Abstract
For SAA patients (pts) lacking an HLA identical donor, outcomes of HSCT using single or dual unrelated cord blood (UCB) transplants or haplo-identical donors have been associated with high graft failure rates and poor survival. We investigated whether co-infusion of a single UCB unit with CD34+ selected cells from a haplo-identical relative following a highly immunosuppressive conditioning could improve transplant outcome for this high-risk population.
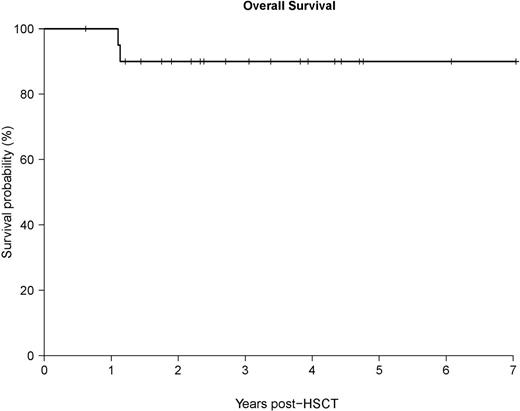
Methods: Eligible pts for HSCT were required to be between the ages of 4-55, have a diagnosis of SAA or SAA evolved to MDS, be unresponsive to immunosuppressive therapy, have severe neutropenia (ANC<500 cells/µL), lack an HLA-matched donor, have an available haploidentical family member, and at least one ≥ 4/6 HLA-matched UCB unit with a minimum TNC dose ≥1.5x107 cells/kg. Pts received conditioning with cyclophosphamide (120 mg/kg), fludarabine (125 mg/m2), equine-ATG (160 mg/kg) and 200 cGy of total body irradiation. On Day 0, pts received a CD34-selected (Miltenyi CliniMacs) G-CSF mobilized haplo-donor allograft combined with a single UCB. Tacrolimus and MMF were used for GVHD prophylaxis. Results: 21 pts (median age: 19.6 yrs, range: 4.5-48.6) including 14 with SAA and 7 with SAA that evolved to early stage MDS (< 5% blasts) underwent haplo-cord transplant. 14 pts received 4/6, and seven pts received a 5/6 HLA-matched UCB unit. UCB units contained a median 3.77x107 TNCs/kg (range: 1.96-6.93), a median 1.54x105 CD34+ cells/kg (range 0.46-3.45), and the haplo-graft contained a median 3.2x106 CD34+ cells/kg (range: 3.0-4.1) and a median 0.95x103 CD3+ cells/kg (range 0.3-5.04). All 21 pts engrafted, which was sustained and associated with transfusion independence in 20/21 pts. At a median follow-up of 3 yrs (1116 days, range: 226-2572), 19/21 pts survive for an overall survival rate of 90%. 2 pts died at day 414 and 402 post-HSCT from viral related complications (CMV pneumonitis and limbic encephalopathy). Neutrophil and platelet recovery occurred at a median 10 (range: 9-22), and 30 (range: 16-129) days respectively. Cord myeloid engraftment (cord ANC>500 cells/µl, calculated from chimerism data) occurred in 18/21 pts at a median 42 days while 3/21 did not achieve a cord ANC>500 but had haplo-donor engraftment which was sustained in 2 cases. The cumulative incidence of grade II-IV acute GVHD (aGVHD) was 28.6%, with only 1 pt (4.8%) developing grade III and no cases of grade IV or steroid refractory aGVHD. The cumulative incidence of chronic GVHD (cGVHD) was 47.8%, with 37% mild, 11% moderate, and no severe cGVHD. Engraftment profiles showed 16 achieved full cord chimerism in all cell lineages, 2 remained mixed haplo-cord chimeras, and 2 failed to have UCB engraftment but had sustained 100% haplo-donor myeloid chimerism. Higher degrees of HLA matching between recipient and UCB unit were associated with faster rates of cord engraftment (P=0.012) and the achievement of full cord chimerism (P= 0.004). Among the 16 pts who had lower degrees of HLA matching (≤5/8 HLA alleles) between the recipient and UCB unit, 9 received grafts with KIR ligand incompatibility in the haplo vs. cord direction ( defined as the presence of a KIR ligand in the haplo-donor graft that was absent in the UCB unit at HLA epitopes Bw4, HLA-C Groups 1 & 2, HLA-A3, and HLA-A11); KIR ligand incompatibility had a negative impact on cord myeloid engraftment as 6/9 (67%) of these pts failed to achieve full cord myeloid chimerism by day 400 and 5/9 (56%) pts failed to achieve a cord ANC>500 by day 250 post-HSCT. In contrast, cord myeloid engraftment occurred quicker in the 12 pts who did not have haplo vs. cord KIR ligand incompatibility including 7 pts with lower degrees of HLA matching (≤5/8 HLA alleles between the recipient and UCB) and 5 pts with higher degrees of HLA matching, where the median times to achieve a cord ANC>500 and full cord myeloid chimerism was 42 days (range: 28-58) and 60 days (range: 14-230) respectively ( both P<0.01 compared to the pts that received grafts with KIR ligand incompatibility). Conclusion: Transplantation of haplo-identical CD34+ cells with a single UCB unit in neutropenic pts with SAA and SAA evolved to MDS was associated with rapid neutrophil recovery, durable donor engraftment and excellent long-term survival. These results suggest that haplo-cord HSCT is an effective treatment option associated with excellent survival in pts with SAA who lack an HLA-matched donor.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal