Abstract

INTRODUCTION: Most clinical trials exclude patients with poor performance, organ dysfunction, and presence of other active malignancies or comorbidities. Although some of these criteria are based on clinical reasoning, patients with such clinical features have dismal expected outcomes and limited therapeutic options and could therefore have a more favorable risk/benefit ratio if treated with a low intensity investigational intervention. The current study was designed to test whether it is feasible to treat patients not eligible for conventional studies in a clinical trial.
METHODS: We conducted an initial Bayesian designed single-arm study and a subsequent randomized study for patients with AML or higher-risk MDS (intermediate-2 or high risk by IPSS) with either ECOG performance status (PS) ≥3, creatinine or bilirubin ≥2mg/dL, presence of other malignancy or other comorbidities. Primary endpoint was survival at day 60. The study included stopping rules for survival, response and toxicity. All patients received azacitidine 75mg/m2 sc daily for 5 days. Patients in the single-arm study and in the combination arm of the randomized study also received vorinostat 200mg tid for 5 days. Cycles could be repeated every 3-8 weeks. Responses were evaluated following the revised 2006 IWG criteria for patients with MDS and the IWG 2003 recommendations for patients with AML. Comorbidities were evaluated using the Adult Comorbidity Evaluation-27 (ACE-27) index. Adverse events (AEs) were assessed and graded according to the CTCAE v4 criteria. Overall survival (OS) was censored at the time of transplant. Event-free survival (EFS) was defined as the time interval between treatment start and date of resistance, progression or death.
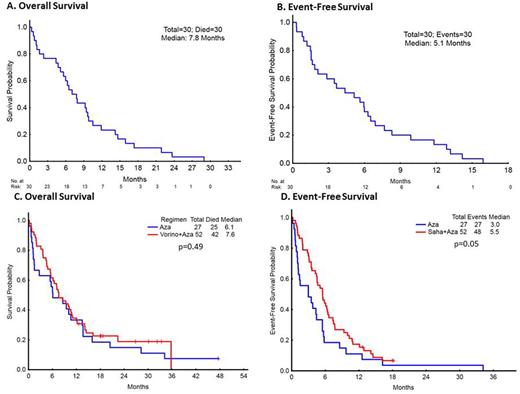
RESULTS: A total of 30 patients (16 with MDS, 14 with AML) were enrolled in the initial single-arm study. Patient characteristics and inclusion criteria are detailed in Table 1. Median age was 73 years (44-83). Median follow-up was 7.4 months (0.3-29). Sixty-day survival was 83%. Median number of cycles administered was 3.5 (1-12). The overall response rate (ORR) was 40% with 8 (27%) patients achieving CR, 4 with AML and 4 with MDS. Median OS was 7.8 months (0.3-29, CI 7.54-8.03) (Figure 1A) and median EFS was 5.1 months (0.3-15.9, CI 4.87-5.37) (Figure 1B). Stopping rules for survival and response were not met. Main adverse events (AEs) where grade 1-2 gastrointestinal toxicities. Mortality at 4 and 8 weeks was 10 and 20% respectively. A total of 79 patients were enrolled in the subsequent randomized study: 27 to azacitidine (A) and 52 to azacitidine and vorinostat (A+V). Patient characteristics and inclusion criteria are also shown in Table 1. Median age was 70 years (30-90). Forty-seven (59%) patients had MDS and 32 (41%) had AML. Median follow-up was 22.7 months (12.6-47.5). Sixty-day survival rates were 67% (A) and 85% (A+V), respectively (p=0.07). No differences in ORR (48% vs 46%, p=0.87), OS (6.1 vs 7.6 months, p=0.49) (Figure 1C) or EFS (3 vs 5.5 months, p=0.05) (Figure 1D) were observed between groups. Main AEs included grade 1-2 gastrointestinal toxicities with a higher proportion of AEs with A+V (81 vs 56%). Mortality at 4 and 8 weeks was 10% (A: 4, A+V: 4) and 19% (A: 9, A+V: 6) respectively. By univariate analysis neither PS ≥3, creatinine or bilirubin ≥2mg/dL nor presence of other malignancy were predictive for 60-day survival, OS or EFS. There were no significant differences in survival between patients with ACE-27 scores of 0-1 compared to 2-3 both in the single-arm (6.3 vs 7 months, HR=0.88, 95% CI 0.41-1.91, p=0.75) and the randomized phase of the study (A: 13.5m vs 6.1m, HR 0.93, 95% CI 0.27-3.17, p=0.9 and A+V: 12.1m vs 7.4m, HR 1.38, 95% CI 0.61-3.14, p=0.4).
CONCLUSION: Most enrolled patients met the study's primary endpoint of survival at 60 days without major toxicity. Patients obtained clinical benefit with acceptable responses and survival despite their high comorbidity burden. Our results support the feasibility of treating patients with MDS or AML not eligible to other clinical trials due to poor performance status, comorbidities or organ dysfunction, with low intensity therapies within a clinical trial. These findings suggest relaxation of such criteria may likely increase the pool of clinical trial patient candidates and allow access to potential beneficial therapies for patients with otherwise dismal prognosis.
Jabbour:ARIAD: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Novartis: Research Funding; BMS: Consultancy. DiNardo:Abbvie: Research Funding; Novartis: Research Funding; Agios: Research Funding; Daiichi Sankyo: Research Funding; Celgene: Research Funding. Cortes:ARIAD: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Teva: Research Funding. Wierda:Genentech: Research Funding; Gilead: Research Funding; Novartis: Research Funding; Acerta: Research Funding; Abbvie: Research Funding. Konopleva:Reata Pharmaceuticals: Equity Ownership; Abbvie: Consultancy, Research Funding; Genentech: Consultancy, Research Funding; Stemline: Consultancy, Research Funding; Eli Lilly: Research Funding; Cellectis: Research Funding; Calithera: Research Funding. Jain:Novimmune: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria, Research Funding; Pharmacyclics: Consultancy, Honoraria, Research Funding; Celgene: Research Funding; ADC Therapeutics: Consultancy, Honoraria, Research Funding; Genentech: Research Funding; Abbvie: Research Funding; Infinity: Research Funding; Incyte: Research Funding; Seattle Genetics: Research Funding; BMS: Research Funding; Novartis: Consultancy, Honoraria; Servier: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal