Abstract
Introduction: Immune checkpoint therapy has been successful in many solid tumors andHodgkins lymphoma.The expression and clinical implications of immune checkpoints in the tumor microenvironment in patients (pts) with AML remain poorly defined.Identification and targeting of immune checkpoints in AMLwill guide the rational selection of specific antibodies for clinical trials.
Methods:Between March, 2015 and April 2016 we performed17-colormulti-parameter flow-cytometry (MFC) on bone marrows (BM) aspirate from 74 pts with AML (36 untreated AML, 38 relapsed AML). We evaluated expression of immune receptors (inhibitory receptors: PD1, CTLA4, LAG3, TIM3, and activating receptors GITR, OX40, 41BB, ICOS) on T-cell subsets: CD4 T effector cells [Teff]: CD3+CD4+CD127lo/+Foxp3, CD4 T regulatory cells [Treg]: CD3+CD4+CD127-Foxp3+, and CD8 T cells. AML blasts were assessed for both immune receptors (as above), and ligands (4-1BBL, B7-1, B7-2, ICOSL, PDL-1, PDL-2, OX40L).Eight healthy human BMs were used as control. These analyses were performed on freshly collected BM aspirate by the M. D. Anderson Cancer Center Immunotherapy Platform.
Results: A total of 74 pts were evaluated. Our analyses show that T-cell populations are preserved in BM of untreated and relapsed AML patients. In untreated AML BM, median frequency of live CD3+, CD4+, and CD8+ T cells were 16.5%, 10.4%, and 5.1% respectively. In relapsed AML BM, median frequency of live CD3+, CD4+, and CD8+ T cells were 19.2%, 9.5%, and 4.5% respectively.
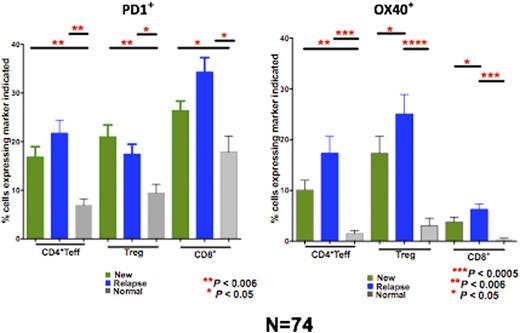
The expression of the8 costimreceptors and 7 ligands varied significantly between individual AML pts. On analysis of all markers PD-1 and OX40 emerged as potential checkpoint receptors of importance in AML.The baseline expression of OX40 and PD-1 on the CD8, Teff, and Treg cells are shown in Figure 1. All T cell subpopulations had significantly higher PD1 expression in relapsed AML (P<0.006) and untreated AML (P<0.05) compared to healthy controls. There were no significant differences in PD1 expression between relapsed and untreated AML. OX40 expression was significantly higher on all T cell subpopulations in relapsed AML pts (P<0.006) and specifically on Teff cells in untreated AML (P<0.006) when compared to healthy controls. Moreover, Treg cells in relapsed AML pts expressed significantly higher OX40 compared to untreated AML.The expression of costimulatory receptors and ligands differed significantly between BM and PB for the same time-point in the same pt (PB data not shown here).
We compared the T-cell repertoire and checkpoint receptor/ligand expression to baseline clinical characteristics (age, cytogenetics, therapy-related status) and outcomes. Pts with untreated AML with adverse karyotype had a higher expression of PDL2 on AML blasts (P=0.07) in the BM. Pts with untreated AML who responded to induction therapy had a trend to higher Teff live cells (P=0.2), and lower OX40 on CD8 cells (P=0.04) in the BM. In relapsed AML higher T-eff live cells (P=0.04) and higher OX40 expression on CD8 (P=0.009) in BM were associated with improved survival.
Conclusions: Total T-cell and T-cell subset populations are preserved in the BM of pts with untreated and relapsed AML and may be manipulated by checkpoint antibodies. Clinically targetable checkpoint receptors, specifically PD1 and OX40 are overexpressed in the BM of pts with AML and may be manipulated to unleash T-cells.
PD1 and OX40 expression in new (N=34) and relapsed AML (N=38), and healthy controls (N=8)
PD1 and OX40 expression in new (N=34) and relapsed AML (N=38), and healthy controls (N=8)
Daver:BMS: Research Funding; Kiromic: Research Funding; Karyopharm: Honoraria, Research Funding; Pfizer: Consultancy, Research Funding; Sunesis: Consultancy, Research Funding; Otsuka: Consultancy, Honoraria; Ariad: Research Funding. Cortes:ARIAD: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Teva: Research Funding. Konopleva:Calithera: Research Funding; Cellectis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal