Abstract
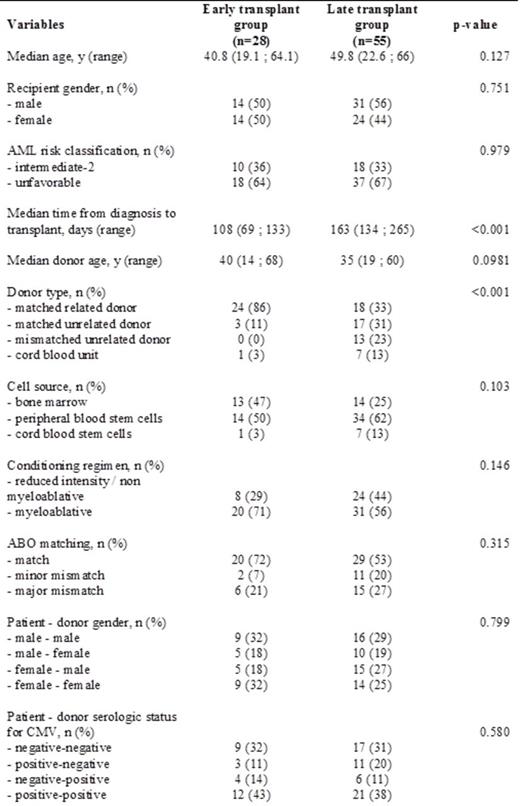
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is the main therapeutic option for most patients with high risk acute myeloid leukemia (AML). In order to determine whether time between diagnosis and allo-HSCT could have any impact on transplant outcomes, we screened 700 consecutive adult AML patients diagnosed between January 2007 and June 2014 at the Lyon Sud Hospital transplant center. Inclusion criteria were: (1) newly diagnosed AML in patients with age ≤ 65 years, (2) AML classified in the intermediate-2 and unfavorable risk groups according to the Acute Leukemia French Association (3) patients fit for receiving chemotherapy (4) patients candidates for allo-HSCT and in first complete remission (CR1) at transplantation. Two hundred and one patients met the inclusion criteria and were enrolled in the study. Among them, 137 (68%) received allo-HSCT of whom 83 (41%) only received HSCT in CR1 after a median time of 143 days (range: 69-265) from diagnosis. We collected within this interval different delays for donor search, including patients HLA typing and time to unrelated donor identification when a sibling donor was not available. Patients were split into 2 groups based on their time to transplant. An "early transplant group" included 28 (33%) patients transplanted after a median time of 108 days (range: 69-133) after diagnosis. The other 55 (67%) patients transplanted after a median time of 163 days (range: 134-265) were qualified as "late transplant group". Patients and transplantation characteristics according to the timing of transplantation are shown in table 1. After a median follow-up of 16 months (range: 0-60) the 5-year probability of overall survival (OS) and disease-free survival (DFS) for the whole population were respectively, 63.4% and 48.3%. The cumulative incidences of non-relapse mortality (NRM) at 1 and 5 years were constant at 17.5%. The multivariate analysis using proportional hazards modeling showed that conditioning regimen and sex mismatching were independent prognostic factors for DFS, with no significant impact on OS. To evaluate the long term impact of transplantation timing on OS and DFS, we performed a landmark analysis for patients surviving at 1 year post-allo-HSCT. This analysis showed that patients in the early transplant group had a higher probability of OS at 3 and 5 years with 100% survival respectively compared to the late transplantation group with 85.5% and 79.4% respectively (p=0.09); accordingly, we found a significant difference in terms of DFS with 100% probability at 3 and 5 years for the early transplantation group compared to 80% and 56% respectively in the late transplantation group (p=0.02). This difference in terms of OS and PFS was still valid after stratification on the type of conditioning regimen.
These results confirm the important impact of allogeneic HSCT timing in high-risk AML patients, early allo-HSCT for patients transplanted in CR1 is associated with a better OS and a very significant benefit in terms of DFS. Further analyses are ongoing including disease monitoring from diagnosis to the last follow-up to identify the potential of transplantation timing on the graft versus leukemia effect.
Nicolini:Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Ariad Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal