Abstract
Introduction
Genomic instability and complex karyotype are linked to chemoresistance, poor prognosis and early relapse rate in Acute Myeloid Leukemia (AML). Chromothripsis, a one-step catastrophic mechanism of genomic instability, could represent a driving force in the development and progression of hematological diseases and could be identified by high throughput technologies as Single Nucleotide Polymorphism (SNP) Array. We investigate the mechanisms involved in chromothripsis in newly diagnosed non M3-AML patients (patients) in order to better characterize a class of very high risk patients that could be candidate to innovative therapies.
Methods
We performed classical cytogenetic and microarray analysis (SNP Arrays 6.0 or Cytoscan HD Arrays, Affymetrix) in 418 AML samples. Data were analyzed by Nexus Copy Number™ and R Core Team. Chromothripsis-like patterns were confirmed by CTLP Scanner (Log Ratio ≥ 8, ≥ 10 switches, minimum segment size of 10 kb, distance between adjacent fragments ≤ 10% and 0.3 as variation from different copy number (CN) states). Overall survival was analyzed by Kaplan-Meier method and Mantel-Cox test.
Results
Twenty-six/418 patients (6.2%) showed chromothripsis involving different chromosomes. Chromosome 12 (23%), 17 (19%) and 5 (19%) were the most affected, followed by chromosomes 3, 6, 7, 8, 10, 11, 13, 15 and 20.
Patients harboring chromothripsis had a higher median age compared with chromothripsis-negative ones (70.4 vs. 55 years, respectively, p<.001) and a lower white blood cells (WBC) count at diagnosis (4,395 vs. 30,000, respectively, p =.019).
The group of patients with chromothripsis presented a prevalence of complex karyotype (p<.001) and high risk (HR) disease according to ELN definition (p<.001). Furthermore, we found a significantly higher incidence of TP53 mutation (p<.001) in chromothripsis-positive patients: 16/26 patients had an heterozygous loss of 17p13 (p<.001) and 21/24 harbored a TP53 mutation (2 samples were not evaluated) . TP53 loss and mutation co-occurred in 20 cases.
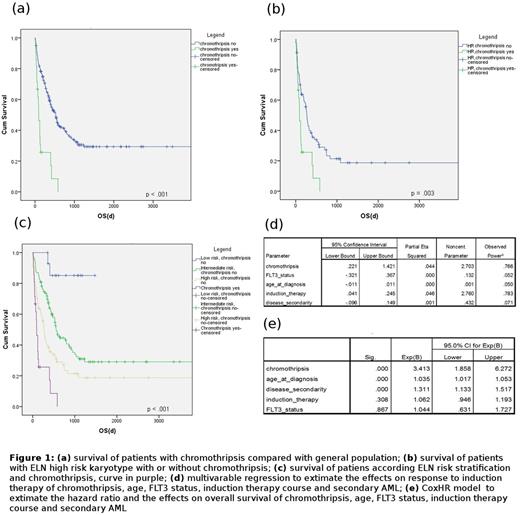
Chromothripsis-positive patients showed an extremely poor prognosis compared with chromothripsis-negative ones (median survival of 120 vs. 526 days, respectively, p<.001) and a 3.4 risk of death at Cox-hazard ratio analysis (C.I. 95%: 1.85-6.27). Moreover, chromothripsis showed to predict a lower response rate independently of age at diagnosis, de novo/secondary AML, FLT3 mutational status and type of induction therapy (p=.044).
Of note, chromothripsis was associated with worst prognosis even if compared with HR karyotype features without chromothripsis (median survival of 120 and 265 days, respectively, p<.001, Figure 1).
Finally, by comparing patients with and without chromothripsis, we identified several genes and pathways differentially altered between the 2 groups (p<0.001). Chromothripsis was particularly associated with loss of RAD50, FANCA, MARCH3, WNT8A, SHH, BCL2, USP34, CTNNA1, with 5q being the main altered chromosomic region, while ZFPM2 was the main amplified gene.
Conclusion
Our results demonstrate that chromothripsis is a recurrent event in adult AML and independently defines a group of patients with poor prognosis. Chromothripsis is strongly associated with TP53 alterations in AML and for the first time, we define incidence and survivals of chromothripsis in a set of 418 newly diagnosed consecutive AML patients.
Chromosomal abnormalities like chromothripsis could be a driving force in the development of cancer as well in hematological disease like AML, in which the genomic instability represent the main scenario. Since TP53 is known to deregulate Fanconi Anaemia genes, the deregulation of DNA double-strand break repair could sustain the maintenance of catastrophic mechanism like chromothripsis.
Acknowledgment
ELN, AIL, AIRC, PRIN, Progetto Regione-Università 2010-12 (L. Bolondi), FP7 NGS-PTL project.
MCF and GM equal contribution
Kralovics:Qiagen: Membership on an entity's Board of Directors or advisory committees; AOP Orphan: Research Funding. Martinelli:Novartis: Speakers Bureau; Amgen: Consultancy, Speakers Bureau; Celgene: Consultancy, Speakers Bureau; MSD: Consultancy; Genentech: Consultancy; Pfizer: Consultancy, Speakers Bureau; Ariad: Consultancy, Speakers Bureau; BMS: Speakers Bureau; Roche: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal