Abstract

Background: We previously reported that haplo-HSCT after depletion of α/β T cells / CD19 B cells is a suitable option for patients with PIDs, with a high success rate (Bertaina et al., Blood 2014). However, in many patients, we observed a delay in the recovery of adaptive immunity, sometimes resulting in life-threatening or even fatal events, providing the rationale for exploring an innovative approach based on the post-transplantation infusion of donor T cells, genetically modified with the novel suicide gene iC9 (BPX-501 cells), with the aim of accelerating reconstitution of adaptive immunity. As the transduced gene contains sequences for the CD19 marker, BPX-501 cells (CD3+/CD19+) can be easily tracked in peripheral blood.
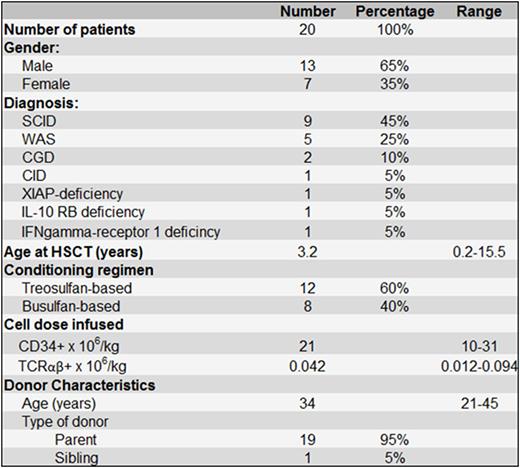
Patients and study design: In this multicenter, prospective phase I-II trial (enrolling both malignant and non-malignant diseases; sponsored by Bellicum Pharmaceuticals®, ClinicalTrials.gov identifier: NCT02065869) 20 children with PIDs have been enrolled. Nine children had Severe Combined Immune Deficiency (SCID), 5 Wiskott-Aldrich syndrome (WAS), 2 Chronic Granulomatosis Disease (CGD) and one each of 4 other PIDs detailed in Table 1, which also reports relevant patient-, donor- and transplant- characteristics. All patients were transplanted after depletion of donor α/β T cells and CD19 B cells, employed to prevent graft-versus-host disease (GvHD) and post-transplant lymphoproliferative disorders (PTLD). Details on cell subsets infused with the graft are reported in Table 1. No patient was given any post-transplantation GvHD prophylaxis. The phase I portion of the trial consisted of a classical 3+3 design with 3 cohorts, with escalating doses of BPX-501 cells of 2.5x105, 5x105, and 1x106 cells/kg, respectively. Patients in the phase II portion received the highest dose identified during the phase I portion (1x106 cells/kg).
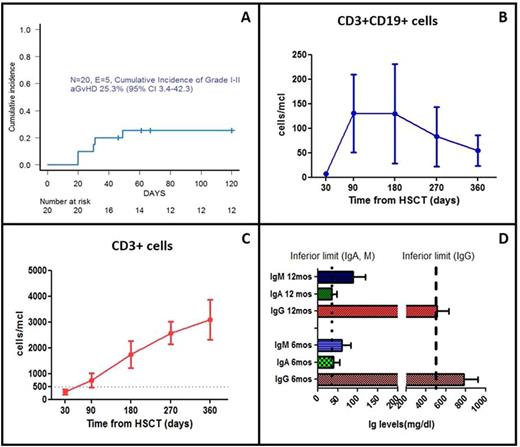
Results: All patients engrafted and no secondary graft failure was recorded. The median time to neutrophil and platelet recovery was 16 (range 11-35) and 10 days (range 7-14), respectively. BPX-501 cells were infused at a median time of 15 days (range 13-56) after the allograft. Four patients were enrolled in the phase I portion of the study; one received 2.5x105 and 3 received 1x106 cells/kg. The remaining 16 children were treated in the phase II part, with a dose was 1x106 cells/kg. Five children experienced Grade I (3 patients) or Grade II (2 children) acute GvHD, which resolved with either topical or systemic steroids in 3 patients. The other 2 cases resolved after the infusion of Rimiducid (AP1903) which activated the iC9 suicide gene. The cumulative incidence of acute GvHD is shown in Figure 1A. Two of the 17 patients at risk (i.e. those with a follow-up longer than 100 days after transplantation) developed mild (skin only) chronic GvHD. The median time to discharge was 36 days (range 26-180). Eight patients (40%) experienced one episode of re-hospitalization after initial discharge. After a median follow-up of 10 months (range 50 days-20 months), all patients are alive and disease-free. Details on expansion/persistence of BPX-501 cells, as well as on recovery of CD3+ cells are shown in Figure 1B and 1C, respectively. Ig serum levels of SCID patients at 6 and 12 months after transplant are depicted in Figure 1D. The median follow-up for WAS patients is 510 days (124-531 days) and their median platelet count at 1, 3 and 12 months after haplo-HSCT was 136 (range 48-168), 204 (range 98-280) and 143 (117-365) x109/L, respectively. One SCID patient who developed BCG bacterial dissemination after the allograft resolved this infection and 3 patients (2 with SCID and one with WAS) cleared cytomegalovirus (2 children) or Adenovirus (one child) infections pre-existing at time of conditioning regimen.
Conclusions: These results indicate that haplo-HSCT, after depletion of α/β T cells and B cells followed by adoptive infusion of donor BPX-501 cells, is an effective alternative for those children with PIDs in need of an urgent allograft or lacking a suitable HLA-matched donor. BPX-501 cells expand in vivo and persist over time, contributing to fasten the recovery of adaptive T-cell immunity and to clear infections. In view of the absence of fatalities and of the low rate of mild chronic GvHD, we conclude that infusion of BPX-501 T cells with the iC9 cell-suicide system may potentially render haplo-HSCT a first-line option for children with PIDs.
Qasim:Cellectis: Research Funding; Autolus: Consultancy, Equity Ownership, Research Funding; Catapult: Research Funding; Calimmune: Research Funding. Slatter:Medac: Other: Travel grants. Moseley:Bellicum Pharmaceuticals: Employment, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal