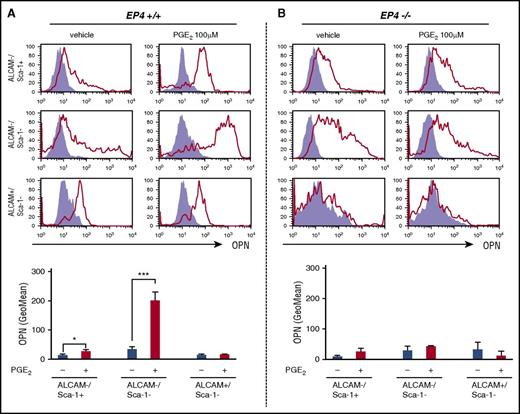
Thus, we tried to identify a possible target of PGE2 among osteolineage cells, with the upregulation of OPN protein as a marker. We established a quantification method for PGE2-mediated OPN protein induction in vitro by flow cytometry in osteolineage cell lines and fractionated primary osteoblasts from adult femurs. PGE2 increased the protein level of OPN in a dose-dependent manner in mesenchymal stromal cells ST2 and osteoblastic cells MC3T3-E1 (supplemental Figure 11A-B). Using this system, we analyzed primary endosteal cells extracted from femoral bone tissues of EP4+/+ and EP4−/− mice. Enzymatically obtained osteoblastic cells were sorted in 3 populations, according to the expression profile of activated leukocyte cell-adhesion molecule (ALCAM) and Sca-1 (supplemental Figure 12).24 In cultures, PGE2 treatment upregulated OPN protein slightly in ALCAM−/Sca-1+ mesenchymal progenitors and drastically in ALCAM−/Sca-1− preosteoblast fraction, whereas no increase was observed in ALCAM+/Sca-1− mature osteoblasts (Figure 6A). Consistent with the OPN expression profile in vivo (supplemental Figure 10C), no alteration of OPN by PGE2 was observed in all fractions in the absence of EP4 (Figure 6B). These results suggest that PGE2 could selectively target ALCAM−/Sca-1− preosteoblast fraction in the endosteal microenvironment to anchor HPCs.
PGE2/EP4 signal targets a certain population of osteolineage cells for OPN induction. Assessment of OPN protein expression by flow cytometry in primary osteoblastic cell cultures from EP4+/+ (A) and EP4−/− (B) mice with or without PGE2 treatment. The fluorescence intensity of each experiment is represented as the geometric mean (GeoMean) value by PE-anti-OPN (open red histogram) after subtraction of that by PE-mouse IgG (closed purple histogram; n = 3). Data are represented as mean ± SEM. *P < .05; ***P < .001.
PGE2/EP4 signal targets a certain population of osteolineage cells for OPN induction. Assessment of OPN protein expression by flow cytometry in primary osteoblastic cell cultures from EP4+/+ (A) and EP4−/− (B) mice with or without PGE2 treatment. The fluorescence intensity of each experiment is represented as the geometric mean (GeoMean) value by PE-anti-OPN (open red histogram) after subtraction of that by PE-mouse IgG (closed purple histogram; n = 3). Data are represented as mean ± SEM. *P < .05; ***P < .001.
Discussion
In the current study, we have demonstrated that BM neutrophils constitutively express mPGES-1 protein and significantly contribute to the modulation of the BM microenvironment and body temperature as a PGE2 source during G-CSF treatment. Our results suggest that G-CSF indirectly stimulates mature neutrophils to synthesize PGE2 via the SNS, in addition to the conventional effect on their expansion from their precursors.
It is reported that the expression of mPGES-1 is very low in most tissues because it is an inducible enzyme but is constitutively high in some particular organs, such as the kidney, placenta, and testis, where the “anytime ready” status to supply supplemental PGE2 on demand is likely indispensable for their appropriate functions.25,26 In the current study, we showed that PGE2 from BM neutrophils plays an important role to modulate body temperature and BM microenvironment during G-CSF treatment. Considering the constitutive expression of mPGES-1 and the significant control of the AA cascade by the SNS, BM neutrophils may be the vanguard in response to various stress stimuli on the whole body.
Because signals through G protein–coupled receptors stimulate intracellular Ca2+ elevation via inositol trisphosphate (IP3), which results in cPLA2 activation to start the AA cascade,27 it seems to be reasonable that the signal through β3-AR expressed on neutrophils enhances PGE2 synthesis (Figure 3C). PGE2 itself stabilizes cox-2 mRNA via the p38/mitogen-activated protein kinase pathway, likely because of the inhibition of tristetraprolin by its phosphorylation, resulting in the establishment of a cox-2/PGE2 positive feedback axis.28,29 Meanwhile, PGE2-mediated p38/mitogen-activated protein kinase signals inhibit NF-κB, a transcription factor for the production of many cytokines/chemokines, which results in the resolution of inflammation.30,31 In addition, the main product of cox-2 will be switched from PGE2 to PGD2, which also promotes the convergence of inflammation (Figure 1D; supplemental Figure 2F).29,32 Via the G-CSF-triggered cooperation between the SNS and neutrophils, the in vivo dynamics of PGE2 synthesis may coordinate the transient inflammatory response and subsequent autoresolution. This transition may take place at about the fourth to sixth doses of G-CSF because the increase of body temperature is not sustained throughout the whole treatment. It is also consistent with the behaviors of mPGES-1, cPLA2, cox-2, and NF-κB mRNAs in both isoproterenol-stimulated neutrophils in vitro (period of hours; supplemental Figure 4C) and G-CSF-treated BM (period of days; Figure 1D; supplemental Figure 2F) in our current study. The administration of G-CSF and subsequent alteration of BM microenvironment for mobilization (such as suppression of osteolineage cells) may be regarded as a stress by the mammalian body, and as a reaction of defense, Gr-1high neutrophils may be primed by the nervous system to produce PGE2 as a factor for marrow tissue repair and HPC maintenance. Activated neutrophils might be mobile and work in a similar way also in other tissues.
It is known that PGE2, which mediates fever, is produced in the central nervous system.33 However, a recent study demonstrated a significant contribution of PGE2 produced in peripheral organs, particularly at the early phase of fever.34 In a study by Steiner et al, it is shown that the neutralization of PGE2 mainly from the lung and liver by anti-PGE2 antibody, which does not cross the blood–brain barrier, attenuated LPS-induced fever. In our current study, we found that fever was attenuated in mPGES-1−/− (Figure 1B; supplemental Figure 1), neutrophil-depleted (Figure 4C), and SNS-denervated mice (Figure 4F) during G-CSF treatment, which suggested that SNS-triggered neutrophil-derived PGE2 initiated fever. Because anti-Gr-1 antibody depleted Gr-1high neutrophils in both BM and peripheral blood, circulating neutrophils would also contribute to the control of body temperature. A clear effectiveness of NSAIDs for G-CSF-induced bone pain, as well as fever in the clinic, suggests that neutrophil-derived PGE2 in the BM might sensitize nociceptors in the BM/bone afferent nerves.35
Because the effect for the role of endogenous PGE2 triggered by G-CSF might not be strong enough in our EP4−/− strain, we assessed the in vivo EP4 function by exogenous PGE2 administration. Anti-OPN antibody is noted to abolish the suppression of mobilization by exogenous PGE2 (supplemental Figure 10D). Furthermore, we clearly showed that PGE2 directly stimulated the strong induction of OPN protein in a certain osteolineage population (Figure 6). Although it is not a direct assessment of the function of endogenous PGE2, one of the major roles of PGE2 in the microenvironment may be the induction of OPN protein to anchor HPCs. The lack of enhanced mobilization in EP4−/− mice could be a result of the treatment period because it was reported that the enhanced mobilization in OPN−/− mice was apparent at 12 doses of G-CSF, but not at 8 doses.23 CXCL12 is known as a potent chemoattractant for the retention of HSCs/HPCs in the BM,36 but it is reported that the PGE2 action is a CXCL12-independent mechanism.9 In addition to G-CSF, we also assessed the contribution of the PGE2-OPN axis in HPC mobilization by AMD3100, an antagonist for CXCL12 receptor CXCR4. PGE2 clearly suppressed AMD3100-induced mobilization, and anti-OPN antibody abolished this effect (data not shown), which indicated that PGE2-mediated microenvironment modulation is mainly the OPN induction and, consistent with the report of Hoggatt et al,9 is likely independent of CXCL12.
Ikushima et al showed that ALCAM−/Sca-1+ cells were capable of supporting HSC/HPC proliferation on stimulation by PGE2,4 whereas the purpose of our experiments was to identify the cell population that may control the trafficking of HPCs in the BM. We found that the ALCAM−/Sca-1− fraction was the strong responder to PGE2 in terms of the OPN protein induction on PGE2 stimulation. Thus, although the purpose and the method were different between 2 studies, these osteolineage ALCAM−/Sca-1+ and ALCAM−/Sca-1− fractions may harbor different functions as niche cells, the proliferation and trafficking of HPCs, respectively, under the control of the PGE2/EP4 pathway.
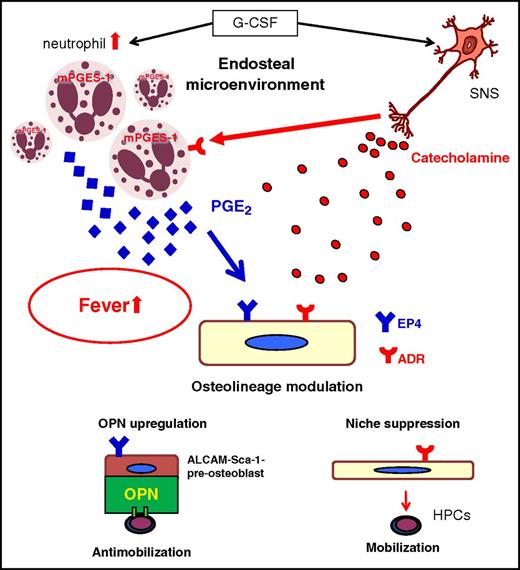
In our current study, we demonstrate that both hematopoietic and neurotropic actions of G-CSF cooperate (Figure 7). G-CSF is well known to expand BM neutrophils from their progenitors.37 G-CSF can also suppress macrophages that support niche cell function,18,38 reduce the stromal cell synthesis of HSC/HPC retention factors in the BM such as CXCL12,14,36,39 suppress osteolineage functions,15,17,40 and stimulate neutrophils to produce PGE2 in the BM. Neutrophil-derived PGE2 increases body temperature and may induce OPN expression via EP4 in ALCAM−/Sca-1− osteoblast precursors, which counteracts mobilization (our current study and Hoggatt et al9 ). Neutrophils align many conditions to efficiently regulate this process, such as the dramatic scaling of cell pool by rapid expansion with short life-span, high motility, constitutive mPGES-1 expression, and high sensitivity to the sympathetic tone. This process may also modulate the innate immune reaction because neutrophils regulate macrophage functions.41 The identification of both a major physiological PGE2 source among hematopoietic cells and its recipient among niche populations is a significant advancement to understand the regulatory mechanism of BM homeostasis. In particular, our study uncovered the functions of mature hematopoietic cells, neutrophils, as regulators of the microenvironment for their immature progenitors. These complex pathways that simultaneously proceed in the BM reveal that the hematopoietic system is elaborately regulated by the interorgan communication of the nervous system, bone metabolism, and hematopoietic cells themselves. This study implies a potential clinical application of SNS modulators to control the innate immunity, inflammation, and tissue repair.
A model for G-CSF-induced fever and cooperative regulation of endosteal microenvironment by the SNS and neutrophils. As a classical function, G-CSF directly expands BM neutrophils from their progenitors, which constitutively express mPGES-1. In the meantime, G-CSF induces high sympathetic tone, which primes BM neutrophils to produce PGE2, resulting in fever. In addition to the direct suppression of osteoblastic microenvironment, high sympathetic tone also initiates the indirect regulation of osteoblastic niche by the induction of OPN to anchor hematopoietic progenitors via PGE2/EP4 signal. ADR, adrenergic receptors.
A model for G-CSF-induced fever and cooperative regulation of endosteal microenvironment by the SNS and neutrophils. As a classical function, G-CSF directly expands BM neutrophils from their progenitors, which constitutively express mPGES-1. In the meantime, G-CSF induces high sympathetic tone, which primes BM neutrophils to produce PGE2, resulting in fever. In addition to the direct suppression of osteoblastic microenvironment, high sympathetic tone also initiates the indirect regulation of osteoblastic niche by the induction of OPN to anchor hematopoietic progenitors via PGE2/EP4 signal. ADR, adrenergic receptors.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Paul S. Frenette (Albert Einstein College of Medicine, New York) for critical reading of our manuscript.
This work was supported by the Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (#19591112 and #23390251, Y. Katayama); Grants-in-Aid for Scientific Research on Innovative Areas “Stem Cell Aging and Disease” from the Ministry of Education, Culture, Sports, Science and Technology in Japan (#15H01512, Y. Katayama); Japan Science and Technology Agency, PRESTO (Y. Katayama); and GSK Japan Research Grant (Y. Kawano).
Authorship
Contribution: Y. Kawano performed all the experiments and wrote the manuscript. C.F., K.W., S.I., T.S., M. Sato, N.A., H.K., K.M., and A.S. helped with animal maintenance, tissue sample preparation, cell cultures, PGE2 ELISA, and quantitative RT-PCR. M. Shinohara supervised the experiments with neutrophils and performed LC-MS/MS. T.F. supervised the experiments with neutrophils. S.U. and S.A. supervised the studies for mPGES-1−/− mice. T.U. supervised the experiments with the anti-OPN antibody. S.N. supervised the studies for EP4−/− mice. T.M. supervised all the experiments. Y. Katayama supervised all the experiments and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Yoshio Katayama, Hematology, Department of Medicine, Kobe University Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe 650-0017, Japan; e-mail: katayama@med.kobe-u.ac.jp.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal