Abstract
Introduction
Myeloproliferative neoplasms (MPNs) are associated with constitutional symptoms and high levels of circulating inflammatory cytokines. The etiology of this increase in inflammatory cytokines could be secondary to Jak2 mutation resulting in enhanced transduction signaling of cytokines. Toll-like receptors (TLRs) represent another activating mechanism by which their expression on antigen presenting cells, such as dendritic cells (DCs) and macrophages, serve as key pattern recognition receptors (PRR) which play a central role in induction of innate and adaptive immune responses resulting in the signaling of inflammatory cytokines. TNFα is one of the inflammatory cytokine which is significantly raised in MPN patients. Recent evidence suggests that TNFα may facilitate clonal expansion of JAK2 V617F mutation positive cells which leads to hypothesis suggesting that chronic inflammation is involved in the pathogenesis and clonal evolution in Philadelphia-negative chronic MPNs. Therefore, we investigated the role of TLRs and related cytokines in MPNs and we found that only TLR-2 was significantly elevated in MPNs. We further used the TLR-2 ligand, Pam3CSK4, to study its effects on the production inflammatory cytokines.
Materials & Methods
TLR assay: TLR-2, 4, 7, 9 quantification was performed by TLR staining of 5×105 mononuclear cells which were incubated with 5 μg/mlof conjugated TLR-2, 4, 7, 9 antibody and assayed by flow cytometry.
Monocyte-derived dendritic cells (mdDC) and Inflammatory Cytokines.
mdDC were generated from isolated monocytes (anti-CD14-coated magnetic beads) then by incubation with IL-4 and GM-CSF for 4 days. Immature mdDC (1×104/well) were either left untreated or stimulated with Pam3CSK4, in 96 well plates. After 48h, cells were incubated with 20% human AB serum in PBS containing 0.1% BSA and 0.1% NaN3 for 20 min at 4¡C. Thereafter, cells were stained with fluorescence-labeled mAb specific to CD80, CD83, (BD Biosciences). Cytokine levels were determined in supernatants harvested after 48h using the MSD (Meso Scale Discovery) System.
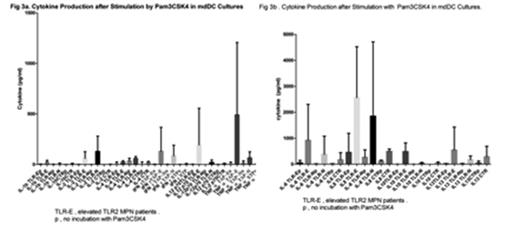
Results. Levels ofTLR-2 were significantly elevated in patients with MPNs especially in those with polycythemia vera and essential thrombocythemia, but only marginally elevated in myelofibrosis (MF) patients, which likely may be attributable to the relatively lack in number of MF patients (Fig 1). In all patient subsets, TLR 4, 7, 9 levels were not significantly different from controls as shown in Fig 1. Fig 2 shows maturation of mdDC by TLR-2 ligand, Pam3CSK4. Higher numbers of CD83+ cells were generated more from patients with elevated TLR levels, confirming these MPN patients has elevated TLR2 levels to be able to generated more dendric cells by TLR-2 ligand. Fig 3 a and b shows in elevated TLR-2 level MPN patients, Pam3CSK4 stimulated more cytokins of IFNγ, IL12p70, TNFα, IL6, IL8, IL10, IL13. Fig 4 showed in elevated TLR-2 levels MPN patients have more of IL8, TNFα, IL13, IL6, in the plasma, consistent with inflammatory cytokines likely from elevated elevated TLR-2.Therefore TLR-2 likely plays a very important role in the inflammatory cytokine production in MPN diseases.
Conclusion. TLR-2 and not TLR-4, 7, 9 were found to be significantly elevated in MPNs. Stimulation of the TLR-2 ligand promoted the generation of more mature DCs in TLR-2 elevated MPN patients, demonstrating TLR-2 were elevated in these patients. Further, the stimulation of mdDC cultures with TLR2 ligand led to greater cytokine production and the level of plasma cytokines correlated with TLR-2 levels. We conclude that TLR-2 is important in the production of inflammatory cytokines in MPNs and it may play a significant role in the pathogenesis of MPNs.
Wang:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal