Abstract

INTRODUCTION: Guadecitabine (SGI-110) is a next generation hypomethylating agent (HMA) formulated as a dinucleotide of decitabine and deoxyguanosine, with an increased length of exposure compared to decitabine due to reduced metabolism by cytidine deaminase. Previous phase 1 and phase 2 clinical trials of guadecitabine demonstrated clinical activity both in untreated and previously treated patients with MDS, with good tolerance. Improving the current response and survival outcomes of patients with higher risk MDS and CMML, particularly in the presence of very high risk biological features, is fundamental. In the current clinical trial we assessed the activity of guadecitabine in patients with higher-risk MDS and CMML as front-line therapy.
METHODS: We are conducting a single arm, non-randomized phase 2 clinical trial of guadecitabine for patients with newly diagnosed MDS or CMML classified as Intermediate-2 or High risk by IPSS. Treatment consisted of guadecitabine at a dose of 60mg/m2 sc daily for 5 days (days 1-5) every 28 days. The primary endpoint was complete response (CR). Secondary objectives included overall response rate (ORR), survival and transfusion independence. Responses were evaluated following the revised 2006 International Working Group (IWG) criteria. Sequencing data was obtained at the time of pre-treatment evaluation by the use of a 28-gene next generation sequencing platform. Study included stopping rules for response and toxicity whereby the study would stop if the CR rate was unlikely (chance <2.5%) to improve over standard of care azacitidine (10% CR rate) by more than 15%, or if at any given time the chance of related grade ≥3 non-hematological toxicity being >30% was >95%, respectively. Adverse events (AEs) were assessed and graded according to the CTCAE v4 criteria. Overall survival (OS) was censored at the time of transplant. Event-free survival (EFS) was defined as the time interval between treatment start and date of resistance, progression or death.
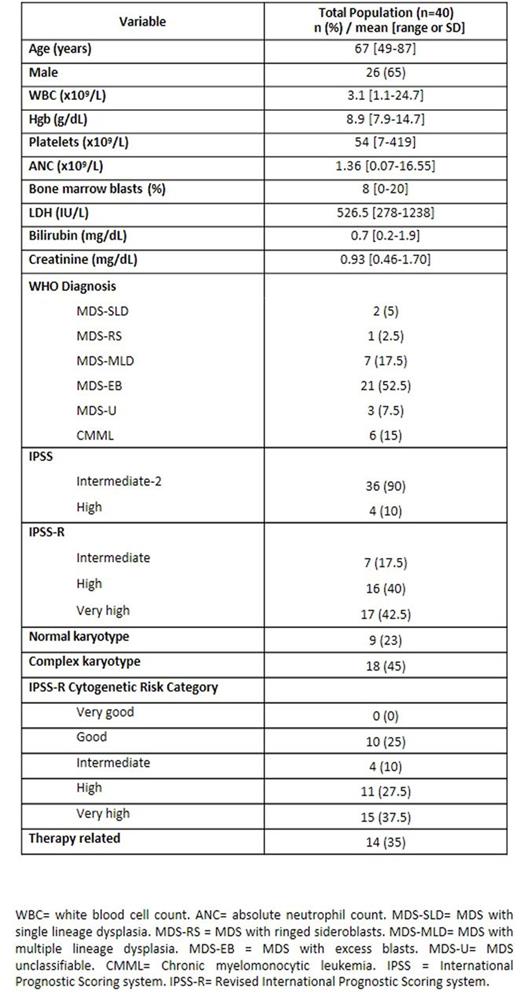
RESULTS: A total of 40 patients were enrolled between November 2014 and June 2016. Thirty-seven (93%) were evaluable for toxicity and 36 (90%) for response at the time of analysis. Patient characteristics are shown in Table 1. Median age was 67 years (range 48-86). A total of 34 (85%) patients had MDS and 6 (15%) had CMML. Thirty-six (90%) were classified as int-2 risk and 4 (10%) as high risk by IPSS. A total of 9 (23%) had normal karyotype and 18 (45%) had complex karyotype. Sequencing data was available in 38 (95%) patients. Identified mutations are shown in Figure 1A, with TP53 mutations being the most frequently detected in 15 (38%) patients. Following a median of 6 treatment cycles (range 1-17), 10 (28%) subjects met the primary endpoint by achieving CR. ORR was observed in 22 (61%) subjects, with 4 (10%) hematologic improvement (HI) and 9 (23%) CRi defined as mCR+HI. Median best response occurred by 3 cycles (range 1-6). Of subjects evaluable for cytogenetic response, (n-26; 72%), 6 (21%) achieved a complete cytogenetic response (CCyR). Seven (19%) subjects responded sufficiently to be removed from the study and proceed to allogeneic stem cell transplantation. Only one (3%) patient had transformation to acute myeloid leukemia. Median follow up was 4 months (range 0-19 months). Median OS was 15.2 months (95% CI 12.13-18.25 months) (Figure 1B) and median EFS was 10.8 months (95% CI 6.9-14.76 months) (Figure 1C). At the present time of follow up, no significant differences in survival were observed based on achievement of response (NR vs 15 months, p=0.142) or CR (13.6 vs 15.1 months, p=0.474). A total of 31 (84%) patients experienced at least one AE during therapy with 4 (11%) patients having related grade ≥3 non-hematologic AEs including fatigue, febrile neutropenia and oral mucositis. Therefore, stopping rule for toxicity was not met. Most common grade 1-2 AEs included fatigue (35%), nausea (24%) and dyspnea (24%). Dose reductions due to cytopenias were required in 12 (33%) patients. Early 8-week mortality occurred in 2 (5%) patients, one due to non-related cardiac arrest and one due to sepsis.
CONCLUSION: Guadecitabine is a well-tolerated and active new HMA for patients with higher-risk MDS and CMML even in the presence of adverse biological features such as high frequency of complex karyotype, therapy related disease and TP53 mutations. Further follow up is required to assess survival benefit in terms of OS and leukemia-free survival.
Daver:Pfizer: Consultancy, Research Funding; Kiromic: Research Funding; Sunesis: Consultancy, Research Funding; Ariad: Research Funding; BMS: Research Funding; Karyopharm: Honoraria, Research Funding; Otsuka: Consultancy, Honoraria. Cortes:ARIAD: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Teva: Research Funding. DiNardo:Novartis: Research Funding; Celgene: Research Funding; Daiichi Sankyo: Research Funding; Agios: Research Funding; Abbvie: Research Funding. Jabbour:ARIAD: Research Funding; Novartis: Research Funding; Pfizer: Research Funding; BMS: Consultancy; Pfizer: Consultancy; ARIAD: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal