Abstract
Introduction: Prognosis of adult patients with Acute Lymphoblastic Leukemia (ALL) has improved in the last decades. Improvement of response rates with new innovative therapies in relapsed patients was associated with better outcome. In the present study we evaluate the impact of CR1 duration on long-term outcome of patients with relapsed disease.
Methods: Patients with relapsed Philadelphia negative pre-B ALL initially treated at our institution between 2000 and 2014 were reviewed. Information regarding treatment, baseline characteristics, response to therapy and duration of remission was evaluated. Survival outcomes were analyzed in terms of response to induction chemotherapy and duration of CR1. Statistical analysis included Chi-squared for categorical variables, T-student for continuous variables and Kaplan-Meier for OS.
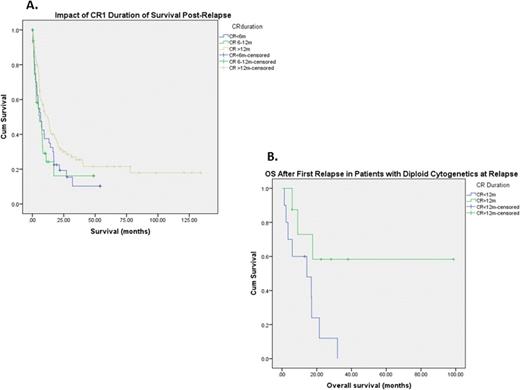
Results: A total of 166 patients were analyzed. Patient characteristics are summarized in Table 1. Overall response rate to initial therapy was 94% (including 91% CR rate); 10 (6%) patients had primary induction failure. Median time to relapse was 25 months. Patients were grouped into three categories according to duration of CR1: 1) Patients with CR1 duration of less than 6 months, 2) CR1of 6-12 months, and 3) CR1 duration greater than 12 months. Among baseline characteristics, younger age was associated with a CR duration of more than 12 months (34y vs 44y and 46y, p=0.01). No significant differences were observed in terms of baseline hemoglobin, white blood cell count, platelet count, blasts, and LDH between these groups. Median survival after relapse was significantly longer in patients with a CR duration of more than 12 months compared to those with 6-12 months or less than 6 months remission duration (12 months vs 6 months vs 5 months respectively, p=0.04) (Figure 1A). Information regarding salvage therapy was available in 79 patients and is summarized in Table 1. Cytogenetic abnormalities at the time of relapse were available in 39 patients and predicted for survival. Presence of a diploid karyotype was associated with longer survival than patients with hypodiploid, hyperdiploid or complex karyotypes (17, 4, 8 and 2 months respectively, p<0.001). Additionally, amongst those patients with diploid cytogenetics at relapse, median survival was significantly longer in those with CR1 duration greater than 12 months (not reached at 98 months of follow-up vs 14 months respectively, p=0.03) compared to those with CR1 duration of less than 12 months. (Figure 1B). In patients with diploid cytogenetics, CR1 duration did not predict for a higher CR rate to salvage therapy (p=0.37).
Conclusions: Duration of CR1 in patients with pre-B ALL predicts survival after first relapse. Furthermore, Patients with diploid cytogenetics and CR1 of more than 12 months have the best outcome post frontline therapy failure.
| Studied factor . | N (%) [range] . |
|---|---|
| Age | 40 (16-86) |
| Sex | |
| Male | 96 (58) |
| Female | 70 (42) |
| Treatment at Baseline | |
| HCVAD-R | 69 (42) |
| HCVAD | 56 (34) |
| Augmented BFM | 41 (25) |
| Treatment at Relapse | |
| HCVAD based | 33 (42) |
| Monoclonal antibodies | 24 (30) |
| FLAG-ida | 5 (6) |
| Investigational | 11 (14) |
| Asparaginase based therapy | 6 (8) |
| Mean blood counts at baseline | |
| Hemoglobin | 8.9g/dL [3.6-15] |
| Platelets | 59 x109 /L [0-393] |
| WBC | 34 x109 /L [0.6-602] |
| Karyotype at Relapse | |
| Diploid | 18 (46) |
| Hipodiploid | 3 (8) |
| Complex | 12 (31) |
| Hiperdiploid | 6 (15) |
| Baseline peripheral Blast % | 40 [0-100] |
| LDH (UI/dL) | 2225 [172-28261] |
| Bone Marrow Blast % | 81 [0-100] |
| Induction Failure | 10 (6) |
| Duration of CR1 | |
| <6 months | 41 (2 |
| 6-12 months | 34 (20) |
| >12 months | 91 (55) |
| Studied factor . | N (%) [range] . |
|---|---|
| Age | 40 (16-86) |
| Sex | |
| Male | 96 (58) |
| Female | 70 (42) |
| Treatment at Baseline | |
| HCVAD-R | 69 (42) |
| HCVAD | 56 (34) |
| Augmented BFM | 41 (25) |
| Treatment at Relapse | |
| HCVAD based | 33 (42) |
| Monoclonal antibodies | 24 (30) |
| FLAG-ida | 5 (6) |
| Investigational | 11 (14) |
| Asparaginase based therapy | 6 (8) |
| Mean blood counts at baseline | |
| Hemoglobin | 8.9g/dL [3.6-15] |
| Platelets | 59 x109 /L [0-393] |
| WBC | 34 x109 /L [0.6-602] |
| Karyotype at Relapse | |
| Diploid | 18 (46) |
| Hipodiploid | 3 (8) |
| Complex | 12 (31) |
| Hiperdiploid | 6 (15) |
| Baseline peripheral Blast % | 40 [0-100] |
| LDH (UI/dL) | 2225 [172-28261] |
| Bone Marrow Blast % | 81 [0-100] |
| Induction Failure | 10 (6) |
| Duration of CR1 | |
| <6 months | 41 (2 |
| 6-12 months | 34 (20) |
| >12 months | 91 (55) |
Cortes:Pfizer: Consultancy, Research Funding; Teva: Research Funding; BMS: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; BerGenBio AS: Research Funding; Ariad: Consultancy, Research Funding; Astellas: Consultancy, Research Funding; Ambit: Consultancy, Research Funding; Arog: Research Funding; Celator: Research Funding; Jenssen: Consultancy. Pemmaraju:Stemline: Research Funding; Incyte: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding; LFB: Consultancy, Honoraria. Konopleva:Novartis: Research Funding; AbbVie: Research Funding; Stemline: Research Funding; Calithera: Research Funding; Threshold: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal