Abstract
Introduction: Older age, poor performance status, diminished organ function and adverse genetic features are poor prognostic factors in treatment of ALL. Our goal is to develop prognostic models predicting complete response (CR), death in CR, 2-month mortality and survival in adult pts with ALL, which would be used to assist pts and oncologists to establish expectations with intensive chemotherapy.
Methods: A total of 434 pts with ALL treated with intensive chemotherapy between 2000 and 2015 were analyzed. Frontline treatments included hyperCVAD alone (n=152) or in combination with rituximab (n=156) [Thomas D, et.al, JCO 2010], or ofatumumab (n=34), and Augmented-BFM (n=92) [Rytting ME, et al Cancer 2014]. Following clinical features were analyzed; age, gender, diagnosis (B or T-ALL), performance status (Zubrod), prior malignancy, prior chemotherapy, white blood cell count, platelet count, hemoglobin level, peripheral blood (PB) blast, bone marrow (BM) blast, mixed lineage leukemia (MLL) gene rearrangements, albumin level, total bilirubin level, estimated glomerular filtration rate (GFR by the Modification of Diet in Renal Disease Study equation) and chemotherapy type. Univariate and multivariate analyses of clinical features associated with CR, death in CR, 2-month mortality and survival were performed.
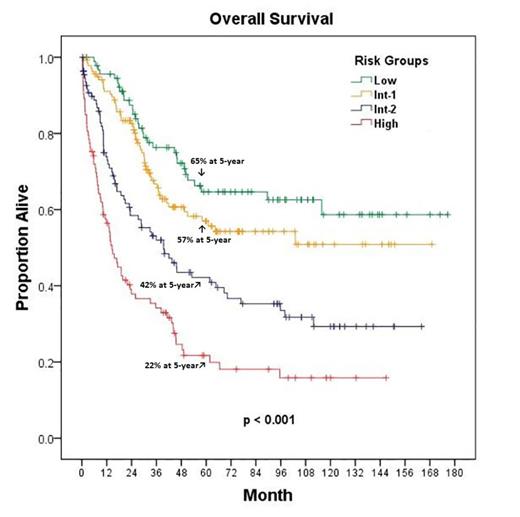
Results: Pts characteristics are summarized in Table 1. The overall CR rate, death in CR rate, 2-month mortality rate, 1-year and 5-year survival rates were 94%, 15%, 8%, 80%, and 47%, respectively. In multivariate analysis, we identified prognostic factors associated with CR, death in CR, 2-month mortality, and survival (Table 2). Age > 40 years, performance status ≥ 2, total bilirubin >1 mg/dL, GFR < 60 mL/min/1.73m2, albumin < 3.5 g/dL, WBC > 50 x109/L and presence of MLL gene rearrangements were identified as independent adverse prognostic features for overall survival (OS). Because all predictive features identified had similar statistical impact, patients were divided into four different risk categories: 1) low (no adverse feature) 92 pts (21%), 2) intermediate-1 (1 adverse feature) 138 pts (32%), 3) intermediate-2 (2 adverse features) 111 pts (26%), and 4) high (≥ 3 adverse features) 93 pts (21%). Median OS survival was not reached in low and intermediate-1 categories, and it was 40 and 15 months for intermediate-2 and high risk categories respectively (p<0.001). The 5-year survival rates were 65%, 57%, 42%, and 22%, respectively (Figure 1).
Conclusion: Prognostic model predicting survival in adult ALL pts were developed based on standard readily available baseline clinical features, which may assist in therapeutic and investigational decisions. This prognostic model is based on retrospective analysis, and further validation is needed in independent study groups.
Characteristics of the Study Group (n=434)
| Parameter . | Category . | No. (%) . |
|---|---|---|
| Age > 40 years old | yes | 207 (48) |
| no | 227 (52) | |
| Sex | female | 198 (46) |
| male | 236 (54) | |
| Diagnosis | Pre-B | 419 (97) |
| Pre-T | 15 (3) | |
| Prior Malignancy | yes | 46 (11) |
| no | 388 (89) | |
| Prior Chemotherapy | yes | 31 (7) |
| no | 403 (93) | |
| Prior Radiotherapy | yes | 21 (5) |
| no | 413 (95) | |
| Performance Status ≥ 2 | yes | 69 (16) |
| no | 365 (84) | |
| MLL Gene Rearrangement | yes | 34 (8) |
| no | 400 (92) | |
| WBC, x109/L | ≤ 50 | 389 (90) |
| > 50 | 45 (10) | |
| Platelet, x109/L | < 100 | 93 (21) |
| ≥ 100 | 341 (79) | |
| Hg, gr/dl | < 8 | 144 (33) |
| ≥ 8 | 290 (67) | |
| PB Blast | yes | 337 (78) |
| no | 97 (22) | |
| BM Blast, % | ≥ 50 | 388 (89) |
| <50 | 46 (11) | |
| Albumin, gr/dl | < 3.5 | 213 (49) |
| ≥ 3.5 | 221 (51) | |
| Total Bilirubin, mg/dl | > 1 | 53 (12) |
| ≤ 1 | 381 (88) | |
| GFR, ml/min/1.73m2 | < 60 | 45 (10) |
| ≥ 60 | 389 (90) | |
| Chemotherapy | HCVAD | 152 (35) |
| HCVAD + Rituximab | 156 (36) | |
| HCVAD + Ofatumumab | 34 (8) | |
| AUG-BFM | 92 (21) |
| Parameter . | Category . | No. (%) . |
|---|---|---|
| Age > 40 years old | yes | 207 (48) |
| no | 227 (52) | |
| Sex | female | 198 (46) |
| male | 236 (54) | |
| Diagnosis | Pre-B | 419 (97) |
| Pre-T | 15 (3) | |
| Prior Malignancy | yes | 46 (11) |
| no | 388 (89) | |
| Prior Chemotherapy | yes | 31 (7) |
| no | 403 (93) | |
| Prior Radiotherapy | yes | 21 (5) |
| no | 413 (95) | |
| Performance Status ≥ 2 | yes | 69 (16) |
| no | 365 (84) | |
| MLL Gene Rearrangement | yes | 34 (8) |
| no | 400 (92) | |
| WBC, x109/L | ≤ 50 | 389 (90) |
| > 50 | 45 (10) | |
| Platelet, x109/L | < 100 | 93 (21) |
| ≥ 100 | 341 (79) | |
| Hg, gr/dl | < 8 | 144 (33) |
| ≥ 8 | 290 (67) | |
| PB Blast | yes | 337 (78) |
| no | 97 (22) | |
| BM Blast, % | ≥ 50 | 388 (89) |
| <50 | 46 (11) | |
| Albumin, gr/dl | < 3.5 | 213 (49) |
| ≥ 3.5 | 221 (51) | |
| Total Bilirubin, mg/dl | > 1 | 53 (12) |
| ≤ 1 | 381 (88) | |
| GFR, ml/min/1.73m2 | < 60 | 45 (10) |
| ≥ 60 | 389 (90) | |
| Chemotherapy | HCVAD | 152 (35) |
| HCVAD + Rituximab | 156 (36) | |
| HCVAD + Ofatumumab | 34 (8) | |
| AUG-BFM | 92 (21) |
Multivariate Analysis of Adverse Factors Associated with the Clinical Outcomes
| Outcome . | Factor . | p . | O.R. . | C.I. . |
|---|---|---|---|---|
| Death in CR | Age > 40 years old | 0.004 | 3.0 | 1.4-6.3 |
| 2-Month Mortality | Total Bilirubin > 1 mg/dl | 0.018 | 3.0 | 1.2-6.0 |
| Albumin < 3.5 gr/dl | 0.023 | 2.6 | 1.1-6.0 | |
| GFR < 60 ml/min/1.73m2 | 0.009 | 3.2 | 1.3-7.6 | |
| Complete Response | GFR < 60 ml/min/1.73m2 | 0.001 | 0.2 | 0.1-0.5 |
| Overall Survival | Age > 40 years old | 0.002 | 0.6 | 0.5-0.8 |
| Performance Status ≥ 2 | <0.001 | 0.5 | 0.4-0.7 | |
| Total Bilirubin > 1 mg/dl | 0.029 | 0.7 | 0.4-0.9 | |
| GFR < 60 ml/min/1.73m2 | 0.003 | 0.6 | 0.4-0.8 | |
| Albumin < 3.5 gr/dl | 0.045 | 0.8 | 0.6-0.9 | |
| WBC > 50 x109/L | 0.030 | 0.6 | 0.4-0.9 | |
| MLL Gene Rearrangement | 0.032 | 0.6 | 0.4-0.9 |
| Outcome . | Factor . | p . | O.R. . | C.I. . |
|---|---|---|---|---|
| Death in CR | Age > 40 years old | 0.004 | 3.0 | 1.4-6.3 |
| 2-Month Mortality | Total Bilirubin > 1 mg/dl | 0.018 | 3.0 | 1.2-6.0 |
| Albumin < 3.5 gr/dl | 0.023 | 2.6 | 1.1-6.0 | |
| GFR < 60 ml/min/1.73m2 | 0.009 | 3.2 | 1.3-7.6 | |
| Complete Response | GFR < 60 ml/min/1.73m2 | 0.001 | 0.2 | 0.1-0.5 |
| Overall Survival | Age > 40 years old | 0.002 | 0.6 | 0.5-0.8 |
| Performance Status ≥ 2 | <0.001 | 0.5 | 0.4-0.7 | |
| Total Bilirubin > 1 mg/dl | 0.029 | 0.7 | 0.4-0.9 | |
| GFR < 60 ml/min/1.73m2 | 0.003 | 0.6 | 0.4-0.8 | |
| Albumin < 3.5 gr/dl | 0.045 | 0.8 | 0.6-0.9 | |
| WBC > 50 x109/L | 0.030 | 0.6 | 0.4-0.9 | |
| MLL Gene Rearrangement | 0.032 | 0.6 | 0.4-0.9 |
Konopleva:Novartis: Research Funding; AbbVie: Research Funding; Stemline: Research Funding; Calithera: Research Funding; Threshold: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal