Abstract

Background: Midostaurin (M) is a multi-targeted small molecule FLT3 inhibitor which has single agent activity in both internal tandem duplication (ITD) and tyrosine kinase domain (TKD) mutant FLT3 AML. The objective of this global rand phase III trial was to determine if the addition of M to ind and consol therapy followed by one year of maint would improve overall survival (OS) compared to standard chemotherapy in younger adults with activating FLT3 muts.
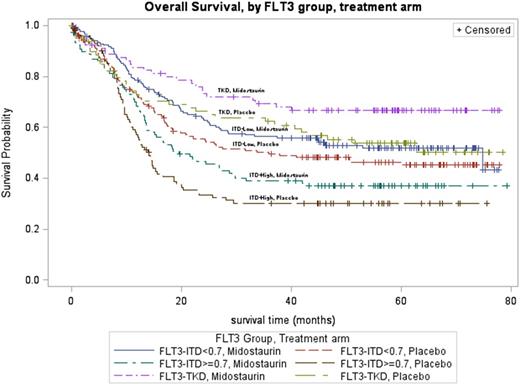
Methods: Between May 2008 and October 2011, 3279 previously untreated AML pts age 18-60 (exclusive of acute promyelocytic leukemia) in 225 sites/17 countries were screened for FLT3 muts at one of 7 academic labs (subject to extensive assay cross-validation). Hydroxyurea was allowed for up to 5 d prior to beginning ind therapy while awaiting results of mut testing. Pts were rand for the duration of therapy to M or P stratified by FLT3 mut subtype (TKD v ITD high allelic mut fraction (>0.7) vs low mut fraction (0.05-0.7). Ind therapy consisted of D 60 mg/m2 IV d1-3 and C 200 mg/m2 d1-7 CIV plus M or P (50 mg po bid, d 8-22). Re-treatment with a second blinded course was allowed if residual AML was noted on a d 21 marrow exam. Pts achieving complete remission (CR) received 4 cycles of C 3g/m2 over 3h q 12h on days 1, 3, and 5 plus M or P (50 mg po bid, d 8-22) followed by a year of maint therapy with M or P (50 mg po bid). Transplantation (SCT) was allowed. With a sample size of 717 pts, the trial was powered to detect an improvement from 16.3 (P) to 20.9 (M) months in median OS (HR = 0.78) using a one-sided alpha of 0.025 and power of 84%. The final analysis was to occur after 509 deaths, but given the slow rate of events (359 deaths by April 2015), the trial was amended to change the timing of the OS analysis, and promote event free survival (EFS, defined as the earliest of death, relapse, or no CR within 61 d of the start of ind) as a key secondary endpoint. The critical value for this primary analysis is set at 0.02286 (1-sided) accounting for the alpha spent at the interim analysis (0.5%). Support: U10CA180821, U10CA180882, CA31946, Novartis
Results: 717 pts (341 FLT3 ITD-Low, 214 FLT3 ITD-High; 162 FLT3 TKD) were rand to either M (n=360) or P (n=357). There were no significant differences between the arms in age (median, 48y), race, FLT3 subtype, or baseline CBC except for gender (M, 48.2% male; P, 40.6% male; p=.04). All pts are off active treatment, with a median follow-up of 57 months for surviving pts. No statistically significant differences were observed in the overall rate of grade 3 or higher hematologic or non-hematologic adverse events (AEs) between M and P (regardless of attribution). A total of 37 grade 5 AEs were reported (M, 5.3%; P, 5.0%; p=1.0). No differences in treatment-related grade 5 AEs were observed (M, 3.1%; P, 2.5%; p=0.82).
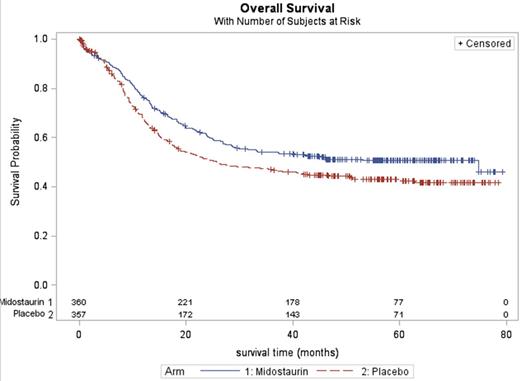
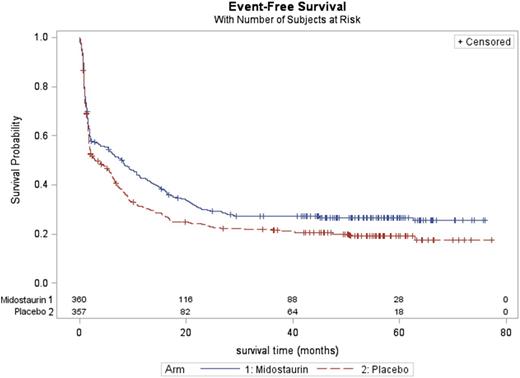
CR rate is 59% (M) and 54% (P) (p=0.18). The HRs comparing M to P for OS is 0.77 (one-sided p = 0.007; Figure 1), and for EFS is 0.80 (one-sided p = 0.004; Figure 2).
402/717 (57%) pts received an allogeneic SCT (M, 58%; P, 54%) at any time; 177/717 (25%) in CR1 (M, 27%; P, 22%). Median time to allogeneic SCT was similar on each arm (M, 5.0 months; P, 4.6; p=0.23). Secondary analyses for OS and EFS censoring at the time of SCT provided similar results (Table). The benefit of M was consistent across all FLT3 subgroups for both EFS and OS (Figure 3).
Conclusions: The C10603 trial demonstrated that a prospective trial in a pre-therapy genetically defined subgroup of AML pts was feasible and that the addition of the multi-kinase inhibitor M to standard chemotherapy and for one year of maint therapy significantly improved EFS and OS (in both uncensored and censored for transplant analyses) in pts whose blasts had a TKD or ITD (low or high FLT3 mut burden). These findings may lead to improved outcomes through the use of M as a component of therapy in younger adults with mutant FLT3 AML.
| . | Arm . | Median, mos (95% CI) . | p-value 1 . | 5-year Event rate % (95% CI) . | HR2 (95% CI) . |
|---|---|---|---|---|---|
| OS | M | 74.7 (31.5, * ) | 0.007 | 50.8 (45.4-55.9) | 0.77 (0.63, 0.95) |
| P | 26.0 (18.5, 46.5) | 43.1 (37.6-48.4) | |||
| OS, SCT censored | M | * (*,*) | 0.047 | 62.6 (54.6-69.7) | 0.77 (0.56,1.05) |
| P | * (36.9, *) | 54.9 (46.2-62.8) | |||
| EFS | M | 8.0 (5.3, 10.6) | 0.0044 | 26.7 (22.2-31.5) | 0.80 (0.67, 0.95) |
| P | 3.0 (1.9, 5.8) | 19.1 (15.1-23.6) | |||
| EFS, SCT censored | M | 8.2 (5.5, 10.7) | 0.025 | 24.2 (18.9-29.8) | 0.84 (0.70, 1.0020) |
| P | 3.0 (1.9, 5.8) | 21.8 (16.8-27.3) |
| . | Arm . | Median, mos (95% CI) . | p-value 1 . | 5-year Event rate % (95% CI) . | HR2 (95% CI) . |
|---|---|---|---|---|---|
| OS | M | 74.7 (31.5, * ) | 0.007 | 50.8 (45.4-55.9) | 0.77 (0.63, 0.95) |
| P | 26.0 (18.5, 46.5) | 43.1 (37.6-48.4) | |||
| OS, SCT censored | M | * (*,*) | 0.047 | 62.6 (54.6-69.7) | 0.77 (0.56,1.05) |
| P | * (36.9, *) | 54.9 (46.2-62.8) | |||
| EFS | M | 8.0 (5.3, 10.6) | 0.0044 | 26.7 (22.2-31.5) | 0.80 (0.67, 0.95) |
| P | 3.0 (1.9, 5.8) | 19.1 (15.1-23.6) | |||
| EFS, SCT censored | M | 8.2 (5.5, 10.7) | 0.025 | 24.2 (18.9-29.8) | 0.84 (0.70, 1.0020) |
| P | 3.0 (1.9, 5.8) | 21.8 (16.8-27.3) |
1Stratified on FLT3 subtype; one-sided, log-rank p-value.
2Cox model stratified on FLT3 subtype.
*= not attained
Stone:Celgene: Consultancy; Sunesis: Consultancy, Other: DSMB for clinical trial; Novartis: Research Funding; Amgen: Consultancy; Agios: Consultancy; Roche/Genetech: Consultancy; Merck: Consultancy; Pfizer: Consultancy; AROG: Consultancy; Celator: Consultancy; Juno: Consultancy; Abbvie: Consultancy; Karyopharm: Consultancy. Off Label Use: midostaurin- FLT 3 inhibitor. Thiede:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; AgenDix GmBH: Equity Ownership. Niederwieser:Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Medeiros:Celgene: Honoraria, Research Funding; Agios Pharmaceuticals: Honoraria. Schlenk:Daiichi Sankyo: Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria, Research Funding; Arog: Honoraria, Research Funding; Teva: Honoraria, Research Funding; Boehringer-Ingelheim: Honoraria; Janssen: Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Research Funding. Larson:Novartis: Consultancy, Research Funding; Bristol-Myers Squibb: Consultancy; Ariad: Consultancy, Research Funding; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal