Key Points
In patients treated with ruxolitinib, harboring ≥3 mutations was inversely correlated with spleen response and time to treatment discontinuation.
Multigene profiling may be useful for therapeutic planning.
Abstract
Although most patients with myelofibrosis (MF) derive benefit from ruxolitinib, some are refractory, have a suboptimal response, or quickly lose their response. To identify genes that may predict response to ruxolitinib, we performed targeted next-generation sequencing (NGS) of a panel of 28 genes recurrently mutated in hematologic malignancies in a cohort of patients with MF who were treated with ruxolitinib in a phase 1/2 study. We also tested for CALR deletions by standard polymerase chain reaction methods. Ninety-eight percent of patients had a mutation in ≥1 gene. Seventy-nine (82.1%) patients had the JAK2V617F mutation, 9 (9.5%) had CALR mutations (7 type 1, 2 type 2), 3 (3.1%) had MPL mutations, and 4 (4.2%) were negative for all 3. ASXL1/JAK2 and TET2/JAK2 were the most frequently comutated genes. Mutations in NRAS, KRAS, PTPN11, GATA2, TP53, and RUNX1 were found in <5% of patients. Spleen response (≥50% reduction in palpable spleen size) was inversely correlated with the number of mutations; patients with ≤2 mutations had ninefold higher odds of a spleen response than those with ≥3 mutations (odds ratio = 9.37; 95% confidence interval, 1.86-47.2). Patients with ≥3 mutations also had a shorter time to treatment discontinuation and shorter overall survival than those with fewer mutations. In multivariable analysis, only number of mutations and spleen response remained associated with time to treatment discontinuation. Patients with ≥3 mutations had the worst outcomes, suggesting that multigene profiling may be useful for therapeutic planning for MF.
Introduction
Although most patients with myelofibrosis (MF) derive benefit from ruxolitinib, some are refractory or have a suboptimal response. Also, the duration of response differs between patients. To date, only 1 study has explored the impact of genetic mutations on response to ruxolitinib.1 Guglielmelli et al found that among patients enrolled in the phase 3 study comparing ruxolitinib with best available therapy (COMFORT-II),2 ruxolitinib-induced improvements in symptoms and splenomegaly were not associated with mutation status, and ruxolitinib improved survival even in patients with prognostically detrimental mutations (ASXL1, EZH2, SRSF2, and IDH1/2).1 That study evaluated 14 recurrently mutated genes and was performed before the discovery of the CALR mutation, which is present in up to 70% of patients who are JAK2 and MPL negative. In recent years, with the explosion of whole genome sequencing efforts, a number of rare, but recurrent, mutations have been identified in myeloproliferative neoplasms (MPNs), suggesting that there may be several paths to the development of MPNs, which have heterogeneous clinical presentations and treatment responses.3-5 To detect genes that may be correlated with response to ruxolitinib and other clinicopathologic features, we performed a comprehensive mutation profile of 29 genes recurrently mutated in primarily myeloid malignancies6 in a cohort of 95 patients with MF who were treated with ruxolitinib in a phase 1/2 study.7
Methods
Sequencing of patient samples
We performed targeted next-generation sequencing (NGS) of DNA samples from bone marrow or peripheral blood collected at study entry from 95 patients with MF who were treated in a phase 1/2 study of ruxolitinib at our center.7 The entire coding sequences of 28 genes (ABL1, ASXL1, BRAF, DNMT3A, EGFR, EZH2, FLT3, GATA1, GATA2, HRAS, IDH1, IDH2, KIT, KRAS, MDM2, IKZF2, JAK2, MLL, MPL, MYD88, NOTCH1, NPM1, NRAS, PTPN11, RUNX1, TET2, TP53, and WT1) were sequenced using a next generation sequencing (NGS)-based custom-designed assay using the Illumina MiSeq platform as previously described.6 Testing for insertion and deletion mutations in CALR was performed as previously described.8 Testing for SRSF2 mutations was not performed.
Clinical end points and statistical analysis
Overall survival (OS) was calculated from the first day of ruxolitinib treatment to the date of death or last follow-up (censoring date). Time to treatment discontinuation (TTD) was calculated from the first day of treatment to the last day of treatment or date of death. Patients still on therapy at the time of data analysis were censored at the date of last follow-up. We excluded 7 patients who went off study to receive a commercial supply of ruxolitinib from our analysis of TTD. The Kaplan-Meier method was used to estimate survival and TTD, and Cox regression was used to determine hazard ratios (HRs). This clinical study was initiated in 2007, and therefore, International Working Group for Myelofibrosis Research and Treatment (IWG-MRT) response criteria published in 2006 were used during the conduct of the study to assess response, as well as progression; the same was used in prior publications about this clinical study.9 Stepwise logistic regression with backward elimination was used to estimate odds ratios (ORs), and the Hosmer-Lemeshow test was used to assess goodness-of-fit.
Fisher’s exact and χ2 tests were used to assess the association between categorical variables, and the Mann-Whitney or Kruskal-Wallis test was used to assess the association between continuous variables. All P values are 2-tailed and were considered significant when <.05. Statistical analysis was performed using SPSS v.22. This study was based on a chart review protocol that was approved by the Institutional Review Board at MD Anderson Cancer Center.
Results
Analysis of mutations in patients treated with ruxolitinib
We performed NGS sequencing of a 28-gene panel on bone marrow or peripheral blood samples from 95 patients treated in a phase 1/2 trial of ruxolitinib at our institution. Of the 107 patients initially enrolled in the study, we had baseline samples for 95 patients.7 We also tested for insertion and deletion mutations in the CALR gene in patients without a JAK2 or MPL mutation. Patient characteristics at baseline are described in Table 1. The patient characteristics for these 95 patients did not differ significantly from those of the whole cohort.7,10 Ninety-three of 95 (97.9%) patients had a mutation in ≥1 gene: 51 (53.7%) patients had 1 mutation, 30 (31.6%) had 2 mutations, and 12 (12.6%) had ≥3 mutations (Figure 1A-B).11 Seventy-nine (82.1%) patients had the JAK2V617F mutation, 9 (9.5%) had CALR mutations, 3 (3.1%) had MPL mutations, and 4 (4.2%) were negative for all 3 mutations (triple-negative [TN]). ASXL1/JAK2 and TET2/JAK2 were the most frequently comutated genes (Figure 1C). Other mutations were found in <5% of patients. No mutations were detected in ABL1, FLT3, HRAS, IKZF2, KIT, MLL, NOTCH1, or WT1. A summary of all mutations is shown in supplemental Table 1 available on the Blood Web site.
Clinical and demographic characteristics of patients with MF stratified by diagnosis (N = 95)
| Characteristic . | All patients (N = 95) . | PMF (n = 54) . | PPV-MF (n = 31) . | PET-MF (n = 10) . | P value . |
|---|---|---|---|---|---|
| Age (years) | 66 (40-84) | 54 (40-84) | 66 (52-80) | 72 (60-80) | .025 |
| Sex (female) | 42 (44) | 32 (59) | 17 (55) | 4 (40) | .526 |
| Hg (g/dL), mean (range) | 10.7 (7.2-16.9) | 11 (7.2-16.9) | 11 (8.7-14.5) | 10 (8.5-13.2) | .099 |
| WBC (109/L), mean (range) | 25 (2.5-159) | 24 (2.5-159) | 30 (2.9-100) | 12 (2.7-26.9) | .008 |
| Plt (109/L), mean (range) | 339 (13-969) | 295 (13-871) | 392 (102-835) | 416 (113-969) | .083 |
| PBBL (%), mean (range) | 0.96 (0-8.0) | .917 | |||
| PBBL ≥1% | 26 (27) | 13 (24) | 10 (32) | 3 (30) | .704 |
| Baseline spleen size (cm), mean (range) | 19.3 (3-35) | .027 | |||
| Transfusion dependence* | 23 (24) | 12 (22) | 7 (23) | 4 (40) | .468 |
| DIPSS Int-2 | 50 (57) | 30 (58) | 14 (54) | 6 (60) | .927 |
| Leukemic transformation | 7 (7.4) | 4 (7.4) | 2 (6.5) | 1 (10) | .933 |
| Cytogenetics | |||||
| Diploid | 54 (57) | 33 (61) | 13 (42) | 8 (80) | .221† |
| Abnormal | 38 (40) | 19 (35) | 17 (55) | 2 (20) | |
| IM | 3 (3.2) | 2 (3.7) | 1 (3.2) | 0 | |
| der(6)t(1;6)(q21-25;p21.3-23) | 5 (5.3) | 2 (3.7) | 3 (9.7) | 0 | |
| del13(q12-14;q14-22) | 9 (9.5) | 5 (5.3) | 4 (13) | 0 | |
| del20(q11.21;q13.3) | 12 (13) | 6 (6.3) | 5 (16) | 1 (10) | |
| Average dose intensity | .549 | ||||
| ≤10 mg BID | 20 (21) | 10 (18) | 6 (19) | 4 (40) | |
| >10 to ≤20 mg BID | 42 (44) | 23 (43) | 15 (48) | 4 (40) | |
| >20 mg BID | 33 (35) | 21 (39) | 10 (32) | 2 (20) | |
| G3/4 hematologic toxicities | |||||
| G3/4 anemia/thrombocytopenia | 70 (74) | 39 (72) | 22 (71) | 9 (90) | .461 |
| No G3/4 anemia/thrombocytopenia | 25 (26) | 15 (28) | 9 (30) | 1 (10) | .205 |
| G3/4 anemia | 34 (36) | 16 (30) | 13 (43) | 5 (50) | |
| G3/4 thrombocytopenia | 18 (19) | 12 (22) | 6 (20) | 0 | |
| G3/4 anemia and thrombocytopenia | 18 (19) | 11 (20) | 3 (10) | 4 (40) | |
| IWG spleen response (N = 88) | 63 (72) | 33 (66) | 22 (79) | 8 (80) | .409 |
| IWG SR duration, mean (weeks) (N = 63) | 34.7 (2.8-74.2) | 29.8 (2.8-68.5) | 39.8 (4.8-74.2) | 41 (13.5-58.9) | .309 |
| Patients still on study (N = 20) | 20 (21) | 7 (13) | 12 (39) | 1 (10) | .013 |
| TTD, mean (weeks) | 177 (7-387) | 151 (9-369) | 213 (7-387) | 206 (60-328) | .052 |
| Overall survival, mean (weeks) | 207 (7-387) | 194 (43-372) | 243 (7-387) | 246 (60-336) | .058 |
| Characteristic . | All patients (N = 95) . | PMF (n = 54) . | PPV-MF (n = 31) . | PET-MF (n = 10) . | P value . |
|---|---|---|---|---|---|
| Age (years) | 66 (40-84) | 54 (40-84) | 66 (52-80) | 72 (60-80) | .025 |
| Sex (female) | 42 (44) | 32 (59) | 17 (55) | 4 (40) | .526 |
| Hg (g/dL), mean (range) | 10.7 (7.2-16.9) | 11 (7.2-16.9) | 11 (8.7-14.5) | 10 (8.5-13.2) | .099 |
| WBC (109/L), mean (range) | 25 (2.5-159) | 24 (2.5-159) | 30 (2.9-100) | 12 (2.7-26.9) | .008 |
| Plt (109/L), mean (range) | 339 (13-969) | 295 (13-871) | 392 (102-835) | 416 (113-969) | .083 |
| PBBL (%), mean (range) | 0.96 (0-8.0) | .917 | |||
| PBBL ≥1% | 26 (27) | 13 (24) | 10 (32) | 3 (30) | .704 |
| Baseline spleen size (cm), mean (range) | 19.3 (3-35) | .027 | |||
| Transfusion dependence* | 23 (24) | 12 (22) | 7 (23) | 4 (40) | .468 |
| DIPSS Int-2 | 50 (57) | 30 (58) | 14 (54) | 6 (60) | .927 |
| Leukemic transformation | 7 (7.4) | 4 (7.4) | 2 (6.5) | 1 (10) | .933 |
| Cytogenetics | |||||
| Diploid | 54 (57) | 33 (61) | 13 (42) | 8 (80) | .221† |
| Abnormal | 38 (40) | 19 (35) | 17 (55) | 2 (20) | |
| IM | 3 (3.2) | 2 (3.7) | 1 (3.2) | 0 | |
| der(6)t(1;6)(q21-25;p21.3-23) | 5 (5.3) | 2 (3.7) | 3 (9.7) | 0 | |
| del13(q12-14;q14-22) | 9 (9.5) | 5 (5.3) | 4 (13) | 0 | |
| del20(q11.21;q13.3) | 12 (13) | 6 (6.3) | 5 (16) | 1 (10) | |
| Average dose intensity | .549 | ||||
| ≤10 mg BID | 20 (21) | 10 (18) | 6 (19) | 4 (40) | |
| >10 to ≤20 mg BID | 42 (44) | 23 (43) | 15 (48) | 4 (40) | |
| >20 mg BID | 33 (35) | 21 (39) | 10 (32) | 2 (20) | |
| G3/4 hematologic toxicities | |||||
| G3/4 anemia/thrombocytopenia | 70 (74) | 39 (72) | 22 (71) | 9 (90) | .461 |
| No G3/4 anemia/thrombocytopenia | 25 (26) | 15 (28) | 9 (30) | 1 (10) | .205 |
| G3/4 anemia | 34 (36) | 16 (30) | 13 (43) | 5 (50) | |
| G3/4 thrombocytopenia | 18 (19) | 12 (22) | 6 (20) | 0 | |
| G3/4 anemia and thrombocytopenia | 18 (19) | 11 (20) | 3 (10) | 4 (40) | |
| IWG spleen response (N = 88) | 63 (72) | 33 (66) | 22 (79) | 8 (80) | .409 |
| IWG SR duration, mean (weeks) (N = 63) | 34.7 (2.8-74.2) | 29.8 (2.8-68.5) | 39.8 (4.8-74.2) | 41 (13.5-58.9) | .309 |
| Patients still on study (N = 20) | 20 (21) | 7 (13) | 12 (39) | 1 (10) | .013 |
| TTD, mean (weeks) | 177 (7-387) | 151 (9-369) | 213 (7-387) | 206 (60-328) | .052 |
| Overall survival, mean (weeks) | 207 (7-387) | 194 (43-372) | 243 (7-387) | 246 (60-336) | .058 |
Hg, hemoglobin; IM, not measurable; IWG, international working group; PBBL, peripheral blood blasts; PET-MF, postessential thrombocythemia myelofibrosis; Plt, platelets; PMF, primary myelofibrosis; PPV-MF, postpolycythemia vera myelofibrosis; SR, spleen response; WBC, white blood cell.
Transfusion dependence was defined as patients who required transfusions at the time they started on ruxolitinib.
Comparison is between diploid, abnormal, and IM.
Frequency and distribution of mutations. (A) Circos plot showing the frequency of co-occurring mutations.11 Length of the arc corresponds to the frequency of mutations, whereas the width of the ribbons between 2 genes shows the frequency of co-occurrence. (B) Frequency of mutations by disease subtype. (C) Plot of mutations by case.
Frequency and distribution of mutations. (A) Circos plot showing the frequency of co-occurring mutations.11 Length of the arc corresponds to the frequency of mutations, whereas the width of the ribbons between 2 genes shows the frequency of co-occurrence. (B) Frequency of mutations by disease subtype. (C) Plot of mutations by case.
Seven patients had mutations in genes that are part of the mitogen-activated protein kinase/Ras pathway (PTPN11, KRAS, and NRAS). Of these, 4 patients with PMF had RAS mutations (2 KRAS and 2 NRAS). Although our sample size was small, we observed a trend toward worse survival for patients with G12 KRAS or NRAS mutations (P = .052).
One patient had a KRAS I36M mutation, which has been reported in patients with Noonan syndrome.12 Three patients had mutations in PTPN11, encoding the SHP2 nonreceptor protein tyrosine phosphatase, which plays an essential role in the survival of hematopoietic progenitor cells.13 Three patients had mutations in GATA2, a master transcriptional regulator that controls the proliferation and differentiation of hematopoietic progenitor cells.14 Germ-line mutations in GATA2 have been described in a wide range of immune dysfunctions that fall under the umbrella of “GATA2 deficiencies,” including Monomac syndrome, dendritic cell monocyte and lymphoid deficiency, familial myelodysplastic syndrome/acute myeloid leukemia (AML), and Emberger’s syndrome.15 Notably, 2 of 3 patients with GATA2 mutations also had mutations in PTPN11 and KRAS. Because all of the patients had died at the time of this analysis, we were not able to test germ-line DNA samples in these cases.
Only 2 patients had a mutation in either RUNX1 or TP53, which have been reported in both primary and post-MPN AML.16,16-19 Both have been rarely identified in MF20,20-22 and often occur in the context of abnormal cytogenetics.23 However, both patients had a diploid karyotype and neither had transformation to AML. The patient with the TP53 mutation died of an abdominal aortic aneurysm after surgery and the patient with the RUNX1 mutation died of disease progression/sepsis.
Comparing the clinical characteristics of JAK2-positive, CALR-positive, MPL-positive, and TN MF patients, those with CALR mutations had significantly lower hemoglobin (mean, 8.6 vs 10.7 g/dL; P = .001) and white blood cell counts (mean, 11.0 vs 25 g/dL; P = .033), trends that have been reported in other MPN cohorts.24,25 There was no significant difference in age, platelet counts, or peripheral blood blasts. Because only 2 patients had the type 2 CALR mutation, we were unable to statistically compare clinical parameters between those with type 1 and type 2 mutations. However, there did not appear to be any striking differences between those with type 1 and type 2 mutations. Our data suggest that DNMT3A mutations were significantly more prevalent in patients with the CALR mutation: 2 of 9 (22%) patients with CALR (both type 1 insertions) compared with 1 of 79 (1.3%) with JAK2 mutations and none of those with MPL mutations (P = .008). However, our sample size was small. Among 14 patients with the TET2 mutation, 9 (64%) were also positive for JAK2V617F, 2 (14%) were positive for CALR mutations (1 type 1 and 1 type 2), and 2 (14%) were positive for MPL mutations. Similar to previous reports, we found that TET2 mutations were associated with older age (mean, 69 [range, 41-80] vs 66 [range, 43-84] years; P = .039).
Correlation of mutations and response to ruxolitinib
Spleen response
Eighty-eight patients were evaluable for a spleen response (3 patients who had splenectomy and 4 with no palpable spleen at baseline were not evaluable). Sixty-three of 88 (72%) patients had an IWG-defined spleen response at any point in the study. Mean palpable spleen size at baseline was 19.3 cm (range, 3-35 cm) and was not correlated with spleen response. Spleen response was not associated with JAK2, CALR, MPL, or TN mutation status (supplemental Table 2). However, patients with 1 or more mutations in ASXL1, EZH2, or IDH1/2 and those with ≥3 mutations of any type were significantly less likely to have a spleen response than those with no ASXL1, EZH2, or IDH1/2 mutations (52% vs 80%; P = .01) and those with ≤2 mutations (25% vs 60.5%; P = .001), respectively (Table 2). The only clinical parameter that significantly differed between patients with and without a spleen response was platelet count (median, 283 × 109/L for responders vs median, 170 × 109/L for nonresponders; P = .010). Despite this correlation between platelet count and spleen response, neither average ruxolitinib dose intensity nor the rate G3/4 hematologic adverse events correlated with spleen response (supplemental Table 2). In a bivariate logistic regression model that included platelet count and number of mutations, only the number of mutations was significantly associated with spleen response. Patients with ≤2 mutations had ninefold higher odds of a spleen response than those with ≥3 mutations (OR = 9.37; 95% confidence interval [CI], 1.86-47.2).
Clinical characteristics stratified by type and number of mutations
| Characteristic . | Molecular risk signature . | Number of mutations (any) . | |||||
|---|---|---|---|---|---|---|---|
| No ASXL1, EZH2, IDH1/2 mutation (N = 68) . | ≥1 ASXL1, EZH2, IDH1/2 mutation (N = 27) . | P value . | ≤1 mutation (N = 53) . | 2 mutations (N = 30) . | ≥3 mutations (N = 12) . | P value . | |
| Age (years) | 66 (43-84) | 65 (41-80) | .525 | 65 (43-80) | 69 (56-70) | 64 (41-80) | .114 |
| Sex (female) | 28 (41) | 14 (52) | .369 | 21 (40) | 16 (53) | 5 (42) | .473 |
| Hg (g/dL), mean (range) | 10.8 (7.2-16.9) | 10.5 (8.2-13.7) | .499 | 10.7 (7.4-16.9) | 11.1 (8.6-16.7) | 9.7 (7.2-12.0) | .120 |
| WBC (109/L), mean (range) | 25 (2.7-152) | 26 (2.5-159) | .824 | 25 (3-152) | 21 (3-88) | 33 (24-159) | .518 |
| Plt (109/L), mean (range) | 367 (95-874) | 269 (13-637) | .043 | 363 (95-835) | 351 (103-969) | 206 (165-637) | .027 |
| Plt < 270 × 109/L | 30 (44) | 17 (63) | .115 | 22 (42) | 16 (53) | 9 (75) | .098 |
| PBBL, mean (range) | 1 (0-8) | 1.5 (0-7.0) | .003 | 0.7 (0-4) | 1.2 (0-8) | 1.6 (0-4) | .023 |
| PBBL ≥1% | 15 (22) | 11 (41) | .058 | 17 (32) | 15 (50) | 9 (75) | .017 |
| Baseline spleen size (cm), mean (range) | 18 (0-35) | 19 (3-30) | .732 | 20.0 (11-35) | 17.2 (3-29) | 21.5 (10-30) | .092 |
| Diagnosis | |||||||
| PMF | 33 (49) | 21 (78) | .032 | 26 (49) | 18 (60) | 10 (83) | .031 |
| PPV-MF | 26 (38) | 5 (18) | 23 (43) | 6 (20) | 2 (17) | ||
| PET-MF | 9 (13) | 1 (4) | 4 (8) | 6 (20) | 0 | ||
| Cytogenetics | |||||||
| Diploid | 36 (53) | 18 (67) | .429 | 23 (43) | 22 (73) | 9 (75) | .056 |
| Abnormal | 30 (44) | 8 (30) | 28 (53) | 7 (23) | 3 (25) | ||
| IM | 2 (3) | 1 (3) | 2 (4) | 1 (3) | 0 | ||
| Co-occurring mutations | |||||||
| TET2 (N = 14) | 10 (15) | 4 (15) | .608 | 0 | 10 (33) | 4 (33) | <.001 |
| JAK2 (N = 79) | 59 (87) | 20 (74) | .222 | 47 (88) | 24 (80) | 8 (67) | .157 |
| CALR (N = 9) | 5 (7) | 4 (15) | .622 | 3 (60) | 3 (50) | 3 (75) | .732 |
| Type 1 (N = 7) | |||||||
| Type 2 (N = 2) | |||||||
| Average dose intensity | .150 | .360 | |||||
| ≤10 mg BID | 14 (21) | 6 (22) | 11 (21) | 8 (27) | 1 (8) | ||
| >10 to ≤20 mg BID | 34 (50) | 8 (30) | 26 (49) | 12 (40) | 4 (33) | ||
| >20 mg BID | 20 (29) | 13 (48) | 16 (30) | 10 (33) | 7 (58) | ||
| G3/4 hematologic toxicities | |||||||
| G3/4 anemia/thrombocytopenia | 52 (76) | 18 (67) | .439 | 39 (74) | 23 (77) | 8 (67) | .801 |
| No G3/4 anemia/thrombocytopenia | 16 (24) | 9 (33) | .533 | 13 (25) | 7 (23) | 4 (33) | .830 |
| G3/4 anemia | 27 (40) | 7 (26) | 21 (40) | 9 (30) | 4 (33) | ||
| G3/4 thrombocytopenia | 13 (19) | 5 (19) | 10 (19) | 7 (23) | 1 (8) | ||
| G3/4 anemia and thrombocytopenia | 12 (18) | 6 (22) | 8 (15) | 7 (23) | 3 (25) | ||
| Spleen response (N = 88) | |||||||
| <50% reduction | 12 (20) | 13 (48) | .01 | 10 (21) | 6 (21) | 9 (75) | .001 |
| ≥50% reduction | 49 (80) | 14 (52) | 37 (79) | 23 (79) | 3 (25) | ||
| 0-24% spleen red | 5 (8) | 9 (33) | .009 | 5 (11) | 4 (14) | 5 (42) | .03 |
| 25-100% spleen red | 56 (92) | 18 (67) | 42 (89) | 25 (86) | 7 (58) | ||
| Median IWG SR duration (weeks) (N = 63) | 39.7 (2.8-68.5) | 14.3 (4.6-74.2) | .212 | 41.4 (3.0-68.5) | 22.2 (2.8-74.2) | 6.6 (6.5-6.6) | .080 |
| Median TTD (weeks) | 214 (7-369) | 96 (9-387) | <.001 | 218 (7-369) | 162 (17-387) | 58 (11-137) | .001 |
| Characteristic . | Molecular risk signature . | Number of mutations (any) . | |||||
|---|---|---|---|---|---|---|---|
| No ASXL1, EZH2, IDH1/2 mutation (N = 68) . | ≥1 ASXL1, EZH2, IDH1/2 mutation (N = 27) . | P value . | ≤1 mutation (N = 53) . | 2 mutations (N = 30) . | ≥3 mutations (N = 12) . | P value . | |
| Age (years) | 66 (43-84) | 65 (41-80) | .525 | 65 (43-80) | 69 (56-70) | 64 (41-80) | .114 |
| Sex (female) | 28 (41) | 14 (52) | .369 | 21 (40) | 16 (53) | 5 (42) | .473 |
| Hg (g/dL), mean (range) | 10.8 (7.2-16.9) | 10.5 (8.2-13.7) | .499 | 10.7 (7.4-16.9) | 11.1 (8.6-16.7) | 9.7 (7.2-12.0) | .120 |
| WBC (109/L), mean (range) | 25 (2.7-152) | 26 (2.5-159) | .824 | 25 (3-152) | 21 (3-88) | 33 (24-159) | .518 |
| Plt (109/L), mean (range) | 367 (95-874) | 269 (13-637) | .043 | 363 (95-835) | 351 (103-969) | 206 (165-637) | .027 |
| Plt < 270 × 109/L | 30 (44) | 17 (63) | .115 | 22 (42) | 16 (53) | 9 (75) | .098 |
| PBBL, mean (range) | 1 (0-8) | 1.5 (0-7.0) | .003 | 0.7 (0-4) | 1.2 (0-8) | 1.6 (0-4) | .023 |
| PBBL ≥1% | 15 (22) | 11 (41) | .058 | 17 (32) | 15 (50) | 9 (75) | .017 |
| Baseline spleen size (cm), mean (range) | 18 (0-35) | 19 (3-30) | .732 | 20.0 (11-35) | 17.2 (3-29) | 21.5 (10-30) | .092 |
| Diagnosis | |||||||
| PMF | 33 (49) | 21 (78) | .032 | 26 (49) | 18 (60) | 10 (83) | .031 |
| PPV-MF | 26 (38) | 5 (18) | 23 (43) | 6 (20) | 2 (17) | ||
| PET-MF | 9 (13) | 1 (4) | 4 (8) | 6 (20) | 0 | ||
| Cytogenetics | |||||||
| Diploid | 36 (53) | 18 (67) | .429 | 23 (43) | 22 (73) | 9 (75) | .056 |
| Abnormal | 30 (44) | 8 (30) | 28 (53) | 7 (23) | 3 (25) | ||
| IM | 2 (3) | 1 (3) | 2 (4) | 1 (3) | 0 | ||
| Co-occurring mutations | |||||||
| TET2 (N = 14) | 10 (15) | 4 (15) | .608 | 0 | 10 (33) | 4 (33) | <.001 |
| JAK2 (N = 79) | 59 (87) | 20 (74) | .222 | 47 (88) | 24 (80) | 8 (67) | .157 |
| CALR (N = 9) | 5 (7) | 4 (15) | .622 | 3 (60) | 3 (50) | 3 (75) | .732 |
| Type 1 (N = 7) | |||||||
| Type 2 (N = 2) | |||||||
| Average dose intensity | .150 | .360 | |||||
| ≤10 mg BID | 14 (21) | 6 (22) | 11 (21) | 8 (27) | 1 (8) | ||
| >10 to ≤20 mg BID | 34 (50) | 8 (30) | 26 (49) | 12 (40) | 4 (33) | ||
| >20 mg BID | 20 (29) | 13 (48) | 16 (30) | 10 (33) | 7 (58) | ||
| G3/4 hematologic toxicities | |||||||
| G3/4 anemia/thrombocytopenia | 52 (76) | 18 (67) | .439 | 39 (74) | 23 (77) | 8 (67) | .801 |
| No G3/4 anemia/thrombocytopenia | 16 (24) | 9 (33) | .533 | 13 (25) | 7 (23) | 4 (33) | .830 |
| G3/4 anemia | 27 (40) | 7 (26) | 21 (40) | 9 (30) | 4 (33) | ||
| G3/4 thrombocytopenia | 13 (19) | 5 (19) | 10 (19) | 7 (23) | 1 (8) | ||
| G3/4 anemia and thrombocytopenia | 12 (18) | 6 (22) | 8 (15) | 7 (23) | 3 (25) | ||
| Spleen response (N = 88) | |||||||
| <50% reduction | 12 (20) | 13 (48) | .01 | 10 (21) | 6 (21) | 9 (75) | .001 |
| ≥50% reduction | 49 (80) | 14 (52) | 37 (79) | 23 (79) | 3 (25) | ||
| 0-24% spleen red | 5 (8) | 9 (33) | .009 | 5 (11) | 4 (14) | 5 (42) | .03 |
| 25-100% spleen red | 56 (92) | 18 (67) | 42 (89) | 25 (86) | 7 (58) | ||
| Median IWG SR duration (weeks) (N = 63) | 39.7 (2.8-68.5) | 14.3 (4.6-74.2) | .212 | 41.4 (3.0-68.5) | 22.2 (2.8-74.2) | 6.6 (6.5-6.6) | .080 |
| Median TTD (weeks) | 214 (7-369) | 96 (9-387) | <.001 | 218 (7-369) | 162 (17-387) | 58 (11-137) | .001 |
IM, not measurable.
TTD
As might be expected, patients with a spleen response also had a longer TTD (the length of time the patient received ruxolitinib on the study; P < .001). As of this report, 68 of the 95 patients have discontinued therapy, 20 patients are still receiving ruxolitinib on study, and 7 patients withdrew consent to obtain a commercial supply of ruxolitinib and are lost to follow-up. Detailed reasons for discontinuation of therapy for most patients (n = 48) were previously reported10 ; the additional 20 patients who discontinued therapy since the last report did so due to relapse/progression, other medical reasons, or death. No new toxicities have been observed in patients on long-term ruxolitinib therapy. Baseline clinical variables that were associated with shorter TTD included lower platelet count (P = .037), peripheral blood blasts ≥1% (P = .02), transfusion dependence at baseline (P = .005), and diagnosis of primary MF (PMF) (P = .006) (Table 3). These findings suggest that anemia and/or thrombocytopenia may have prevented patients from receiving an optimal dose of ruxolitinib. Indeed, we found that for patients receiving an average dose of ≤10 mg twice per day (BID), the median platelet count was significantly lower than for those receiving an average dose >20 mg BID (median, 160 × 109/L vs 298 × 109/L, respectively; P < .001). However, there was no difference in average hemoglobin levels by dose level (P = .386), and neither average ruxolitinib dose intensity nor grade 3/4 hematologic adverse events were associated with TTD (Table 3).
Factors associated with TTD
| Characteristic . | Median TTD, weeks (range) . | HR . | 95% CI . | P value . |
|---|---|---|---|---|
| Platelets | ||||
| ≥270 × 109/L | 222 (194-250) | Reference | ||
| <270 × 109/L | 103 (50-156) | 1.80 | 1.11-2.92 | .017 |
| Peripheral blood blasts | ||||
| <1% | 201 (164-238) | Reference | ||
| ≥1% | 103 (26-181) | 1.70 | 1.05-2.75 | .030 |
| Transfusion dependence | 62 (14-110) | 2.05 | 1.21-3.47 | .008 |
| Baseline spleen size (cm)* | 0.99 | 0.95-1.04 | .638 | |
| Diagnosis | ||||
| PPV-MF (N = 28) | 240 (93-387) | Reference | ||
| PMF (N = 52) | 119 (70-169) | 1.48 | 1.06-2.17 | .033 |
| PET-MF (N = 8) | 211 (165-257) | 1.00 | 0.587-1.70 | .994 |
| DIPSS | ||||
| Low/Int-1 (N = 39) | 178 (116-240) | |||
| Int-2/High (N = 49) | 142 (47-237) | 1.13 | 0.70-1.83 | .618 |
| ASXL1+ (N = 19) | 51 (42-60) | 4.19 | 2.39-7.34 | <.001 |
| EZH2+ (N = 7) | 65 (29-101) | 3.97 | 1.71-9.07 | .002 |
| GATA2+ (N = 3) | 60 (39-81) | 2.88 | 0.8869.36 | .127 |
| ≥1 mutation in ASXL1, EZH2, IDH1/2 (N = 26) | 55 (43-67) | 3.02 | 1.81-5.03 | <.001 |
| ≥1 mutation in ASXL1, DNMT3A, or EZH2 (N = 22) | 51 (41-61) | 4.61 | 2.661-7.9 | <.001 |
| Number of mutations | ||||
| ≤1 (N = 48) | 217 (165-269) | Reference | ||
| 2 (N = 28) | 142 (21-263) | 1.71 | 1.00-2.90 | .049 |
| ≥3 (N = 12) | 55 (40-70) | 5.74 | 2.74-12.1 | <.001 |
| Average dose intensity | ||||
| ≤10 mg BID (N = 20) | 96 (37-155) | Reference | .365 | |
| >10 to ≤20 mg BID (N = 39) | 189 (161-217) | 0.798 | 0.431-1.48 | |
| >20 mg BID (N = 28) | 119 (26-212) | 1.18 | 0.627-2.32 | |
| Average dose intensity* | 1.03 | 0.997-1.068 | .071 | |
| G3/4 anemia/thrombocytopenia (N = 66) | 166 (55-277) vs 154 (74-233) | .454 | ||
| No G3/4 anemia OR thrombocytopenia (N = 21) | 166 (55-277) | Reference | .396 | |
| G3/4 anemia (N = 31) | 188 (87-289) | 0.942 | 0.505-1.76 | |
| G3/4 thrombocytopenia (N = 18) | 189 (158- 220) | 0.713 | 0.333-1.53 | |
| G3/4 anemia and thrombocytopenia (N = 18) | 96 (11-181) | 1.324 | 0.667-2.63 | |
| IWG spleen response (N = 57) | 51 (31-71) | Reference | ||
| 217 (181-253) | 0.281 | 0.164-0.481 | <.001 |
| Characteristic . | Median TTD, weeks (range) . | HR . | 95% CI . | P value . |
|---|---|---|---|---|
| Platelets | ||||
| ≥270 × 109/L | 222 (194-250) | Reference | ||
| <270 × 109/L | 103 (50-156) | 1.80 | 1.11-2.92 | .017 |
| Peripheral blood blasts | ||||
| <1% | 201 (164-238) | Reference | ||
| ≥1% | 103 (26-181) | 1.70 | 1.05-2.75 | .030 |
| Transfusion dependence | 62 (14-110) | 2.05 | 1.21-3.47 | .008 |
| Baseline spleen size (cm)* | 0.99 | 0.95-1.04 | .638 | |
| Diagnosis | ||||
| PPV-MF (N = 28) | 240 (93-387) | Reference | ||
| PMF (N = 52) | 119 (70-169) | 1.48 | 1.06-2.17 | .033 |
| PET-MF (N = 8) | 211 (165-257) | 1.00 | 0.587-1.70 | .994 |
| DIPSS | ||||
| Low/Int-1 (N = 39) | 178 (116-240) | |||
| Int-2/High (N = 49) | 142 (47-237) | 1.13 | 0.70-1.83 | .618 |
| ASXL1+ (N = 19) | 51 (42-60) | 4.19 | 2.39-7.34 | <.001 |
| EZH2+ (N = 7) | 65 (29-101) | 3.97 | 1.71-9.07 | .002 |
| GATA2+ (N = 3) | 60 (39-81) | 2.88 | 0.8869.36 | .127 |
| ≥1 mutation in ASXL1, EZH2, IDH1/2 (N = 26) | 55 (43-67) | 3.02 | 1.81-5.03 | <.001 |
| ≥1 mutation in ASXL1, DNMT3A, or EZH2 (N = 22) | 51 (41-61) | 4.61 | 2.661-7.9 | <.001 |
| Number of mutations | ||||
| ≤1 (N = 48) | 217 (165-269) | Reference | ||
| 2 (N = 28) | 142 (21-263) | 1.71 | 1.00-2.90 | .049 |
| ≥3 (N = 12) | 55 (40-70) | 5.74 | 2.74-12.1 | <.001 |
| Average dose intensity | ||||
| ≤10 mg BID (N = 20) | 96 (37-155) | Reference | .365 | |
| >10 to ≤20 mg BID (N = 39) | 189 (161-217) | 0.798 | 0.431-1.48 | |
| >20 mg BID (N = 28) | 119 (26-212) | 1.18 | 0.627-2.32 | |
| Average dose intensity* | 1.03 | 0.997-1.068 | .071 | |
| G3/4 anemia/thrombocytopenia (N = 66) | 166 (55-277) vs 154 (74-233) | .454 | ||
| No G3/4 anemia OR thrombocytopenia (N = 21) | 166 (55-277) | Reference | .396 | |
| G3/4 anemia (N = 31) | 188 (87-289) | 0.942 | 0.505-1.76 | |
| G3/4 thrombocytopenia (N = 18) | 189 (158- 220) | 0.713 | 0.333-1.53 | |
| G3/4 anemia and thrombocytopenia (N = 18) | 96 (11-181) | 1.324 | 0.667-2.63 | |
| IWG spleen response (N = 57) | 51 (31-71) | Reference | ||
| 217 (181-253) | 0.281 | 0.164-0.481 | <.001 |
Analyzed as a continuous variable by Cox regression.
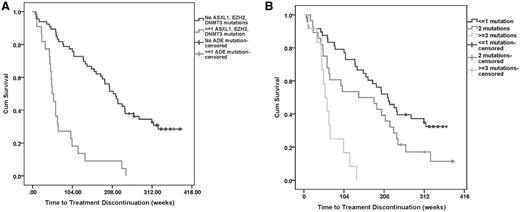
Patients with PMF had a significantly shorter TTD than those with PPV-MF (HR = 1.52; 95% CI, 1.06-2.17; P = .022). In addition, a significantly larger proportion of patients with PMF and fewer patients with PPV-MF had ≥3 mutations (P = .031). Baseline spleen size and dynamic international prognostic scoring system (DIPSS) score were not associated with TTD. Individually, ASXL1, DNMT3A, and EZH2 but not IDH1/2 were associated with shorter TTD (Table 3). However, all 3 DNMT3A mutations co-occurred with ASXL1, so the prognostic relevance of DNMT3A on its own is not known. Patients with 1 or more mutation in ASXL1, DNMT3A, or EZH2 had a fourfold higher hazard of treatment discontinuation than those without at least 1 of these mutations (P < .001; Figure 2A). In addition, patients with ≥3 mutations of any type had a nearly sixfold higher hazard of treatment discontinuation than those with ≤1 mutation (P < .001; Figure 2B). In multivariable analysis, only number of mutations (HR for ≥3 mutations = 3.63; 95% CI, 1.49-8.81; P = .005) and spleen response (HR = 0.380; 95% CI, 0.183-0.789; P = .009) remained associated with TTD (Table 4). A summary of the 12 patients with ≥3 mutations is shown in supplemental Table 3. Patients with 1 or more ASXL1, EZH2, or IDH1/2 mutations (HR = 3.82; 95% CI, 2.18-6.68) and those with ≥3 mutations also had shorter OS (HR = 5.97; 95% CI, 2.81-12.65; P < .001) (supplemental Table 4). Because only 7 patients had transformation to AML, we could not statistically analyze the effects of mutations on leukemia-free survival. However, notably, 1 of the patients who transformed to AML had an IDH2 mutation and 2 had ASXL1 and/or EZH2 mutations.
Kaplan-Meier analysis of time to event outcomes. Time to treatment failure stratified by (A) molecular risk group and (B) number of mutations.
Kaplan-Meier analysis of time to event outcomes. Time to treatment failure stratified by (A) molecular risk group and (B) number of mutations.
Multivariable Cox regression analysis of TTD
| Variable . | HR . | 95% CI . | P value . |
|---|---|---|---|
| Number of mutations | |||
| ≤1 | Reference | ||
| 2 | 2.56 | 1.35-4.86 | .004 |
| ≥3 | 3.74 | 1.53-9.10 | .004 |
| Transfusion dependence | 1.65 | 0.823-3.31 | .158 |
| Diagnosis | |||
| PPV-MF | Reference | ||
| PMF | 1.85 | 0.959-3.57 | .066 |
| IWG-defined spleen response | 0.372 | 0.179-0.776 | .008 |
| Variable . | HR . | 95% CI . | P value . |
|---|---|---|---|
| Number of mutations | |||
| ≤1 | Reference | ||
| 2 | 2.56 | 1.35-4.86 | .004 |
| ≥3 | 3.74 | 1.53-9.10 | .004 |
| Transfusion dependence | 1.65 | 0.823-3.31 | .158 |
| Diagnosis | |||
| PPV-MF | Reference | ||
| PMF | 1.85 | 0.959-3.57 | .066 |
| IWG-defined spleen response | 0.372 | 0.179-0.776 | .008 |
Bold text highlights variables that remained statistically significant in the multivariate model.
Long-term responders
At the time of this report, 20 patients are still being treated with ruxolitinib after a median of 6.4 years (range, 4.8-7.4 years). Of these 20 patients, 12 (60%) have PPV-MF, 7 (35%) have PMF, and 1 has PET-MF (5%). These proportions are significantly different than those of the entire cohort, where 25% had PPV-MF and 63% had PMF (P = .013). None of the patients still taking ruxolitinib have >2 mutations: 16 (80%) have only 1 mutation and 4 (20%) have 2 mutations (P = .031). Not surprisingly, 19 of 20 (95%) had a spleen response compared with 3 of 12 (25%) of those with ≥3 mutations. Eighteen of the 20 (90%) patients still being treated harbor no ASXL1, DNMT3A, EZH2, or IDH1/2 mutations, whereas only 1 of 12 (8%) of those with ≥3 mutations had none of these mutations (P < .001). There were no significant differences in clinical parameters (age, hemoglobin, platelet count, white blood cell count, peripheral blood blasts, transfusion dependence, baseline spleen size, or DIPSS score) between patients with ≥3 mutations and those still being treated (data not shown).
Discussion
We identified mutations in 15 genes commonly mutated in myeloid malignancies in all but 2 patients in our cohort. Patients with ≥3 mutations of any type had significantly lower odds of a spleen response and a shorter TTD. In multivariate analysis, only the presence ≥2 mutations and spleen response were associated with shorter TTD. These findings suggest that patients with ≥3 mutations have a more aggressive disease that is less amenable to treatment with ruxolitinib.
In agreement with previous findings showing that ASXL1, EZH2, and IDH1/2 are associated with poor outcomes, we also found that patients with one or more mutations in ASXL1, EZH2, or IDH1/2 had shorter TTD and OS.1,19,26 In contrast to the analysis of mutations in patients in the COMFORT-II cohort, we found that patients with 1 or more mutations in ASXL1, EZH2, or IDH1/2 were significantly less likely to have a spleen response. One reason for this discrepancy could be the differences in the combinations of mutations assessed in the 2 studies. For our cohort, we did not have information on the SRSF2 mutation status, which was included as a high-molecular risk mutation in the study by Guglielmelli et al.1 In addition, we analyzed best overall spleen response, whereas Guglielmelli et al analyzed spleen response after 24 and 48 weeks. Thus, our cohort includes IWG-defined responses that may have occurred at later time points. Indeed, a long-term follow-up analysis of the phase 1/2 study reported a spleen response rate of 62% after a median follow-up of 32 months compared with a spleen response rate of 44% after 12 weeks.7,10 Likewise, after a median follow-up of 3 years, 59% percent of patients in the COMFORT-I cohort had achieved a spleen response compared with 42% at week 24.27
We also identified mutations in genes that are part of the mitogen-activated protein kinase/Ras pathway (KRAS, NRAS, and PTPN11) in 9 patients (10%). Three of 4 KRAS/NRAS mutations were found at residue G12 or G13, a mutational hotspot in Ras proteins that leads to oncogenic activation.28 Activating NRAS/KRAS mutations have been found in 2% to 5% of PMF patients and are reported to be associated with poor prognosis.3 We observed a trend toward shorter survival for these patients (P = .052), but our sample size was small. The fourth patient had a KRAS I36M mutation, which has been reported in patients with Noonan syndrome, an autosomal dominant disorder associated with dysmorphic facial features, short stature, heart disease, skeletal abnormalities, and predisposition to juvenile myelomonocytic leukemia (JMML), acute lymphoblastic leukemia (ALL), and AML.12
Three patients had mutations in PTPN11, encoding a phosphatase that signals upstream of KRAS/NRAS. To our knowledge, somatic mutations in PTPN11 have only been reported in 4 MPN patients, 1 of whom had transformed to AML.16,29 Somatic PTPN11 mutations (P491) have been described in patients with JMML and pediatric AML and ALL,30,31 and germ-line mutations (F71 and D106) have been reported in patients with JMML and >50% of those with Noonan syndrome.32,33 The 3 patients harboring KRAS/PTPN11 mutations found in patients with Noonan syndrome reported a history of stroke (2 patients; KRAS I36M and PTPN1 1F71) and mitral and tricuspid valve regurgitation (1 patient; PTPN11 D106 mutation), but none of them displayed any obvious signs of Noonan syndrome. A history of bleeding problems and congenital heart defects are common symptoms of Noonan syndrome, suggesting that these may indeed be germ-line mutations. Regardless, given the role of Ras and PTPN11 mutations in pediatric myeloid malignancies and Noonan syndrome, the mutation likely contributes to the MPN phenotype in some patients.3
Three patients had mutations in GATA2, which have been reported in a group of autosomal dominant immune dysfunctions involving the myeloid lineage, which have recently been grouped together as GATA2 deficiencies. To our knowledge somatic GATA2 mutations have only been reported in 1 MPN patient.22 Given the link between germ-line GATA2 mutations and myeloid malignancies, as well as its absence in recently published whole-genome studies,4 it is plausible that the mutations identified in GATA2 in these patients represent germ-line mutations. Two of the 3 patients with GATA2 mutations had in-frame deletions, which to our knowledge have not been previously reported in MPNs. Although the functional relevance of these deletions is not known, the amino acid residues deleted (K389 and K390) are predicted to be sumoylation sites.34 None of these patients showed any evidence of chronic immune dysfunctions.
Fourteen patients in our cohort had TET2 mutations, 9 of which co-occurred with the JAK2 mutation. In our cohort, TET2 was not associated with TTF or OS, but was associated with older age (mean, 69 vs 66 years; P = .039), as reported previously.35 Studies of the prognostic relevance of TET2 mutations are conflicting,22,35 but a recently published study suggests that the order in which the JAK2 and TET2 mutations are acquired has important prognostic relevance.36 Indeed, the authors reported that patients who acquired TET2 first were older than those who acquired JAK2 first and also that ruxolitinib inhibits proliferation of cells that acquire JAK2 first, but not those that acquire TET2 first. This may explain why studies of the prognostic relevance of TET2 have been ambiguous.
Among the 12 patients with ≥3 mutations, only 2 had >3 mutations (one had 4 and the other had 6), which is consistent with previous findings that the majority of patients with MF have 2 or fewer mutations.19,22 Notably, 10 (83%) had PMF and 2 (17%) had PPV-MF. In addition, 11 (92%) patients had ≥1 ASXL1, EZH2, or IDH1/2 mutation (25% had both ASXL1 and EZH2 mutations). However, the hazard of TTD in patients with ≥3 of any mutation (HR = 5.74) was nearly twofold higher than for those with 1 or more ASXL1, EZH2, or IDH1/2 mutations (HR = 3.02), suggesting that mutations in other genes, such as GATA2, KRAS, NRAS, TP53, and PTPN11 (all of which were present in patients with ≥3 mutations), also confer a prognostic disadvantage. Interestingly, NRAS, KRAS, RUNX1, TP53, GATA2, and DNMT3A mutations were only observed in patients with PMF.
In summary, using a targeted NGS approach, we identified mutations in 15 genes frequently mutated in hematologic malignancies in patients with MF who were treated with ruxolitinib in a phase 1/2 study. We found that the presence of mutations previously associated with a negative prognosis, as well as the total number of mutations, was inversely correlated with spleen response and TTD. Patients with ≥3 mutations, although only 12% of our cohort, had the worst outcomes, suggesting that multigene profiling to identify prognostically detrimental mutations should eventually be included as part of not only diagnostic work up but also therapeutic planning for MF. Targeted NGS panels such as the one presented here are feasible for diagnosis and disease monitoring in the clinic.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This research was supported by funds from the University Cancer Foundation via the Sister Institution Network Fund at the University of Texas MD Anderson Cancer Center, and in part by a Cancer Center Support Grant from National Institutes of Health, National Cancer Institute grant CA016672 to The University of Texas MD Anderson Cancer Center.
Authorship
Contribution: S.V. and K.P.P. designed the study, analyzed and interpreted data, and wrote and approved the manuscript; K.J.N analyzed and interpreted the data and wrote the manuscript; R.L. performed the sequencing, analyzed the data, and approved the manuscript; S.P. collected the data and approved the manuscript; E.J., J.C., and H.K. provided clinical care to patients and approved the manuscript; R.S., M.M., M.J.R., and M.L. performed the sequencing, analyzed the data, and approved the manuscript; T.M. collected and prepared the samples and approved the manuscript; and F.P.S. interpreted data and wrote and approved the manuscript.
Conflict-of-interest disclosure: S.V. has received research funding from Incyte Corporation for the conduct of clinical trials. All other authors declare no competing financial interests.
Correspondence: Srdan Verstovsek, 1515 Holcombe Blvd, Unit 428, Houston, TX 77030; e-mail: sverstov@mdanderson.org.